INTRODUCTION
Early term delivery, defined as term delivery at 37–38 weeks of gestation, has been reported to be associated with the risk of neonatal morbidity, and this relationship has also been demonstrated in cases with elective cesarean delivery (CD).
12345 According to these evidences, it has been recommended to postpone elective CD until late term (39 weeks of gestation or later).
6
Planning the date of elective CD in the late term period may increase the risk of emergent CD, which could be a risk factor for maternal/neonatal morbidity. Nevertheless, most studies of adverse neonatal outcomes and the timing of CDs are based on elective CDs after excluding cases with emergent CD.
2789
To address this issue, we assessed the risk of emergent CD prior to the planned delivery date and adverse neonatal/maternal outcomes according to the planned gestational age at delivery (GAD) for elective CD.
Go to :

METHODS
Study design
The study population consisted of consecutive term pregnant women who were booked for elective CD and were subsequently delivered at term (gestational age at or after 37 weeks) in Seoul National University Hospital between January 2003 and February 2011. In this study period when the conception of early term deliveries has not been universally implemented, the delivery timing was decided at the discretion of the attending obstetrician based on the mother's preference. Cases in which a trial of labor was undertaken prior to CD, cases in which the elective dating of CD was not completed, cases of fetal anomaly or fetal death in utero, cases with maternal disease that could affect the fetal outcome (hypertensive disease in pregnancy, gestational diabetes requiring insulin therapy, overt diabetes, history of maternal cardiac/renal/connective tissues disease, human immunodeficiency virus [HIV] infection, clinical chorioamnionitis prior to delivery, active rhesus or other blood type antagonism, and maternal infectious disease such as toxoplasmosis, syphilis, rubella, cytomegalovirus, or herpes), or cases with an obstetric condition that could affect the fetal outcome (non-reassuring fetal status, placenta previa, placenta accreta, placental abruption, nonvertex presentation with unsuccessful version) were excluded.
