1. Kivimäki M, Shipley MJ, Ferrie JE, Singh-Manoux A, Batty GD, Chandola T, et al. Best-practice interventions to reduce socioeconomic inequalities of coronary heart disease mortality in UK: a prospective occupational cohort study. Lancet. 2008; 372(9650):1648–1654.

2. Khang YH, Lynch JW, Jung-Choi K, Cho HJ. Explaining age-specific inequalities in mortality from all causes, cardiovascular disease and ischaemic heart disease among South Korean male public servants: relative and absolute perspectives. Heart. 2008; 94(1):75–82.

3. Khang YH, Lynch JW, Yang S, Harper S, Yun SC, Jung-Choi K, et al. The contribution of material, psychosocial, and behavioral factors in explaining educational and occupational mortality inequalities in a nationally representative sample of South Koreans: relative and absolute perspectives. Soc Sci Med. 2009; 68(5):858–866.

4. Khang YH, Yun SC, Cho HJ, Jung-Choi K. The impact of governmental antismoking policy on socioeconomic disparities in cigarette smoking in South Korea. Nicotine Tob Res. 2009; 11(3):262–269.

5. Park EJ, Kim H, Kawachi I, Kim IH, Cho SI. Area deprivation, individual socioeconomic position and smoking among women in South Korea. Tob Control. 2010; 19(5):383–390.

6. Cho HJ, Song YM, Smith GD, Ebrahim S. Trends in socio-economic differentials in cigarette smoking behaviour between 1990 and 1998: a large prospective study in Korean men. Public Health. 2004; 118(8):553–558.

7. Choi S, Kim Y, Park S, Lee J, Oh K. Trends in cigarette smoking among adolescents and adults in South Korea. Epidemiol Health. 2014; 36:e2014023.
8. Yun WJ, Rhee JA, Kim SA, Kweon SS, Lee YH, Ryu SY, et al. Household and area income levels are associated with smoking status in the Korean adult population. BMC Public Health. 2015; 15:39.

9. Khang YH, Cho HJ. Socioeconomic inequality in cigarette smoking: trends by gender, age, and socioeconomic position in South Korea, 1989–2003. Prev Med. 2006; 42(6):415–422.

10. Ministry of Health and Welfare (KR). Health Plan 2010. Seoul, Korea: Ministry of Health and Welfare;2005.
11. Ministry of Health and Welfare (KR). Health Plan 2020 (2011–2015). Seoul, Korea: Ministry of Health and Welfare;2011.
12. Ministry of Health and Welfare (KR). Health Plan 2020 (2016–2020). Cheongju, Korea: Ministry of Health and Welfare;2015.
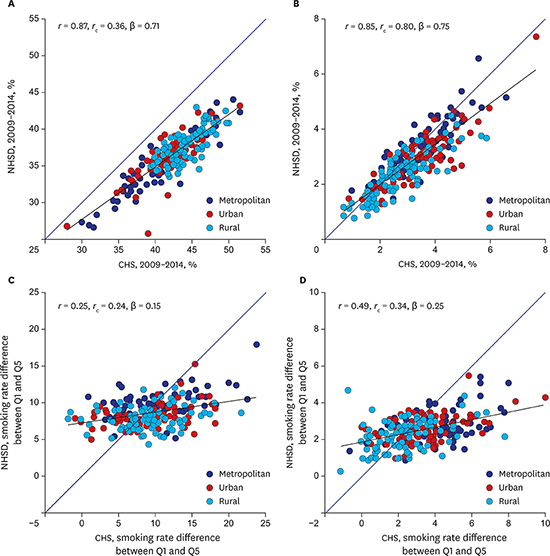
13. Kim I, Bahk J, Yoon TH, Yun SC, Khang YH. Income differences in smoking prevalences in 245 districts of South Korea: patterns by area deprivation and urbanity, 2008–2014. J Prev Med Public Health. 2017; 50(2):100–126.

14. Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46(3):799–800.
15. Khang YH, Yun SC, Bahk J, Kang HY, Kim I, Seo S, et al. Developing Indicators for Evaluating and Monitoring the Health Plan 2020 Using the National Health Information Database of the National Health Insurance Service in Korea. Wonju, Korea: National Health Insurance Service;2016.
16. Khang YH, Bahk J, Yi N, Yun SC. Age- and cause-specific contributions to income difference in life expectancy at birth: findings from nationally representative data on one million South Koreans. Eur J Public Health. 2016; 26(2):242–248.

17. Khang YH, Yang S, Cho HJ, Jung-Choi K, Yun SC. Decomposition of socio-economic differences in life expectancy at birth by age and cause of death among 4 million South Korean public servants and their dependents. Int J Epidemiol. 2010; 39(6):1656–1666.

18. Zhou B, Bentham J, Di Cesare M, Bixby H, Danaei G, Cowan MJ, et al. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017; 389(10064):37–55.
19. Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health (Oxf). 2005; 27(3):281–291.









 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download