Abstract
Objectives
Due to the uncontrolled increase of the mobile health applications and their scarce use by elderly for reason of absence credibility of measurements by lack scientific support, the aim of this study was to evaluate the differences between the biophysical measurements based on standard instrument against a mobile application using controlled experiments with elderly to propose an effective validation model of the developed apps.
Methods
The subjects of the study (50 people) were elderly people who wanted to check their weight and cardiac status. For this purpose, two mobile applications were used to measure energy expenditure based on physical activity (Activ) and heart rate (SMCa) during controlled walking at specific speeds. Minute-by-minute measurements were recorded to evaluate the average error and the accuracy of the data acquired through confidence intervals by means of statistical analysis of the data.
Results
The experimental results obtained by the Activ/SMCa apps showed a consistent statistical similarity with those obtained by specialized equipment with confidence intervals of 95%. All the subjects were advised and trained on the use of the applications, and the initial registration of data to characterize them served to significantly affect the perceived ease of use.
Conclusions
This is the first model to validate a health-app with elderly people allowed to demonstrate the anthropometric and body movement differences of subjects with equal body mass index (BMI) but younger. Future studies should consider not only BMI data but also other variables, such as age and usability perception factors.
According to a 2016 report by Research2Guidance, there are currently about 259,000 mobile health (mHealth) apps available in megastores, such as the AppStore and Google Play Store. However, mHealth market development is dominated by Europe and the United States with higher contributions (over 70%) than those provided by South America [1]. Based on app download growth over the last four years, in 2016 there were approximately 3.2 billion downloads, which was 7% higher than the number of downloads in 2015. Consequently, statistics support the importance of research on mHealth apps and their development to underpin the health habits and practices of older adults.
mHealth apps are assessed under a benefit-risk framework [2]. The benefits of these apps can be assessed by considering their useful applications in multiple areas, such as information technologies for an approximate energy balance [3], monitoring daily activity levels (sedentary, moderate, and vigorous) of individuals [4], heart rate monitoring during physical activity [5], accessing patient data in real time [6], real-time monitoring through the use of a Bluetooth oximeter, monitoring of heart rate and oxygen saturation levels in chronic obstructive pulmonary disease (COPD) patient [7], and so forth. However, mobile apps must also be considered in terms of risks, particularly regarding the security level of user data. The main risk is the security vulnerability of user data. Another major risk of mHealth apps is the margin of error in their results approximation, thus affecting diagnoses and clinical tests, among other relevant consequences.
Analysis of the risks involved in mHealth apps has demonstrated the lack of secure protocols, such as SSL/TLS in the transmission of personal and medical data encryption. Moreover, validation and security protocols, assessment tests, and other quality requirements, are not implemented in mHealth apps for mobile platforms [8]. Among data protection regulations for mobile apps, Open Web Application Security Project (OWASP) has identified the ten most important vulnerabilities [9]; identification of these risks by the OWASP Project has reduced cyber-attacks in mHealth apps by up to 3%.
In 2015, an assessment method for mHealth apps was developed [10]. The iSYScore establishes a reliability analysis for mobile apps based on three dimensions: popularity and interest, confidence and quality, and finally, usefulness. The first dimension deals with user assessment, while the second includes professional validation or scientific organization, a crucial point focused on mHealth apps. Finally, the third dimension includes a social impact statement, confirming that research should be conducted with a sample of at least 30 users, among other key aspects. Determining the effectiveness and soundness of mHealth apps may require tools such as the iSYScore for validation [10].
In Colombia, Nunez and Caballero-Uribe [11] showed the importance of implementing telemedicine and other information technologies. Telemedicine in Colombia is a promising solution to provide access to remote places, to assist people in rural areas, and to provide early diagnoses, among other benefits. The Ministry of Information and Communication Technologies has supported initiatives in the health sector as well as in enterprises and universities by developing multiple technologies. The Universidad Militar Nueva Granada, which is implementing such an initiative, has been developing mHealth apps in recent years through the Telemedicine Research Group (TIGUM) [5]. ‘Activ’ and ‘SMCa’ are among the main apps so far developed. Although Activ and SMCa offer advantages in comparison with other apps developed, no exclusive use factor is evidenced. For users, it is essential to use mHealth apps that limit the risks previously mentioned.