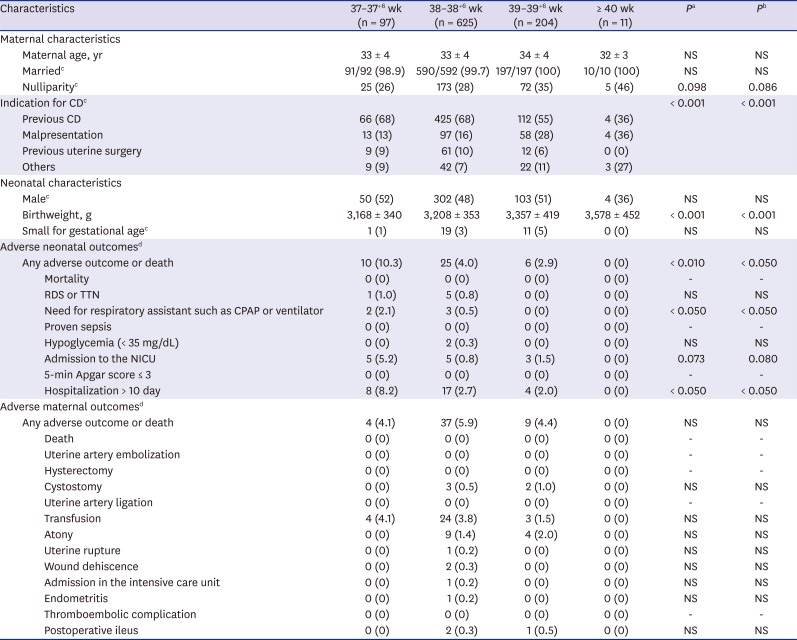
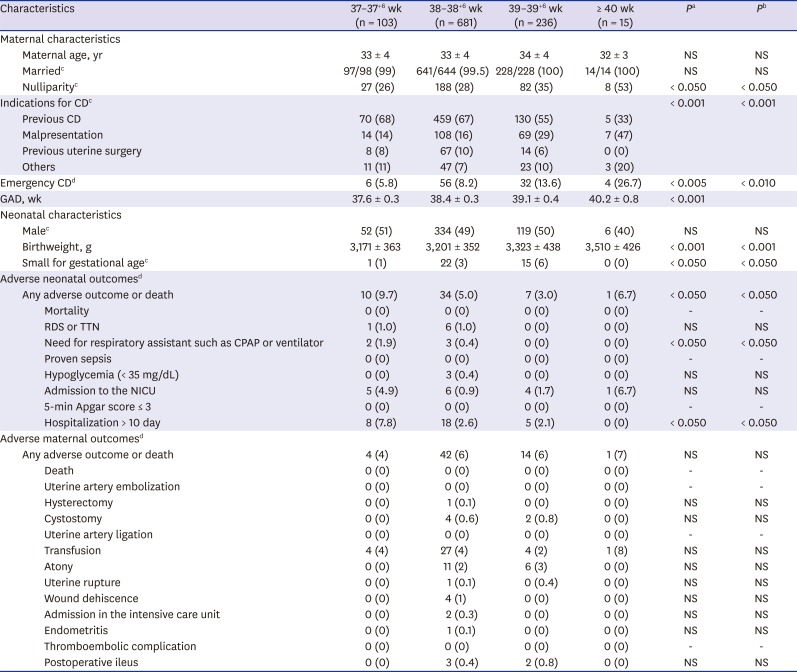
The relationship between the planned GAD for elective CD (planned GAD), the rate of emergent CD due to labor/ruptured membranes prior to the planned delivery date, and the risk of adverse neonatal/maternal outcomes were determined in the study population.
Adverse neonatal and maternal outcomes
Adverse neonatal outcomes were defined as the presence of neonatal mortality, adverse respiratory outcomes (respiratory distress syndrome, transient tachypnea of newborn, or need for respiratory assistant such as continuous positive airway pressure or ventilator), proven congenital sepsis, hypoglycemia, seizures, necrotizing enterocolitis, hypoxic ischemic encephalopathy, cardiopulmonary resuscitation, 5-minute Apgar Score ≤ 3, admission to the neonatal intensive care unit (NICU), or prolonged hospitalization for more than 10 days. The criteria for adverse neonatal outcomes were adapted from the criteria of Tita et al.
2 and Ghartey et al.
1 with modification.
Adverse maternal outcomes included a primary composite of death, uterine atony, need for transfusion, uterine artery embolization, peripartum hysterectomy, cystostomy, broad ligament hematoma, uterine artery ligation, uterine rupture, wound dehiscence, admission to the intensive care unit, endometritis, thromboembolic complications, or postoperative ileus. The criteria for adverse maternal outcomes were adapted from the criteria of Tita et al.
10 with modification.
Statistical analysis
Proportions were compared with Fisher's exact test, and comparisons of continuous variables between groups were performed with a Mann-Whitney U test or Kruskal-Wallis analysis of variance as appropriate. Logistic regression analysis was conducted for multivariate analysis. P values < 0.05 were considered significant.
Ethics statement
The Institutional Review Board of the Seoul National University Hospital approved the study, and we followed the ethical standards for human experimentation established in the Declaration of Helsinki.
