The 2012 Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline for the evaluation and management of chronic kidney disease (CKD) recommends use of the 2009 CKD Epidemiology Collaboration (CKD-EPI) equation to calculate the estimated glomerular filtration rate (eGFR) for adults [
1]. The creatinine-based CKD-EPI equation is divided into four subgroup equations with regard to sex (female, male) and creatinine concentrations (62 µmol/L [0.7 mg/dL] for females; 80 µmol/L [0.9 mg/dL] for males) in “black” and “white or other” races. A single CKD-EPI equation that incorporates all of the above variables has been proposed as follows: GFR=141×Min (SCr/k,1)
α×Max (SCr/k,1)
1.209×0.993
Age [×1.018 if female] [×1.159 if black], where SCr is serum creatinine (in mg/dL), k is 0.7 for females and 0.9 for males, α is −0.329 for females and −0.411 for males, Min is the minimum of SCr/k or 1, and Max is the maximum of SCr/k or 1 [
12].
The subgroup equation employs a constant of 141 for white or other males, 144 for white or other females, 163 for black males, and 166 for black females [
12]. To express the subgroup CKD-EPI equation as a single CKD-EPI equation, previous researches multiplied the race and sex variables in the single equation by a fixed constant, 1.018 for females and 1.159 for black [
12]. In white or other females, multiplying 141 by 1.018 is 143.538 and not 144. In other words, the constant of the single equation for white or other females is 143.538, which is almost 0.5 less than the corresponding constant, 144, in the subgroup equation. Even such minor differences can affect eGFR values or GFR category. For example, for a 61-year-old Korean female with a serum creatinine concentration of 1.02 mg/dL (90.17 µmol/L), the eGFR (mL/min/1.73 m
2) value calculated by the subgroup equation would be 59.510; rounding off to the nearest integer, 60, corresponds to GFR category G2 (60–89 mL/min/1.73 m
2). By contrast, the eGFR value calculated by the single equation would be 59.31; rounding off to the nearest integer, 59, corresponds to GFR category G3a (45–59 mL/min/1.73 m
2).
There are various kinds of calculations available to clinicians in clinical laboratories via a laboratory information system (LIS), such as eGFR [
2], albumin-creatinine ratio [
3], kappa-lambda ratio [
4], risk ovarian malignancy algorithm value [
5], and some parameters from blood gas analysis [
6]. Accurate calculations are necessary for the reported numerical results, and most clinical laboratories automatically calculate and report these values using the LIS or instrument interface. Since the single creatinine-based CKD-EPI equation is easier to apply than the subgroup equation when building a query to automatically calculate eGFR on an LIS or instrument interface, the single equation is used conventionally at many institutions. Some online tools for calculating eGFR also use the single equation [
78].
We investigated how differences in eGFR values obtained using the subgroup and single creatinine-based CKD-EPI equations affect the classification of GFR category, in a large Korean cohort. We also tried to optimize the constant applied to the gender variable of the single equation so as to obtain the same GFR category from the subgroup and single creatinine-based CKD-EPI equations for the Korean population.
