This article has been
cited by other articles in ScienceCentral.
Abstract
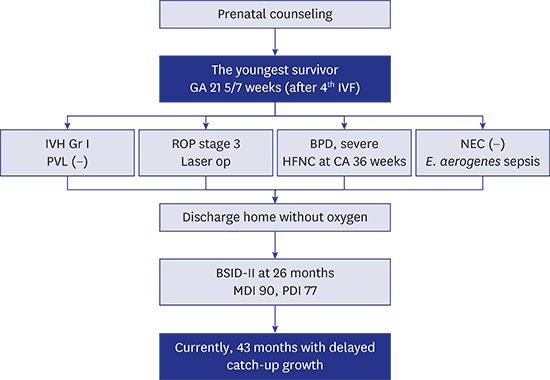
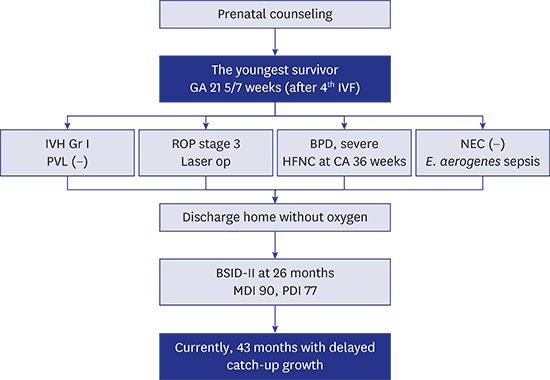
The decision whether or not to resuscitate extremely low gestational age (GA) infants is recommended to be individualized according to antenatal counseling with parents, neonatologists, and obstetricians. A GA of 220/7–236/7 weeks is generally considered as the lower end of the range where infants can be candidates for selective resuscitation. Below this lower end of periviable gestation, resuscitation is usually not considered and survivors are rarely reported. To date, the youngest survivor is an infant with a GA of 216/7 weeks reported in the English medical literature. Here, we report the case of a female infant, the first twin conceived through in vitro fertilization, with a GA of 215/7 weeks, who was resuscitated initially according to strong parental wishes after antenatal counseling and is still surviving at 43 months of age with fairly good neurodevelopmental outcome.
Keywords: Extremely Low Gestational Age Infant, Resuscitation, Case Reports
INTRODUCTION
Periviable gestation is a gestational age (GA) spectrum that includes a high rate of mortality and severe morbidities among survivors at its lower end. Individualized decision-making for each pregnancy/neonate is more influential to the outcome of infants in this gestational period than GA itself. GA 22
0/
7–23
6/
7 weeks is currently considered as the lower end of the periviable gestational range, and these infants might be candidates for selective resuscitation.
1 Below this periviable GA, survivors are rarely reported. There is only one report of a surviving preterm infant at 21
6/
7 weeks GA published in the English literature.
2 We report a case of a preterm infant born at GA 21
5/
7 weeks, the youngest survivor to date, who is still surviving without severe neurodevelopmental impairment at 43 months of age.
The infant was born as the first twin, and the second infant (male), who was born at 450 g and 5/6 Apgar score at 1/5 minutes, expired on day 63 of life due to sepsis. We will describe only the first surviving female twin in this case report.
CASE DESCRIPTION
A female infant, the first twin with a GA of 21
5/
7 weeks, was born at Samsung Medical Center (SMC) in October 2012. The mother was 38 years old and was gravida 1 para 0. She was previously healthy without hypertension, diabetes, or other medical issues except a history of appendectomy received 8 years before delivery. Following several failed experiences of intrauterine insemination and in vitro fertilization (IVF), she got pregnant after 12 years of marriage at her fourth IVF attempt. Prenatal checks were done regularly without specific medical issues. GA was calculated as the interval from the insertion of the fertilized ovum to birth, plus 14 days.
3
At GA 214/7 weeks, due to sudden premature rupture of the membranes, bag bulging and preterm labor, she was emergently transferred to SMC. She received prophylactic antibiotics for premature rupture of the membrane and tocolytics including ritodrine and atosiban, but not magnesium sulfate. There was no evidence of clinically suspected chorioamnionitis and the placental biopsy later confirmed no chorioamnionitis. Prenatal counseling for parents was done with a neonatologist and obstetrician. The parents were extensively informed that attempting resuscitation of an infant with a GA of 21 weeks is extremely rare and the medical team of SMC had no previous experience with such infants, only for several successful cases of GA 223/7 weeks and greater; thus, a good outcome for the infants would be very unlikely. However, the parents strongly and persistently wanted full resuscitation and all efforts possible; thus, a full course of antenatal betamethasone was given for impending delivery. The next day, at GA 215/7 weeks, vaginal delivery was spontaneously induced with the attendance of the neonatal resuscitation team.
After birth, the baby was intubated immediately and received prophylactic surfactant. Her heart rate recovered to over 100 beats per minute after applying positive pressure ventilation for 5 minutes, showing 4/6/7 of 1/5/10 minute Apgar scores. Her body measurements were birth weight 490 g (< 10 percentile), height 30 cm (< 10 percentile), and head circumference 19 cm (< 10 percentile). Her modified Ballard score was −6, which was compatible with 20–22 weeks' GA.