Therefore, the primary aim of this study was to evaluate the differences between biophysical measurements based on standard instruments in comparison to a mobile application using controlled experiments to assess its statistical error and the limitations of its use. The second aim was to propose a model to validate the application of health with older people that allows demonstrating that the anthropometric and body movement differences are not enough to personalize mobile health applications and another variable is necessary, such as the age of the subject.
The study protocol was reviewed and approved by the Ethical Committee of the Universidad Militar Nueva Granada (UMNG), Bogota, Colombia (No. ING-2108/2365). The subjects signed an informed consent, and they were trained about their personal risk in relation to the protocol test.
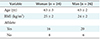
A total of 50 elderly subjects participated in this study. The tests were conducted in a sports research center with specialists in physical activity. Such tests were conducted during a 30-day period with both Activ and SMCa mobile apps (Table 1).
For analysis and validation a mixed-effects line model using the programming language R was employed. This statistical analysis allows a comparison of measured data with theoretical models (patterns).
A telehealth center was designed to centralize the information of multiple nodes: mobile applications, biomedical sensors, web applications, and so forth. Figure 1 shows the telehealth center and its key components.
Activ acquires patient data during their physical activity to calculate wear and tear (kcal). This app works through a three-axis accelerometer in the mobile device. The physical activity level is assessed by calculating the magnitude of the acceleration vector for each axis. Physical activity was recorded by a per-minute counting system using the metabolic equivalent (MET) to identify user activity intensity levels [12]. Activ calculates five physical level states: sedentary, mild, moderate, vigorous, and intense.
A Life Fitness 95Ti Treadmill (LF95 Integrity Treadmill; Life Fitness Inc., Rosemont, IL, USA) was selected for the comparison of collected signal records by Activ. The LF95 Integrity Treadmill includes Lifepulse, which is a heart rate monitoring sensor compatible with Polar telemetry. It also calculates total calories burned throughout the day or during certain time periods while engaging in physical activity using the main personal data recorded (body mass). Additionally, certain adjustments are made using a mobile device support in the center of body mass.
Activ's calibration was based on two main goals. The first was to personalize the mobile app through a user data validation process. Such a validation guarantees that personal data (age, gender, body mass, height, ethnic group, etc.) are confirmed for users' future diagnoses. The mobile app stores previously recorded physical activity data in its internal memory. To overcome this limitation, the mobile app was connected with the telehealth center at UMNG. The second goal was to create a constant record of calories burned, which would be calibrated in accordance with specialized equipment.
The user's body mass and height are essential for Activ's calibration. According to Brooks et al. [13], Activ is calibrated to determine calories burned as follows:
For the first goal, Activ adjusts the body mass and height data previously stored in the database for each user. To obtain accurate values of the app's functioning, personal data must be updated every 2 weeks. For the second goal, calorie consumption data collection was calibrated every 60 seconds. This consumption was formerly obtained by deducing the calories burned during the previous minute, thus creating some imbalance in the real value for calories burned by the user.
The SMCa mobile app was designed to record heart rate signal frequency using a heart rate telemetry strap. The app monitors strap signals via Bluetooth. Zephyr is the established communication protocol, including optimal heart rate (status) based on ranges already established during highperformance tests, daily activities (walking, baseline condition), jogging tests, and so on. Status is shown as normal, warm-up, fat burning, cardio, and intense. Zephyr HxM BT was the strap selected for the tests. This strap monitors heart rate, calories burned, steps, speed, and distance.
Finally, a mobile phone was used to conduct the tests. Calibration and programming was carried out for the Android operating system. This equipment included a Snapdragon S4 Pro dual-core processor, a 16 GB internal memory, and an accelerometer sensor using Bluetooth v4.0 LE technology.
