1. Matthew IR, Frame JW. Policy of consultant oral and maxillofacial surgeons towards removal of miniplate components after jaw fracture fixation: pilot study. Br J Oral Maxillofac Surg. 1999; 37:110–112.

2. Falter B, Schepers S, Vrielinck L, Lambrichts I, Politis C. Plate removal following orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 112:737–743.

3. Hall JE, Uhrich TD, Barney JA, Arain SR, Ebert TJ. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg. 2000; 90:699–705.

4. Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000; 93:382–394.

5. Herr DL, Sum-Ping ST, England M. ICU sedation after coronary artery bypass graft surgery: dexmedetomidine-based versus propofol-based sedation regimens. J Cardiothorac Vasc Anesth. 2003; 17:576–584.

6. Candiotti KA, Bergese SD, Bokesch PM, Feldman MA, Wisemandle W, Bekker AY; MAC Study Group. Monitored anesthesia care with dexmedetomidine: a prospective, randomized, double-blind, multicenter trial. Anesth Analg. 2010; 110:47–56.

7. Muller S, Borowics SM, Fortis EA, Stefani LC, Soares G, Maguilnik I, et al. Clinical efficacy of dexmedetomidine alone is less than propofol for conscious sedation during ERCP. Gastrointest Endosc. 2008; 67:651–659.

8. Glass PS, Hardman D, Kamiyama Y, Quill TJ, Marton G, Donn KH, et al. Preliminary pharmacokinetics and pharmacodynamics of an ultra-short-acting opioid: remifentanil (GI87084B). Anesth Analg. 1993; 77:1031–1040.
9. Fu X, Huang F, Chen Y, Deng Y, Wang Z. Application of dexmedetomidine-remifentanil in high-intensity ultrasound ablation of uterine fibroids: a randomised study. BJOG. 2017; 124:Suppl 3. 23–29.

10. Lu Z, Li W, Chen H, Qian Y. Efficacy of a Dexmedetomidine-Remifentanil Combination Compared with a Midazolam-Remifentanil Combination for Conscious Sedation During Therapeutic Endoscopic Retrograde Cholangio-Pancreatography: A Prospective, Randomized, Single-Blinded Preliminary Trial. Dig Dis Sci. 2018; 63:1633–1640.

11. Sachar H, Pichetshote N, Nandigam K, Vaidya K, Laine L. Continued midazolam versus diphenhydramine in difficult-to-sedate patients: a randomized double-blind trial. Gastrointest Endosc. 2018; 87:1297–1303.

12. Shin S, Park CH, Kim HJ, Park SH, Lee SK, Yoo YC. Patient satisfaction after endoscopic submucosal dissection under propofol-based sedation: a small premedication makes all the difference. Surg Endosc. 2017; 31:2636–2644.

13. Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I Model development. Anesthesiology. 1997; 86:10–23.

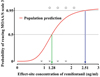
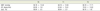
14. Heo B, Kim M, Lee H, Park S, Jeong S. Optimal effect-site concentration of remifentanil when combined with dexmedetomidine in patients undergoing cystoscopy. Korean J Anesthesiol. 2014; 66:39–43.

15. Choi BM, Lee YH, An SM, Lee SH, Lee EK, Noh GJ. Population pharmacokinetics and analgesic potency of oxycodone. Br J Clin Pharmacol. 2017; 83:314–325.

16. Lee B, Lee JR, Na S. Targeting smooth emergence: the effect site concentration of remifentanil for preventing cough during emergence during propofol-remifentanil anaesthesia for thyroid surgery. Br J Anaesth. 2009; 102:775–778.

17. Kim JS, Kim DH, Min SK, Kim KM, Kim JY. Comparison of effect-site concentration of remifentanil for tracheal intubation with the lightwand and laryngoscopy during propofol target-controlled infusion. Korean J Anesthesiol. 2011; 60:393–397.

18. Kim SH, Choi EM, Chang CH, Kim HK, Chung MH, Choi YR. Comparison of the effect-site concentrations of remifentanil for Streamlined Liner of the Pharynx Airway (SLIPA) versus laryngeal mask airway SoftSealTM insertion during target-controlled infusion of propofol. Anaesth Intensive Care. 2011; 39:611–617.

19. Lee BW, Kim SH, So KY. The effect of gender on EC(50) of remifentanil to prevent pain during injection of microemulsion propofol. Korean J Anesthesiol. 2012; 63:504–509.







 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download