After admission, she was on a ventilator and given minimal enteral feeding, starting total parenteral nutrition on hospital day (HD) #1. According to our institutional policy, her patent ductus arteriosus was managed conservatively, including judicious fluid restriction and proper ventilation strategy, and it closed spontaneously on HD #46. Postnatal dexamethasone was used during the 3rd week of life, and she was extubated on HD #60. She had full enteral feeding (> 120 mL/kg/day) achieved on HD #64 without experiencing necrotizing enterocolitis. She had one episode of blood culture proven sepsis for Enterobacter aerogenes at the 6th week of life. At corrected age (CA) 36 weeks, she was on a high flow nasal cannula that was removed at CA 39 weeks without supplemental oxygen thereafter.
Brain ultrasonography and brain magnetic resonance imaging obtained at CA 40 weeks showed intraventricular hemorrhage grade 1 with neither ventriculomegaly nor white matter injury. Retinopathy of prematurity was managed with laser treatment due to bilateral stage 3 plus at CA 36 weeks with proper regression thereafter. Both brainstem auditory and visual evoked potential examination revealed normal findings.
On HD #169, CA 55/7 weeks, she was discharged without supplemental oxygen but with a gavage tube that was removed 2 weeks later. Her body measurements at discharge were weight 3,310 g (25–50 percentile), height 45 cm (< 10 percentile), and head circumference 34 cm (25–50 percentile).
On follow-up at CA 3 months, eye contact, social smile, head control, and sitting with trunk support was possible. No hypotonia and no upper motor neuron signs were observed. She had no wheezy episodes or respiratory cause related readmissions during the follow-up period. At CA 23 months, she was able to speak some words and simple sentences and climb stairs without support. At CA 26 month, Bayley Scales of Infant Development II revealed a normal mental developmental index of 90 (95% confidence interval [CI] of 84–98) and a psychomotor developmental index of 77 (95% CI of 70–90), which was compatible with 22 months of developmental age, suggesting mildly delayed performance.
Currently, she is 43 months old, has no cerebral palsy, no hearing or visual impairment (she wears glasses due to myopia), and has good language development compared to children of the same age group, but shows delayed catch-up for growth with body weight 9.5 kg (< 3 percentile), height 86.2 cm (< 3 percentile), and head circumference 45.5 cm (< 3 percentile).
DISCUSSION
According to Bell et al.,
2 an infant with GA of 21
6/
7 weeks was the youngest surviving infant published in the English medical literature. There was a report on a web-site in 1998 of the survival of an infant born at 21
5/
7 weeks gestation.
4 However, the best obstetrical estimates of GA for most pregnancies have a margin of error of at least 5 days, probably more in pregnancies resulting in extremely preterm births. In the present case, conception occurred through IVF, so GA could be confirmed precisely as 21
5/
7 weeks.
35
There may be an ethical dilemma considering whether to resuscitate a baby born at 21 weeks GA, and whether the baby will be viable after birth. The periviable gestation, though different by nations and institutes, is constantly decreasing as extremely preterm infants' care develops and has been generally defined as 22–25 weeks in the recent decade. In 2002, the American Congress of Obstetricians and Gynecologists provided the guideline that intensive care is generally considered justifiable by 25 weeks; 23–24 weeks is a gray zone, with judgement usually made on an individual basis with consideration of the parents' wishes; and the general consensus for 22 weeks being compassionate care.
6 On the other hand, recent American Academy of Pediatrics guidelines (2009) failed to give any specific recommendations for treatment stratified on GA.
7 Many studies and committees suggested the lower limit of periviable gestation as 22 weeks' GA, with GA below that not mentioned.
8910
Survival rates of extremly preterm infants born at 22 and 23 weeks' gestation reported by Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network from the data of 2006–2011 were 5.1% and 23.6% respectively in all infants and 23.1% and 33.3% respectively in infants who received active treatment.
11 They concluded that hospital variation in survival rate of these extremly premature infants was derived partly from the hospital practice variation regarding the initation of active treatment. In Korea, according to the Korean Neonatal Network data, survival rates of infants born at 22 and 23 weeks' gestation between 2013 and 2014 who received active resuscitation and were admitted to neonatal intensive care unit (NICU), were reported as 13.8% and 41.1% respectively.
12
Accordingly, GA of 22
0/
7–23
6/
7 weeks is generally considered as the lowest GA when infants can be candidates for selective resuscitation.
1 However, relying on expected GA for the decision to resuscitate or not has several limitations. Even when not considering consent for social expenses for life-long care of a survivor with neurodevelopmental impairment, survival of extremely low GA infants is affected by multiple factors other than GA, such as antenatal steroids, sex, multiple gestation, and type of delivery. Therefore, whether to resuscitate or not should be determined individually and comprehensively with careful antenatal counseling of the parents.
13 The decision largely depends on parental wishes as well as medical professional experiences, and thus, is mostly emotional in nature.
In this case, after prenatal counseling, we learned that the parents had suffered many years due to subfertility, and were very adamant in saving the infant. Even after extensively explaining to the parents the high possibility of death or severe neurodevelopmental sequelae, they were very firm with their decision, which ultimately lead to full resuscitation of the infant. Female sex and complete administration of antenatal steroids might partly affect the prognosis favorably in this case.
In conclusion, this infant born at GA of 215/7 weeks is currently surviving at 43 months of age with a fairly good neurodevelopmental outcome. This case cannot be generalized to change our practice for very early GA infants, but paradoxically shows the importance of individualized care after meticulous antenatal counseling.