Abstract
Purpose
To investigate the factors associated with glaucoma in patients with pseudoexfoliation syndrome by comparing features of the anterior segments and ocular biometry according to the presence or absence of open-angle glaucoma in pseudoexfoliation syndrome.
Methods
We analyzed 96 patients (115 eyes) diagnosed as having pseudoexfoliation syndrome in this study. The patients were divided into two groups of simple pseudoexfoliation syndrome (64 patients, 76 eyes) and pseudoexfoliation glaucoma (32 patients, 39 eyes). We compared the age, sex, underlying disease, location of pseudoexfoliative material, iris change, degree of nuclear cataract, pupil dilatation, corneal endothelial cell counts, central corneal thickness, anterior chamber depth, axial length, corneal curvature, and intraocular pressure (IOP).
Results
There were no significant differences between the two groups in terms of age (p = 0.694), sex (p = 0.161), diabetes (p = 0.440), hypertension (p = 0.238), pseudoexfoliative material observed in anterior capsule (p = 0.700), pupillary margin (p = 0.210), iris depigmentation (p = 0.526), pupillary ruff loss (p = 0.708), degree of nuclear cataract (p = 0.617), pupil dilatation (p = 0.526), central corneal thickness (p = 0.097), anterior chamber depth (p = 0.283), axial length (p = 0.095), or horizontal and vertical corneal curvature (p = 0.066 and 0.306, respectively). In pseudoexfoliation glaucoma, significantly higher IOP (p = 0.026), a high frequency of membrane formation (p = 0.047), and decreased corneal endothelial cell counts (p = 0.048) were observed.
Conclusions
Pseudoexfoliation syndrome with open-angle glaucoma was shown to be associated with high IOP, decreased corneal endothelial cell counts, and a high frequency of membrane formation. Therefore, when such changes are observed in pseudoexfoliation syndrome patients, a higher risk of open-angle glaucoma should be recognized, and careful attentionis required accordingly.
Figures and Tables
 | Figure 1Features of pupil margin without mydriasis with pseudoexfoliation syndrome. Iris sphincter depigmentation (A), membrane formation (B), pupillary ruff loss (C) are shown (arrow). |
Table 2
Comparison of the anterior segment without mydriasis between groups with and without glaucoma in pseudoexfoliation syndrome
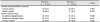
Table 3
Comparison of nuclear hardness (LOCS III) between groups with and without glaucoma in pseudoexfoliation syndrome
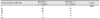
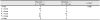
Table 4
Comparison of pupil dilatation between groups with and without glaucoma in pseudoexfoliation syndrome
Notes
References
1. Choi J, Park KH. Clinical characteristics of Korean patients with pseudoexfoliation syndrome. J Korean Ophthalmol Soc. 2006; 47:577–586.
2. Naumann GO, Schlötzer-Schrehardt U, Küchle M. Pseudoexfoliation syndrome for the comprehensive ophthalmologist. Intraocular and systemic manifestations. Ophthalmology. 1998; 105:951–968.
3. Ritch R. Exfoliation syndrome. Ritch R, Shields MB, Krupin T. The Glaucomas. 2nd ed. St. Louis: CV Mosby Co.;1996. v. 2. chap. 47.
5. Jeng SM, Karger RA, Hodge DO, et al. The risk of glaucoma in pseudoexfoliation syndrome. J Glaucoma. 2007; 16:117–121.

6. Schlötzer-Schrehardt U. Genetics and genomics of pseudoexfoliation syndrome/glaucoma. Middle East Afr J Ophthalmol. 2011; 18:30–36.

7. Grødum K, Heijl A, Bengtsson B. Risk of glaucoma in ocular hypertension with and without pseudoexfoliation. Ophthalmology. 2005; 112:386–390.

8. Koz OG, Turkcu MF, Yarangumeli A, et al. Normotensive glaucoma and risk factors in normotensive eyes with pseudoexfoliation syndrome. J Glaucoma. 2009; 18:684–688.

9. Cashwell LF Jr, Shields MB. Exfoliation syndrome. Prevalence in a southeastern United States population. Arch Ophthalmol. 1988; 106:335–336.

10. Hiller R, Sperduto RD, Krueger DE. Pseudoexfoliation, intraocular pressure, and senile lens changes in a population based survey. Arch Ophthalmol. 1982; 100:1080–1082.
13. Brooks AM, Gillies WE. The presentation and prognosis of glaucoma in pseudoexfoliation of the lens capsule. Ophthalmology. 1988; 95:271–276.

14. Gillies WE, Brooks AM. The presentation of acute glaucoma in pseudoexfoliation of the lens capsule. Aust N Z J Ophthalmol. 1988; 16:101–106.

15. Schlötzer-Schrehardt U. New pathogenetic insights into pseudoexfoliation syndrome/glaucoma. Therapeutically relevant. Ophthalmologe. 2012; 109:944–945.
16. Puska P, Vesti E, Tomita G, et al. Optic disc changes in normotensive persons with unilateral exfoliation syndrome: a 3-year follow-up study. Graefes Arch Clin Exp Ophthalmol. 1999; 237:457–462.

18. Olivius E, Thorburn W. Prognosis of glaucoma simplex and glaucoma capsulare. Acomparative study. Acta Ophthalmol (Copenh). 1978; 56:921–934.
19. Heijl A, Bengstton B, Hyman L, et al. Natural history of open-angle glaucoma. Ophthalmology. 2009; 116:2271–2276.

20. Anderson DR. Automated Static Perimetry. St. Louis: Mosby Year Book;1992. p. 123.
21. Slagsvold JE. The follow-up in patients with pseudoexfoliation of the lens capsule with and without glaucoma. 2. the development of glaucoma in persons with pseudoexfoliation. Acta Ophthalmol (Copenh). 1986; 64:241–245.
22. Chang IB, Paik DW, Kim TJ, et al. Central corneal thickness and corneal endothelial cells in pseudoexfoliation syndrome. J Korean Ophthalmol Soc. 2013; 54:1060–1065.

23. Seo JY, Park IW, Chung YS. Diverse types of glaucoma in patients with pseudoexfoliation syndrome: normal pressure glaucoma. J Korean Ophthalmol Soc. 2011; 52:1455–1460.

24. Kunishi Y. Gonioscopic features of pseudoexfoliation syndrome. Jpn J Clin Ophthalmol. 1998; 52:1683–1690.
25. Wishart PK, Spaeth GL, Poryzees Em. Anterior chamber angle in the exfoliation syndrome. Br J Ophthalmol. 1985; 69:103–107.

26. Iwanejko M, Turno-Kręcicka A, Tomczyk-Socha M, et al. Evaluation of the anterior chamber angle in pseudoexfoliation syndrome. Adv Clin Exp Med. 2017; 26:795–801.

27. Inoue K, Okugawa K, Oshika T, Amano S. Morphological study of corneal endothelium and corneal thickness in pseudoexfoliation syndrome. Jpn J Ophthalmol. 2003; 47:235–239.

28. Lindberg JG. Clinical investigations on depigmentation of the papillary border and translucency of the iris in case of senile cataract and in normal eyes in eldery persons. Acta Ophthalmol. 1989; 190:1–96.
29. Young AL, Tang WW, Lam DS. The prevalence of pseudoexfoliation syndrome in Chinese people. Br J Ophthalmol. 2004; 88:193–195.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download