1. Gray ML, Killinger AH. Listeria monocytogenes and listeric infections. Bacteriol Rev. 1966; 30:309–382.
2. de Noordhout CM, Devleesschauwer B, Angulo FJ, Verbeke G, Haagsma J, Kirk M, et al. The global burden of listeriosis: a systematic review and meta-analysis. Lancet Infect Dis. 2014; 14:1073–1082.

3. Bubonja-Sonje M, Mustac E, Brunn A, Deckert M, Abram M. Listeriosis in pregnancy: case report and retrospective study. J Matern Fetal Neonatal Med. 2013; 26:321–323.

4. Lamont RF, Sobel J, Mazaki-Tovi S, Kusanovic JP, Vaisbuch E, Kim SK, et al. Listeriosis in human pregnancy: a systematic review. J Perinat Med. 2011; 39:227–236.

5. de Valk H, Jacquet C, Goulet V, Vaillant V, Perra A, Simon F, et al. Surveillance of Listeria infections in Europe. Euro Surveill. 2005; 10:251–255.
6. Elinav H, Hershko-Klement A, Valinsky L, Jaffe J, Wiseman A, Shimon H, et al. Pregnancy-associated listeriosis: clinical characteristics and geospatial analysis of a 10-year period in Israel. Clin Infect Dis. 2014; 59:953–961.

7. Committee on Obstetric Practice, American College of Obstetricians and Gynecologists. Committee opinion No. 614: management of pregnant women with presumptive exposure to Listeria monocytogenes
. Obstet Gynecol. 2014; 124:1241–1244.
8. Charlier C, Goffinet F, Azria E, Leclercq A, Lecuit M. Inadequate management of pregnancy-associated listeriosis: lessons from four case reports. Clin Microbiol Infect. 2014; 20:246–249.

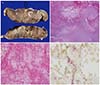
9. Barikbin P, Sallmon H, Hüseman D, Sarioglu N, Weichert A, von Weizsäcker K, et al. Clinical, laboratory, and placental findings in perinatal listeriosis. Fetal Pediatr Pathol. 2016; 35:307–314.

10. Awofisayo A, Amar C, Ruggles R, Elson R, Adak GK, Mook P, et al. Pregnancy-associated listeriosis in England and Wales. Epidemiol Infect. 2015; 143:249–256.

11. Charlier C, Perrodeau É, Leclercq A, Cazenave B, Pilmis B, Henry B, et al. Clinical features and prognostic factors of listeriosis: the MONALISA national prospective cohort study. Lancet Infect Dis. 2017; 17:510–519.
12. Mazor M, Froimovich M, Lazer S, Maymon E, Glezerman M. Listeria monocytogenes. The role of transabdominal amniocentesis in febrile patients with preterm labor. Arch Gynecol Obstet. 1992; 252:109–112.
13. Sapuan S, Kortsalioudaki C, Anthony M, Chang J, Embleton ND, Geethanath RM, et al. Neonatal listeriosis in the UK 2004–2014. J Infect. 2017; 74:236–242.

14. Thønnings S, Knudsen JD, Schønheyder HC, Søgaard M, Arpi M, Gradel KO, et al. Antibiotic treatment and mortality in patients with Listeria monocytogenes meningitis or bacteraemia. Clin Microbiol Infect. 2016; 22:725–730.
15. Committee on Obstetric Practice. Committee opinion No. 712: intrapartum management of intraamniotic infection. Obstet Gynecol. 2017; 130:e95–e101.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download