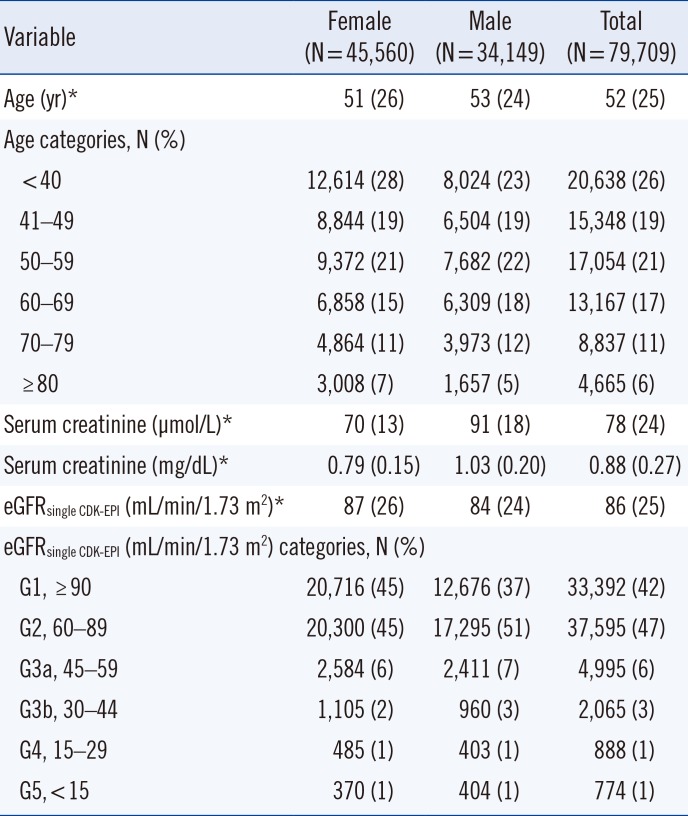
We retrospectively reviewed the electronic medical records for a total of 246,122 creatinine measurements obtained at Ewha Womans University Mokdong Hospital, Seoul, Korea, from January to December 2017. These measurements were obtained using the kinetic Jaffe method (Clinimate CRE Coloring Solution, Sekisui Medical Co. Ltd., Tokyo, Japan) with an isotope dilution mass spectrometry-traceable calibrator (Wako Multi-Chem Calibrator A, Wako Pure Chemical Industries Ltd., Osaka, Japan) on a Hitachi 7600 automatic analyzer (Hitachi, Tokyo, Japan). After excluding duplicate measurements for the same patient, patients aged 17 years and younger than 18 years, and non-Korean patients, 79,709 Koreans (45,560 females and 34,149 males) remained. A flowchart of patient selection is provided in
Supplemental Data Fig. S1. The characteristics of the study patients are summarized in
Table 1. The Institutional Review Board of Ewha Womans University Mokdong Hospital approved the study (approval number: EUMC 2018-01-048).
Table 1
Clinical characteristics of study patients
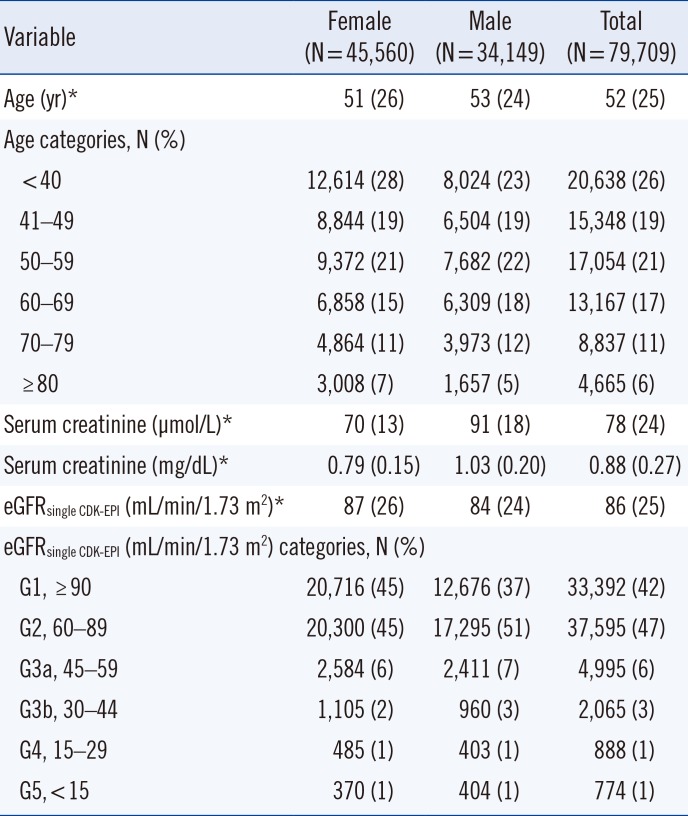
|
Variable |
Female (N = 45,560) |
Male (N = 34,149) |
Total (N = 79,709) |
|
Age (yr)*
|
51 (26) |
53 (24) |
52 (25) |
|
Age categories, N (%) |
|
|
|
|
< 40 |
12,614 (28) |
8,024 (23) |
20,638 (26) |
|
41–49 |
8,844 (19) |
6,504 (19) |
15,348 (19) |
|
50–59 |
9,372 (21) |
7,682 (22) |
17,054 (21) |
|
60–69 |
6,858 (15) |
6,309 (18) |
13,167 (17) |
|
70–79 |
4,864 (11) |
3,973 (12) |
8,837 (11) |
|
≥ 80 |
3,008 (7) |
1,657 (5) |
4,665 (6) |
|
Serum creatinine (µmol/L)*
|
70 (13) |
91 (18) |
78 (24) |
|
Serum creatinine (mg/dL)*
|
0.79 (0.15) |
1.03 (0.20) |
0.88 (0.27) |
|
eGFRsingle CDK-EPI (mL/min/1.73 m2)*
|
87 (26) |
84 (24) |
86 (25) |
|
eGFRsingle CDK-EPI (mL/min/1.73 m2) categories, N (%) |
|
G1, ≥ 90 |
20,716 (45) |
12,676 (37) |
33,392 (42) |
|
G2, 60–89 |
20,300 (45) |
17,295 (51) |
37,595 (47) |
|
G3a, 45–59 |
2,584 (6) |
2,411 (7) |
4,995 (6) |
|
G3b, 30–44 |
1,105 (2) |
960 (3) |
2,065 (3) |
|
G4, 15–29 |
485 (1) |
403 (1) |
888 (1) |
|
G5, < 15 |
370 (1) |
404 (1) |
774 (1) |

