Introduction
Hysterectomy is a common gynecological procedure for treatment of benign uterine disease. However, conventional laparoscopy has limitations, including limited dexterity and range of motion, 2-dimensional vision, and a slow learning curve. These factors make complex surgical tasks difficult [
1]. To overcome these limitations, hysterectomy is frequently conducted with robotic assistance. The robotic approach is more feasible for routine clinical use than conventional laparoscopy. Its advantages include increased precision, 3-dimensional vision, and faster learning curves, and this could allow more providers to offer the robotic modality to a broader patient population with more advanced disease, particularly patients with adhesions from prior surgery, inflammation, or endometriosis [
123]. This could ultimately lead to decreased overall numbers of abdominal hysterectomies. However, high level clinical evidence comparing robotic and traditional laparoscopic techniques in benign uterine disease is lacking [
45]. Furthermore, the costs of robot-assisted hysterectomy in patients with benign uterine disease, which are associated with acquisition, application, and maintenance, have an unfavorable impact on cost-effectiveness [
23]. For these reasons, gynecologists hesitate to recommend robot-assisted hysterectomy to suitable candidates for the procedure.
Surgical outcomes cannot be evaluated based on clinical outcomes and cost-effectiveness alone; patient satisfaction is an important factor and should be the main objective of healthcare providers. However, patient satisfaction is a subjective, complex concept involving physical, emotional, mental, social, and cultural factors [
6]. Few existing studies examine satisfaction following robot-assisted hysterectomy. Furthermore, there is no standard for measuring patient satisfaction due to its complexity and multi-dimensionality.
The objectives of this study were to evaluate overall patient satisfaction with the results of robot-assisted hysterectomy and to analyze the specific factors associated with patient satisfaction using a questionnaire modified at our institution.
Materials and methods
1. Ethical considerations
Informed consent was obtained from all study participants and the study protocol was approved by the Institutional Review Board (IRB) at Hallym University Kangnam Sacred Heart Hospital (IRB file No. 2016-11-143).
2. Patients and procedures
This was a prospective study of 100 patients who underwent robot-assisted hysterectomy using the da Vinci Xi® system (Intuitive Surgical Inc., Sunnyvale, CA, USA) between March 2016 and December 2017 in the department of obstetrics and gynecology at our institution.
Patients were included if they had benign uterine disease (e.g., myoma or adenomyosis, endometrial polyp, endometrial hyperplasia) and underwent three-port robot-assisted hysterectomy. Patients were excluded if they had malignant or ovarian disease or underwent one-port robot-assisted hysterectomy.
All operations were performed by one of two surgeons, Sung Taek Park and Sung-ho Park, both of whom had overcome the learning curves of the procedure.
We distributed the questionnaire to patients when they visited outpatient department after discharge and collected the data from returned questionnaires. We also collected data on other variables from patient records, such as uterine weight, rate of pelvic adhesion, operation time, rate of transfusion, delayed discharge, and readmission.
3. Questionnaire development
The National Health Service(NHS) maintains a User Experience Survey Question Bank comprising a set of questions validated for patient use [
7]. Questions considered relevant to our service were extracted from the bank and compiled into a questionnaire [
8]. Additional questions specific to robot-assisted hysterectomy were then created, following the style of NHS-validated questions. Our questionnaire included questions regarding overall satisfaction and specific factors potentially affecting satisfaction, including postoperative pain, return to daily life, the hospital experience, wounds, cost, the doctor-patient relationship, whether expectations were met, and whether detailed information was provided.
We asked an expert for feedback on the first version of our questionnaire. We also performed a pilot study involving 5 patients to examine face and content validities, and to test the comprehensibility and feasibility of the questionnaire. In an open-ended question at the end of the questionnaire, patients were asked to provide additional comments or mention important issues that were missed in the questionnaire.
The final questionnaire included 20 questions, including 3 on overall satisfaction, 8 on demographic characteristics, 8 on factors thought to influence patient satisfaction, and one open-ended question for additional feedback or comments. The 3 questions on overall satisfaction concerned satisfaction with the surgery, whether patients would select the surgical modality again, and whether patients would recommend the surgical modality to others (questions 19, 20, and 21) (
Supplementary data 1). Patients scored each question on a 5-point Likert-type scale. A Likert scale consists of several declarative items that express a viewpoint on a topic. Respondents indicate the degree to which they agree or disagree with the opinion expressed by the statement [
6]. The questionnaire was distributed to patients when they visited an outpatient clinic for 3 months following their surgery. A total of 73 patients returned fully completed questionnaires and were included in this study. Patients with incomplete questionnaires were excluded.
4. Statistical analysis
Data were analyzed using Stata 13.1 (Stata, College Station, TX, USA). The data were categorical; therefore, variables are presented as proportions. Satisfaction score was simplified into a binary variable indicating whether or not the patient was satisfied with the surgery. Overall satisfaction was evaluated using the sum of the scores for questions 19, 20, and 21 (
Supplementary data 1). The median score was 4. Patients with a score below 4 were categorized as “satisfied”; those with a score above 4 were categorized as “not satisfied.” A bivariate analysis was performed to determine whether differences in outcome were associated with satisfaction status. A multiple logistic analysis with the binary outcome was then performed to determine the variables associated with satisfaction. Correlation analysis was performed to identify the correlation between factors.
P<0.05 was considered to be statistically significant.
