1. Reese AC, Cooperberg MR, Carroll PR. Minimal impact of clinical stage on prostate cancer prognosis among contemporary patients with clinically localized disease. J Urol. 2010; 184(1):114–119.

2. Eastham J. Prostate cancer screening. Investig Clin Urol. 2017; 58(4):217–219.

3. Park J, Suh B, Shin DW, Hong JH, Ahn H. Cause of death in Korean men with prostate cancer: an analysis of time trends in a nationwide cohort. J Korean Med Sci. 2016; 31(11):1802–1807.

4. Rodrigues G, Warde P, Pickles T, Crook J, Brundage M, Souhami L, et al. Pre-treatment risk stratification of prostate cancer patients: a critical review. Can Urol Assoc J. 2012; 6(2):121–127.

5. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998; 280(11):969–974.
6. Mohler JL. The 2010 NCCN clinical practice guidelines in oncology on prostate cancer. J Natl Compr Canc Netw. 2010; 8(2):145.

7. Zumsteg ZS, Spratt DE, Pei I, Zhang Z, Yamada Y, Kollmeier M, et al. A new risk classification system for therapeutic decision making with intermediate-risk prostate cancer patients undergoing dose-escalated external-beam radiation therapy. Eur Urol. 2013; 64(6):895–902.

8. Grossfeld GD, Latini DM, Lubeck DP, Broering JM, Li YP, Mehta SS, et al. Predicting disease recurrence in intermediate and high-risk patients undergoing radical prostatectomy using percent positive biopsies: results from CaPSURE. Urology. 2002; 59(4):560–565.

9. Morris WJ, Keyes M, Palma D, Spadinger I, McKenzie MR, Agranovich A, et al. Population-based study of biochemical and survival outcomes after permanent 125I brachytherapy for low- and intermediate-risk prostate cancer. Urology. 2009; 73(4):860–865.
10. Weiner AB, Patel SG, Etzioni R, Eggener SE. National trends in the management of low and intermediate risk prostate cancer in the United States. J Urol. 2015; 193(1):95–102.

11. Abern MR, Aronson WJ, Terris MK, Kane CJ, Presti JC Jr, Amling CL, et al. Delayed radical prostatectomy for intermediate-risk prostate cancer is associated with biochemical recurrence: possible implications for active surveillance from the SEARCH database. Prostate. 2013; 73(4):409–417.

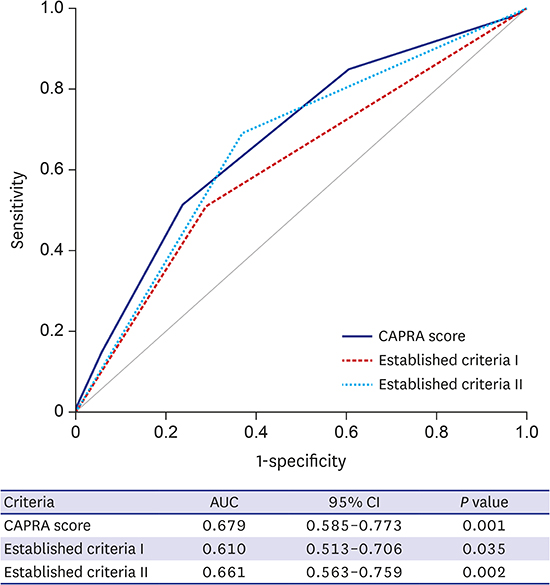
12. Cooperberg MR, Pasta DJ, Elkin EP, Litwin MS, Latini DM, Du Chane J, et al. The University of California, San Francisco Cancer of the Prostate Risk Assessment score: a straightforward and reliable preoperative predictor of disease recurrence after radical prostatectomy. J Urol. 2005; 173(6):1938–1942.

13. Seo WI, Kang PM, Chung JI. Predictive value of the cancer of the prostate risk assessment score for recurrence-free survival after radical prostatectomy in Korea: a single-surgeon series. Korean J Urol. 2014; 55(5):321–326.