Continuous variables were expressed as mean±standard deviation if normally distributed or as median (interquartile range) if not. The eGFR of each patient was calculated by both the single and subgroup equations using Microsoft Excel 2016 (Microsoft Corporation, Santa Rosa, CA, USA). The eGFR was calculated using the creatinine value (mg/dL) to two decimal places, as recommended by the KDIGO guideline [
1], and expressed as an integer using a rounding function. Differences in the eGFR values between the two equations (single-subgroup) were analyzed using a paired t-test by using MedCalc (ver. 14.12.0; MedCalc Software, Ostend, Belgium); the subgroup equation was considered the reference method. GFR categories were determined based on eGFR (mL/min/1.73 m
2) values as follows: G1, ≥90; G2, 60–89; G3a, 45–59; G3b, 30–44; G4, 15–29; G5,<15 [
1]. The overall inter-rater agreement between the single and subgroup CKD-EPI equations was analyzed by weighted kappa.
The constant applied to gender variables in the single equation was optimized to yield the same GFR category between the single and subgroup equations. Using the same methods, we also conducted a simulation analysis for the same patients, assuming the constants used for the black race. In the single equation, the female constant was multiplied by 1.018, and the black constant was multiplied by an additional 1.159 according to the previous research [
2].
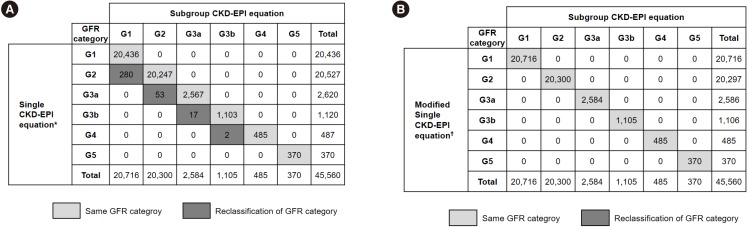
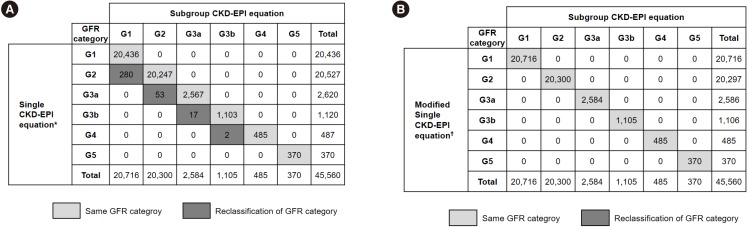
Since the single and subgroup creatinine-based CKD-EPI equations are the same for Korean males, eGFR values did not differ between equations. The eGFR value for 12,476 (27.4%) of the 45,560 female patients was lower by 1 mL/min/1.73 m
2 when calculated using the single equation (
P<0.0001). The GFR categories of 352 (0.77%) female patients were reclassified with an increase of one category level for every decrease in eGFR by 1 mL/min/1.73 m
2 (
Fig. 1A). However, applying a constant of 1.0213 (144/141=1.021276595...) rather than 1.018 eliminated the difference in eGFR between the two equations, and all female patients had the same GFR category (
Fig. 1B).