SMCa's calibration also included the first goal of Activ's calibration. For the second goal, it was necessary to acquire signals correctly from any band over Bluetooth technology. The first SMCa version recorded data up to 127 beats per minute, but beyond that rate, the app failed and did not record any heart rate entry. This programming issue results from the protocol used to connect the cardiac strap and the mobile device. The protocol uses a frequency storage arrangement of up to 8 bits, i.e., 2N bits −1,255 arrangement settings. However, the cardiac strap records data through a converted binary system to be processed. This binary system is programmed via Java using a programming method known as two's complement (see equation below):
Two's complement calculations are carried out using logic valves to determine its decimal system equivalent. Hence, 128 positive bits result along with their complement (−127 negative bits). Storage arrangement changes were made to carry out binary-to-decimal conversion to 9 bits.
Changing the maximum heart rate formula was another adjustment made, which was suggested by specialized staff at the physical performance center:
Although it is globally used as a basic formula, it lacks precision and proper maximum heart rate measuring standards for multiple users: athletic, average physical activity, sedentary, and so forth. Also, the previous formula did not include gender distinction. This study used equation (4) for greater precision [14]:
The results were analyzed from two standpoints. First, we compared the acquired values of each record obtained by mobile apps and specialized equipment. Second, we conducted a predictive analysis of users' capabilities and limitations with respect to their records and performance.
Figure 2 shows that there was no significant shift between the mixed data of the specialized equipment and the SMCa app, so the symmetry and dispersion showed similar behavior.
The heart rate (beat per minute) was measured at various stages of physical activity. No heart beats were acquired from minutes 5 to 11 due to user's movement to hold on to the equipment. Figure 3 shows minor value deviations during the first minute while the participants were warming up. There are differences in the averages of values analyzed arising from users with huge body mass or age disparities. Thus, the correlation between the specialized equipment and SMCa app can be observed and analyzed, showing a direct relationship and a useful fit between the two measurements.
Minute 11 after physical activity top speed was considered to analyze each patient's physical conditioning level. Heart beats per minute in individuals who regularly perform physical activity constantly decrease, while those of sedentary individuals abruptly decrease. However, such in-depth analysis is beyond the scope of this study. As clearly observed, the average for minute 12 constantly decreases, thus validating the fact that the volunteers were active people. As seen in the comparison between heart rates (beats per minute) obtained by the fitness equipment and the SMCa mobile app, both showed similar values. Figure 4 shows the statistical results obtained when a linear model was applied.
These result verify that the correlation between the measurements obtained by the specialized equipment and the SMCa app was 95%.
Activ validates the theoretical and practical values obtained by the fitness equipment and those acquired by the mobile equipment. All of the tests were flawed in their value acquisition for logistics reasons during specific minutes in random mode. Consequently, values per minute were grouped into five subcategories to calculate a correlation in (5) [1516]:
Furthermore, Figure 5 shows a box plot of the Activ app. It was found that there was no significant discrepancy between the mixed data of the specialized equipment and the Activ app, so the symmetry and dispersion showed a similar behavior.
Also, as seen in Figure 6, an analysis of the correlation between the results obtained by the specialized equipment and the Activ application showed that there was a direct relationship and a useful fit between the two sets of measurements.
Figure 7 shows the statistical results obtained when the linear model was applied:
Thus, the result verified that the correlation between the measurements obtained by the specialized equipment and the Activ app was 95%.
The ActivityAware app measures the user's daily activity levels (sedentary, moderate, and vigorous), and it was previously used to implement a model to detect the level of activity of 14 subjects [4]. In this study, the sample was 50 subjects, and level of physical activity was measured in METs with 96% accuracy. The specified conditions of the model analyzed were age, body mass index, and gender.
The Exercit@rt app is used to conduct real-time monitoring of patients with COPD. Its usability has been qualitatively validated based on 6 activities with 10 patients [7] and with 94 patients to measure facility use [17]. Our study emphasized statistical validation supported by experiments approved by the ethics committee with reproducible results.
In this study, the apps were developed for implementation with Android. Likewise, a study of Gregoski et al. [18] developed an app to measure heart rate with Android; validation with 14 subjects using Bland-Altman plots for all possible pairs of devices across all conditions assessed agreement to reach 95% of the data points (differences between devices) within the limits of the agreement. In our work, we also achieved 95%, but with a sample of 50 elderly subjects.