14. May M, Knoll N, Siegsmund M, Fahlenkamp D, Vogler H, Hoschke B, et al. Validity of the CAPRA score to predict biochemical recurrence-free survival after radical prostatectomy. Results from a European multicenter survey of 1,296 patients. J Urol. 2007; 178(5):1957–1962.

15. Loeb S, Carvalhal GF, Kan D, Desai A, Catalona WJ. External validation of the cancer of the prostate risk assessment (CAPRA) score in a single-surgeon radical prostatectomy series. Urol Oncol. 2012; 30(5):584–589.

16. Lughezzani G, Budäus L, Isbarn H, Sun M, Perrotte P, Haese A, et al. Head-to-head comparison of the three most commonly used preoperative models for prediction of biochemical recurrence after radical prostatectomy. Eur Urol. 2010; 57(4):562–568.

17. Delouya G, Krishnan V, Bahary JP, Larrivée S, Taussky D. Analysis of the Cancer of the Prostate Risk Assessment to predict for biochemical failure after external beam radiotherapy or prostate seed brachytherapy. Urology. 2014; 84(3):629–633.

18. Cooperberg MR, Freedland SJ, Pasta DJ, Elkin EP, Presti JC Jr, Amling CL, et al. Multiinstitutional validation of the UCSF cancer of the prostate risk assessment for prediction of recurrence after radical prostatectomy. Cancer. 2006; 107(10):2384–2391.

19. Jung JW, Lee JK, Hong SK, Byun SS, Lee SE. Stratification of patients with intermediate-risk prostate cancer. BJU Int. 2015; 115(6):907–912.

20. Lee JY, Diaz RR, Cho KS, Yu HS, Chung JS, Ham WS, et al. Lymphocele after extraperitoneal robot-assisted radical prostatectomy: a propensity score-matching study. Int J Urol. 2013; 20(12):1169–1176.

21. Kattan MW. Nomograms are superior to staging and risk grouping systems for identifying high-risk patients: preoperative application in prostate cancer. Curr Opin Urol. 2003; 13(2):111–116.

22. Kutikov A, Cooperberg MR, Paciorek AT, Uzzo RG, Carroll PR, Boorjian SA. Evaluating prostate cancer mortality and competing risks of death in patients with localized prostate cancer using a comprehensive nomogram. Prostate Cancer Prostatic Dis. 2012; 15(4):374–379.

23. Yossepowitch O, Eggener SE, Bianco FJ Jr, Carver BS, Serio A, Scardino PT, et al. Radical prostatectomy for clinically localized, high risk prostate cancer: critical analysis of risk assessment methods. J Urol. 2007; 178(2):493–499.

24. Freedland SJ, Humphreys EB, Mangold LA, Eisenberger M, Dorey FJ, Walsh PC, et al. Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. JAMA. 2005; 294(4):433–439.

25. Bastian PJ, Boorjian SA, Bossi A, Briganti A, Heidenreich A, Freedland SJ, et al. High-risk prostate cancer: from definition to contemporary management. Eur Urol. 2012; 61(6):1096–1106.

26. San Francisco IF, Werner L, Regan MM, Garnick MB, Bubley G, DeWolf WC. Risk stratification and validation of prostate specific antigen density as independent predictor of progression in men with low risk prostate cancer during active surveillance. J Urol. 2011; 185(2):471–476.

27. Huang J, Vicini FA, Williams SG, Ye H, McGrath S, Ghilezan M, et al. Percentage of positive biopsy cores: a better risk stratification model for prostate cancer? Int J Radiat Oncol Biol Phys. 2012; 83(4):1141–1148.

28. Wattson DA, Chen MH, Moran BJ, Dosoretz DE, Braccioforte MH, Salenius SA, et al. The number of high-risk factors and the risk of prostate cancer-specific mortality after brachytherapy: implications for treatment selection. Int J Radiat Oncol Biol Phys. 2012; 82(5):e773–e779.










 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download