Fig. 1
Distribution of GFR category according to the creatinine-based CKD-EPI equation in females. The overall agreement between the subgroup and single equations was 99.2% (weighted kappa, 0.990; 95% confidence interval, 0.989–0.991). (A) When using the single equation with the constant 1.018, the GFR categories of 352 (0.77%, 352/45,560) patients were reclassified. (B) The use of 1.0213 rather than 1.018 eliminated the difference in eGFR. *GFR=141×min (Scr/κ, 1)α×max (Scr/κ, 1)−1.209×(0.993)Age×1.018 [if female]×1.159 [if black]; †GFR=141×min (Scr/κ, 1)α×max (Scr/κ, 1)−1.209×(0.993)Age×1.0213 [if female]×1.159 [if black].
Abbreviations: CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; eGFR, estimated glomerular filtration rate; G1, ≥90; G2, 60–89; G3a, 45–59; G3b, 30–44; G4, 15–29; G5,<15 mL/min/1.73 m2; GFR, glomerular filtration rate.

In the simulation for black patients, the eGFR from the single equation was 1 mL/min/1.73 m2 higher than that from the subgroup equation for 24,358 (53.5%) female patients (P<0.0001). Accordingly, GFR category was reclassified for 430 (0.94%) female patients. Similarly, in 8,296 (24.3%) of the 34,149 male patients, the eGFR from the single equation was 1 mL/min/1.73 m2 higher than that from the subgroup equation (P<0.0001). Accordingly, GFR category was reclassified for 167 (0.49%) male patients. Dividing the constant used in the subgroup equation for black females (166) and males (163) by 144 and 141 yielded a new constant of 1.15278 and 1.15603, respectively, which minimize the difference in eGFR values obtained with the constant of 1.159 in the single equation.
Although the Modification of Diet in Renal Disease (MDRD) equation for calculating the eGFR is multiplied by gender- and race-specific constants, there is only one MDRD equation form; therefore, the results do not change depending on the MDRD equation used for calculation [
9]. By contrast, the creatinine-based CKD-EPI equation has four subgroup equations for two race groups, although it can also be expressed as a single equation [
2]. Our results demonstrated that the different constants used for the single and subgroup creatinine-based CKD-EPI equations would result in a 1 mL/min/1.73 m
2 difference in the eGFR value depending on which equation is implemented in the LIS. Although much larger differences would likely reflect non-renal factors, biological variation in serum creatinine concentration, and ethnic coefficients of the CKD-EPI equation besides analytical performance [
10111213141516], even this minor difference can change the GFR category. For example, we found that 272 Korean females with an eGFR of 60 mL/min/1.73 m
2 (calculated by the subgroup equation) corresponded to GFR category G2, and 53 (19.5%, 53/272) of these patients were reclassified into GFR category G3a when the single equation was used.
In contrast to the “white or other” equations, the single equation for black females yielded an eGFR value 1 mL/min/1.73 m2 higher than that obtained using the corresponding subgroup equation. This is because in the “white or other” calculation, the constant 141 is multiplied by 1.018, which is slightly smaller than 144 (143.538), whereas the constant for black is 141×1.018 (if female)×1.159 (if black), which is slightly greater than 166 (166.360).
The eGFR calculated by the 2009 creatinine-based CKD-EPI equation is widely used for CKD management such as in prognosis, frequency of monitoring (number of times per year), and the need for referral in clinical practice [
117]. Therefore, it is appropriate to change the constant applied to the single equation for “white or other” females from 1.018 to 1.0213. Similarly, the constants of the single equation for black patients (female, 1.15278; male, 1.15603) need to be changed appropriately. Although changing the constants will inevitably further complicate the single equation, this should not be a problem since most clinical laboratories use an LIS for eGFR calculation.
In conclusion, clinicians should be careful when using the 2009 creatinine-based CKD-EPI equation because the eGFR values may differ by 1 mL/min/1.73 m2 depending on the manner of calculation. To minimize these differences, the constants of the single equation can be revised appropriately.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download