Discussion
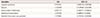
This study demonstrated that patients had high levels of overall satisfaction following robot-assisted hysterectomy. Most patients were satisfied with their operation, regardless of demographic differences. Interestingly, cost did not influence the patients' overall satisfaction. The cost of robot-assisted hysterectomy in Korea (approximately $8,000–9,000 for the surgery only, excluding inspection, hospital room, consultation, and examination fees) is 10 times greater than the cost of laparoscopic hysterectomy (approximately $800–900). Furthermore, the surgery fee for robot-assisted hysterectomy is not covered by Korea's national health insurance system, so patients must pay the entire cost out of pocket; in contrast, laparoscopic hysterectomy is covered by the national health insurance, so patients are charged only 20% of the surgery fee ($200). Notably, most patients in Korea (94.5%) have a private insurance policy to relieve financial burdens, which covers the majority of fees for robot-assisted hysterectomy (75.3%) (
Table 1). To overcome this bias, we analyzed satisfaction according to actual payment of fees. Eighteen patients paid the entire fee out of pocket, and most of them were satisfied with their operation; 11 patients were very satisfied and 7 were satisfied (question 19) (
Supplementary data 1). Therefore, we determined that cost is not an important factor in overall satisfaction.
The quality of healthcare was assessed according to three aspects: structure, process, and results [
9]. Our initial study design assigned greater value to the clinical and surgical results of care provided than to the process of providing care. However, our study shows that overall satisfaction was significantly affected by whether preoperative expectations were met, how satisfactory the hospital experience was, how satisfactory the doctor-patient relationship was, and whether sufficient detailed information was provided. The meaningful factors were associated not with clinical or surgical outcomes, as we expected, but with the process of providing services [
61011]. These findings are consistent with those of other studies evaluating patient satisfaction with surgery. Mira et al. [
12] reported a satisfaction rate of 75% in a large sample of urological, traumatological, ophthalmological, and general surgery patients discharged from multiple Spanish hospitals during a 2-month period. They found that in addition to a successful surgical procedure, other aspects of the surgical experience, such as preoperative explanation of the procedure, provision of information upon admission and discharge, and a satisfactory hospital experience, substantially influenced patients' overall satisfaction [
12]. From the patient's perspective, satisfaction with healthcare is determined not only by the outcome of treatment, but also by the extent to which the patients are supported during their hospital stay and outpatient care [
6].
In our hospital, most patients were initially provided with information about robot-assisted hysterectomy, such as its technical aspects, cost, and expected outcomes, by robot coordinators and doctors, and they selected robot-assisted hysterectomy as a surgical modality based on their doctor's recommendation. Further, our study reported that better-informed patients also evaluated their doctor-patient relationship more highly than those who were less informed. Combining these observations, we conclude that provision of information and the doctor-patient relationship are the major factors influencing patient satisfaction. Our findings concur with those of Heidegger et al. [
13], who concluded that a questionnaire to assess patient satisfaction should contain factors such as patient information, patient approach in decision-making, and contact with doctors. This indicates the importance of the healthcare delivery method in addition to the specifics of the care delivered.
Surgeons and patients choose robotic surgery for many reasons. First, robotic surgery may be easier to learn than laparoscopy because it is more analogous to traditional open surgery [
14]. Second, robotic assistance may allow for successful completion of more technically demanding cases that would otherwise have required laparotomy [
14]. Third, robotic surgery has been the subject of extensive marketing, not only to surgeons and hospitals but also to medical consumers [
14]. For these reasons, hospitals are rapidly acquiring robotic technology and using it routinely in gynecology [
1415]. However, the cost of robot-assisted hysterectomy is high, and there is little evidence to support its economic value [
15]. In this study, we confirmed the overall satisfaction of patients who underwent robot-assisted hysterectomy. Most patients were satisfied with their operation, regardless of its cost and clinical or surgical outcomes. Patients placed more value on the process of healthcare provision than on its costs or its clinical or surgical results. Furthermore, overall satisfaction was determined by the way the healthcare provider behaved toward the patient. Therefore, if gynecologists consider robot-assisted hysterectomy to be suitable for patients, they can confidently recommend it, despite its high cost.
This study has strengths in that it is the first prospective study of patient satisfaction with robot-assisted hysterectomy in a real-world setting. Additionally, data were collected prospectively, with a good follow-up rate.
However, the study also has several limitations. First, the sample size was too small. We included only 73 patients who underwent robot-assisted hysterectomy for benign uterine disease. Second, analysis was performed using data collected from a non-random sample of patients, and the results thus cannot be generalized to reflect the opinions of the overall population. Third, self-reported questionnaires are subject to participants' reporting and selection biases. Because patients voluntarily participated in this study, the results were positively biased. Forth, the questionnaire and its items were insufficient to accurately measure patient satisfaction. Additionally, only robot-assisted hysterectomy was evaluated; therefore, no direct comparison can be made to other surgical modalities within the same field of gynecology [
4].
To overcome these limitations, large, multi-center cohort studies are needed to represent the overall population in assessing the satisfaction of patients who undergo robot-assisted hysterectomy. In addition, the questionnaires used require further testing and confirmation by other investigators. More reliable and valid questionnaires are also needed to assess overall satisfaction, and further research is recommended to investigate the influence of confounding variables on patient satisfaction. Only then will the ratings of patient satisfaction become discriminatory, reproducible, and able to truly reflect overall patient satisfaction with robot-assisted hysterectomy.








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download