The main contribution from the validation of Activ and SMCa mHealth apps confirms a higher precision level to calculate calories burned and heart rate. It is ideal to properly interconnect Activ and SMCa mHealth apps with a central node to capture data in real settings to analyze each patient's physical activity development. However, this analysis is nowadays conducted in a less efficient way. Results obtained by both apps can be added to electronic health records to be related to disease information and current or future prediction of diseases in elderly people.
Figures and Tables
Acknowledgments
This project has been funded by the Office of the Vice Rector for Research at Universidad Militar Nueva Granada (Project No. INV-ING-2365).
References
1. Research2Guidance. mHealth app developer economics 2016: the current status and trends of the mHealth app market [Internet]. Berlin, Germany: Research2Guidance;c2016. cited at 2018 Oct 15. Available from: http://research2guidance.com/r2g/r2g-mHealth-App-Developer-Economics-2016.pdf.
2. Santamaria-Puerto G, Hernandez-Rincon E. Mobile medical applications: definitions, benefits and risks. Salud Uninorte. 2015; 31(3):599–607.

3. Ramirez L, Rodriguez Y. mHealth mobile application for energy balance. J Ind Neotechnol. 2016; 3(2):40–47.
4. Boateng G, Batsis JA, Halter R, Kotz D. ActivityAware: an app for real-time daily activity level monitoring on the amulet wrist-worn device. In : Proceedings of 2017 IEEE International Conference on Pervasive Computing and Communications Workshops (PerCom Workshops); 2017 Mar 13–17; Kona, HI. p. 431–435.
5. Lopez LJ, Alvarez DA. SMCa: a mobile cardiac monitoring system. Ciencia Y Poder Aereo. 2013; 8(1):91–96.
6. Lysis: software for clinical laboratory with web and mobile applications [Internet]. Bogota, Colombia: Lysis;c2013. cited at 2018 Oct 15. Available from: http://lysis.co/.
7. Pereira M, Almeida AM, Caixinha H. Exercit@rt mobile: monitoring of pulmonar rehabilitation in COPD. In : Proceedings of International Conference on Technology and Innovation in Sports, Health and Wellbeing (TISHW); 2016 Dec 1–3; Vila Real, Portugal. p. 1–8.
8. Cifuentes Y, Beltran L, Ramirez L. Analysis of security vulnerabilities for mobile health applications. World Acad Sci Eng Technol Int J Health Med Eng. 2015; 9(9):1067–1072.
9. OWASP Mobile Security Project [Internet]. Wakefield (MA): OWASP;c2017. cited at 2018 Oct 15. Available from: https://www.owasp.org/index.php/OWASP_Mobile_Security_Project.
10. Grau I, Kostov B, Gallego JA, Grajales Iii F, Fernandez-Luque L, Siso-Almirall A. Assessment method for mobile health applications in Spanish: the iSYScore index. Semergen. 2016; 42(8):575–583.
11. Vloria Nunez C, Caballero-Uribe CV. Advancements and challenges for implementing telemedicine and other information technologies (TICs). Salud Uninorte. 2014; 30(2):6–8.
12. Miller NE, Strath SJ, Swartz AM, Cashin SE. Estimating absolute and relative physical activity intensity across age via accelerometry in adults. J Aging Phys Act. 2010; 18(2):158–170.

13. Brooks AG, Gunn SM, Withers RT, Gore CJ, Plummer JL. Predicting walking METs and energy expenditure from speed or accelerometry. Med Sci Sports Exerc. 2005; 37(7):1216–1223.

14. Marins JC, Fernandez MD, Peinado PJ. Accuracy of different equation to predict maximal heart rate in cycle ergometer. Arch Med Deporte. 2013; 30(1):14–20.
15. Luo X. Analyzing the correlations between the uninsured and diabetes prevalence rates in geographic regions in the United States. In : Proceedings of 2017 IEEE/ACM International Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE); 2017 Jul 17–19; Philadelphia, PA. p. 44–50.
16. Zaghbani N, Nakajima M, Nabetani H, Hafiane A. Modeling of reverse osmosis flux of aqueous solution containing glucose. Korean J Chem Eng. 2017; 34(2):407–412.





 PDF
PDF ePub
ePub Citation
Citation Print
Print











 XML Download
XML Download