Go to :

DISCUSSION
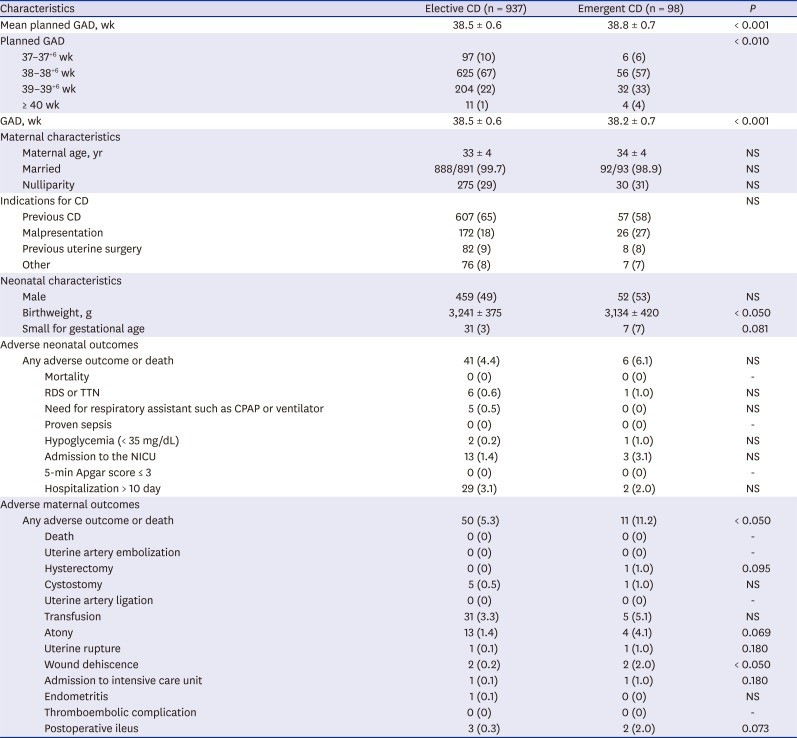
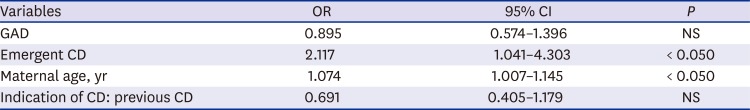
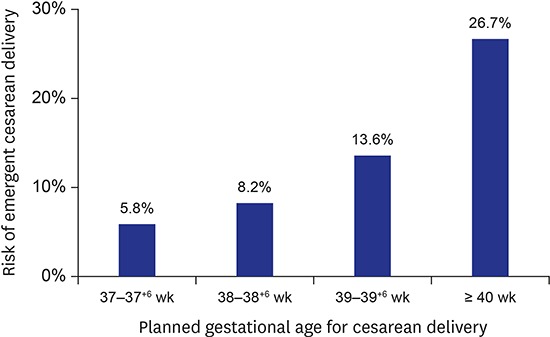
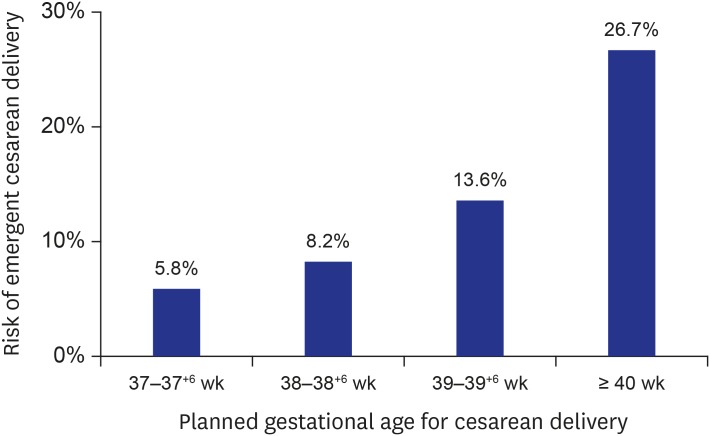
The main findings of the current study were: 1) the risk of emergent operation increased significantly with increasing planned GAD for elective CD; 2) the risk of adverse maternal outcomes was greater in cases of emergent CD compared to elective CD, whereas the risk of adverse neonatal outcomes did not differ; 3) in the total study population including both cases with elective and emergency operation, the risk of adverse maternal outcomes did not increase according to the planned GAD, and the risk of adverse neonatal outcomes decreased significantly according to the planned GAD.
To our knowledge, this is the first study which assessed the risk of emergency CDs and adverse neonatal/maternal outcomes according to the planned GAD for elective CDs. Indeed, most studies of adverse neonatal or maternal outcomes and the timing of CDs are based on elective CDs after excluding cases with emergent CD.
Previous studies have indicated that the risk of adverse neonatal outcomes in elective term CDs decreases progressively with increasing gestational age at birth.
278911 According to this evidence, performing elective CD prior to 39 weeks of gestation is discouraged. However, delaying delivery until 39 weeks may increase the risk of emergent CDs, and the outcome of this particular group has not been adequately addressed in the literature.
