2. Imhof AE. The Fielding H. Garrison lecture. From the old mortality pattern to the new: implications of a radical change from the sixteenth to the twentieth century. Bull Hist Med. 1985; 59(1):1–29. PMID:
3886046.
3. Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980–1997. Pediatrics. 2000; 106(1 Pt 2):205–209. PMID:
10888693.
4. Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001; 107(6):E99. PMID:
11389297.
5. American Academy of Pediatrics. Committee on Bioethics and Committee on Hospital Care. Palliative care for children. Pediatrics. 2000; 106(2):351–357. PMID:
10920167.
6. Fraser LK, Miller M, Aldridge J, Mckinney PA, Parslow RC, Hain R. Life-limiting and Life-threatening Conditions in Children and Young People in the United Kingdom; National and Regional Prevalence in Relation to Socioeconomic Status and Ethnicity. Leeds, United Kingdom: University of Leeds;2011.
7. Keim-Malpass J, Hart TG, Miller JR. Coverage of palliative and hospice care for pediatric patients with a life-limiting illness: a policy brief. J Pediatr Health Care. 2013; 27(6):511–516. PMID:
24055071.
8. ICPCN estimated levels of children's palliative care provision worldwide. Updated 2013. Accessed June 25, 2017.
http://www.icpcn.org.
9. Liben S. Pediatric palliative medicine: obstacles to overcome. J Palliat Care. 1996; 12(3):24–28. PMID:
8885567.
10. Martinson IM. Improving care of dying children. West J Med. 1995; 163(3):258–262. PMID:
7571589.
11. Martinson IM. Hospice care for children: past, present, and future. J Pediatr Oncol Nurs. 1993; 10(3):93–98. PMID:
8397974.
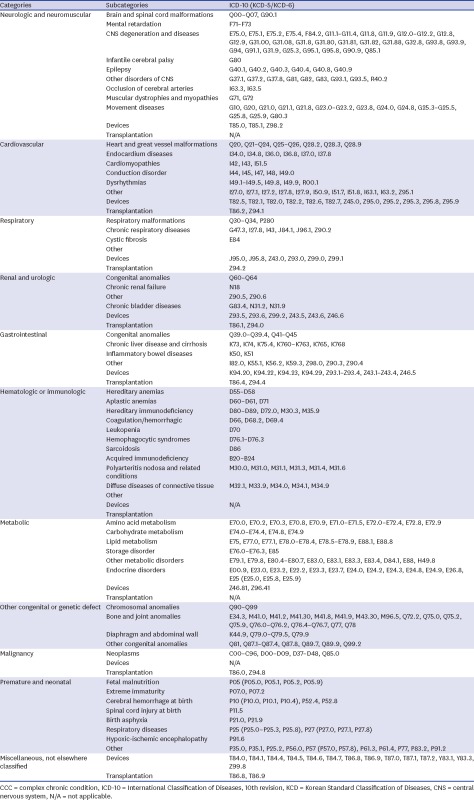
13. Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014; 14:199. PMID:
25102958.
14. Kim CG. Hospice & palliative care policy in Korea. Korean J Hosp Palliat Care. 2017; 20(1):8–17.
15. Schwantes S, O'Brien HW. Pediatric palliative care for children with complex chronic medical conditions. Pediatr Clin North Am. 2014; 61(4):797–821. PMID:
25084725.
16. Kang KA, Hwang AR. Pediatric hospice and palliative care. Korean J Hosp Palliat Care. 2012; 15(3):131–140.
17. Himelstein BP, Hilden JM, Boldt AM, Weissman D. Pediatric palliative care. N Engl J Med. 2004; 350(17):1752–1762. PMID:
15103002.
18. Liben S, Papadatou D, Wolfe J. Paediatric palliative care: challenges and emerging ideas. Lancet. 2008; 371(9615):852–864. PMID:
17707080.
19. Morrison RS, Maroney-Galin C, Kralovec PD, Meier DE. The growth of palliative care programs in United States hospitals. J Palliat Med. 2005; 8(6):1127–1134. PMID:
16351525.
20. Carter BS, Howenstein M, Gilmer MJ, Throop P, France D, Whitlock JA. Circumstances surrounding the deaths of hospitalized children: opportunities for pediatric palliative care. Pediatrics. 2004; 114(3):e361–e366. PMID:
15342898.
21. Michelson KN, Steinhorn DM. Pediatric end-of-life issues and palliative care. Clin Pediatr Emerg Med. 2007; 8(3):212–219. PMID:
18438449.
22. Wiener L, McConnell DG, Latella L, Ludi E. Cultural and religious considerations in pediatric palliative care. Palliat Support Care. 2013; 11(1):47–67. PMID:
22617619.
23. Ministry of Health and Welfare. Korea Central Cancer Registry; National Cancer Center. Annual Report of Cancer Statistics in Korea in 2014. Goyang, Korea: National Cancer Center;2016.
24. Feudtner C, Kang TI, Hexem KR, Friedrichsdorf SJ, Osenga K, Siden H, et al. Pediatric palliative care patients: a prospective multicenter cohort study. Pediatrics. 2011; 127(6):1094–1101. PMID:
21555495.
25. Bergstraesser E. Pediatric palliative care-when quality of life becomes the main focus of treatment. Eur J Pediatr. 2013; 172(2):139–150. PMID:
22476440.
26. Kreicbergs U, Valdimarsdóttir U, Onelöv E, Björk O, Steineck G, Henter JI. Care-related distress: a nationwide study of parents who lost their child to cancer. J Clin Oncol. 2005; 23(36):9162–9171. PMID:
16172455.
27. Feudtner C, Feinstein JA, Satchell M, Zhao H, Kang TI. Shifting place of death among children with complex chronic conditions in the United States, 1989–2003. JAMA. 2007; 297(24):2725–2732. PMID:
17595273.
28. Wolfe J, Hammel JF, Edwards KE, Duncan J, Comeau M, Breyer J, et al. Easing of suffering in children with cancer at the end of life: is care changing? J Clin Oncol. 2008; 26(10):1717–1723. PMID:
18375901.
29. van der Geest IM, Darlington AS, Streng IC, Michiels EM, Pieters R, van den Heuvel-Eibrink MM. Parents' experiences of pediatric palliative care and the impact on long-term parental grief. J Pain Symptom Manage. 2014; 47(6):1043–1053. PMID:
24120185.
30. Law for hospice and palliative care, and decision of life sustaining treatment for patients in dying process. Updated Feb 3, 2016. Accessed July 30, 2017.
http://www.law.go.kr.
31. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015; 47(2):127–141. PMID:
25761484.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download