INTRODUCTION
METHODS
Inclusion criteria
Baseline intraocular pressure (IOP) ≤ 21 mmHg
Best corrected visual acuity ≥ 20/30
Spherical equivalent < ± 6D
Astigmatism < ± 3D
Normal findings on anterior segment examination and gonioscopy
Fixation loss ≤ 20%, false positive error ≤ 33%, and false negative error ≤ 33%
Study groups
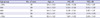
Table 1
Demographic information of normal eyes and glaucomatous eyes

Normal eye group
Glaucomatous eye group
Visual field tests
 | Fig. 2Comparison of visual field test results of LVF and HFA for a participant with normal tension glaucoma (illustrated). The diagrams on the top and the bottom show TSVs (dB) and corresponding gray scales of the left and right eyes for LVF and HFA, respectively.
LVF = LCD-based visual field testing system, HFA = Humphrey Field Analyzer II-750i, TSV = threshold sensitivity value.
|
MOBS algorithm
 | Fig. 3Example of a MOBS process for a subject with a threshold of 8 dB and making a mistake using the initial threshold range of 0 and 20 dB and the termination criteria of 3 dB as the minimum width of range and 2 as the number of reversals. After two consecutive no responses, the corresponding lower limit (10 dB) is checked and then widened to 0 dB as the mistake of the subject is confirmed. An estimate of threshold is determined as 7.8 dB as the termination criteria are satisfied (adapted from Turpin et al.23).
MOBS = Modified Binary Search.
|
LVF normative database
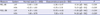
Table 2
Normative data of MD and PSD of LVF by age group
Statistical analysis
RESULTS
Comparison of MD and PSD for normal and glaucomatous eye groups
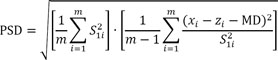
Table 3
MD and PSD values of LVF and HFA for normal eyes and glaucomatous eyes
Relationship between LVF and HFA in terms of MD and PSD
Comparison of MD and PSD AUCs of LVF and HFA
DISCUSSION
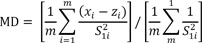
 = variance of the normal field measurement at location i, zi = reference TSV at location i, xi = measured TSV of test location i, m = number of test locations (excluding the blind spot).
= variance of the normal field measurement at location i, zi = reference TSV at location i, xi = measured TSV of test location i, m = number of test locations (excluding the blind spot). | Fig. 7Comparison of ranges of MD and PSD of normal and glaucomatous eyes for LVF and HFA.
MD = mean deviation, PSD = pattern standard deviation, LVF = LCD-based visual field testing system, HFA = Humphrey Field Analyzer II-750i.
|




 PDF
PDF Citation
Citation Print
Print








 XML Download
XML Download