12 In the current study, we examined the frequency and risk among this group undergoing emergent delivery with regards to both neonatal and maternal outcomes. As a result, the risk of emergency operation was increased in cases according to advance planned GAD, and maternal morbidity was higher in cases with emergency CD. However, the total risk of adverse maternal outcomes did not increase according to the advance planned GAD, when including both cases with elective and emergent CD, and the total risk of adverse neonatal outcomes decreased significantly according to the advanced planned GAD.
In the literature, the impacts of emergent CD on adverse neonatal outcomes in patients who are candidates for elective CDs are controversial. Neonatal respiratory morbidity has been shown to decrease in cases of emergent CD after the onset of labor,
31314 although other studies have failed to demonstrate this relationship.
1115 In addition, the onset of labor in cases among women who have undergone previous cesarean is associated with lower cord pH, neonatal sepsis, iatrogenic fetal injury, uterine rupture, and intrapartum fetal death.
131416 In the current study, the risk of adverse neonatal outcomes was not increased among emergent CDs.
Until now, few studies have addressed maternal morbidity according to the GAD.
17 In elective CD, maternal morbidity does not appear to be affected by the GAD.
10 In terms of emergency CD, the risk of onset of labor before 39 weeks was 10%–25%,
39 and concerns about an increased risk of maternal mortality and morbidity, such as excessive blood loss, uterine rupture and infections in intrapartum CD, compared to elective CD have also been suggested in emergency operation.
9121819202122 In the current study, the risk of emergent CD increased significantly with increasing planned GAD, and maternal morbidity was greater in cases of emergent CD. In multiple logistic regression analysis, emergent CD remained a risk factor for adverse maternal morbidity even after adjustment for GAD. However, only the risk of wound dehiscence was increased in emergency CD than in elective CD in the current study, whereas the risk of severe maternal, such as excessive blood loss, uterine rupture and endometritis was not significantly increased. Moreover, when including both cases with elective and emergency operation, the maternal morbidity was not increased according to the planned GAD.
The results of the current study may be used for the counseling women regarding the planning of the gestational age at elective CD. Planning of elective CD at 39 weeks or later is encouraged to decrease the risk of neonatal respiratory morbidity; however it carries the higher risk of emergent CD, which can result in maternal, though not neonatal, morbidity. In addition, emergent CD carries the risk of lower medical service qualities in terms of operating facilities and health professionals, especially in resource-constrained countries.
23 However, as a total (when including both cases with elective and emergency operation), the maternal morbidity was not increased according to the planned GAD. And the neonatal morbidity was decreased according to planned gestational age, as a total.
The limitation of the current study is the nature of the current study which is retrospective study; further prospective randomized trials may be needed to compare the risk and benefit according to the timing of elective CD.
Further studies may be needed to evaluate the risk of other adverse outcomes and the planned gestational age for CD. In the current study, we excluded cases of fetal death in utero, cases with maternal disease such as hypertensive disease in pregnancy or clinical chorioamnionitis prior to delivery, and cases with a non-reassuring fetal status or placental abruption; all of these may develop while awaiting elective delivery at 39 weeks or later.
2425 Therefore, the risk versus benefit of postponing elective CD until 39 weeks of gestation also needs to be evaluated with regards to these complications.
No prospective randomized trials have been conducted to compare the risk and benefit between the timing of elective CD before and after 39 weeks of gestation.
12 From the results of the current study and previous retrospective studies, we may postulate that neonatal respiratory morbidities may be lower but maternal morbidities may be similar in the strategies of timing of elective CD after 39 weeks of gestation. Additionally, other neonatal morbidities such as perinatal mortality should be evaluated. The determination of optimal delivery timing for elective CD is very important issue, considering that the CD rate is about 20%–40% in various countries and 35% in Korea.
26
In conclusion, the risk of emergent CD increased with increasing planned gestational age for elective CD, and the risk of adverse maternal outcomes was higher with emergent CD. However, the risk of adverse maternal outcomes did not increase according to the planned gestational age in the total study population including both cases with elective and emergency CD.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download