Abstract
Objective
The objective of this study was to reinterpret the neurodevelopmental prognostic factors that are associated with birth head injury by performing a long-term follow-up.
Methods
Seventy-three neonates with head injuries were retrospectively analyzed after a duration of 10.0±7.3 years to determine the correlations between perinatal factors, including gender, head circumference, gestational age, body weight, and mode of delivery, and head injury factors from radiologic imaging with social, fine motor, language, and motor developmental quotients.
Results
There was a statistically significant difference between perinatal factors and head injury factors with respect to head circumference, body weight, gestational age, mode of delivery, Apgar scores at 1 min, cephalohematoma, subdural hemorrhage, subarachnoid hemorrhage, and hypoxic injury, but no direct correlation by regression analysis was observed between perinatal factors and developmental quotients. Of the head injury factors, falx hemorrhage showed a significant indirect relationship with the language and motor developmental quotients. Mode of delivery, subgaleal hematoma, cephalohematoma, greenstick skull fracture, epidural hemorrhage (EDH), tentorial hemorrhage, brain swelling, and hypoxic injury showed an indirect relationship with social development.
Conclusion
In terms of perinatal factors and head injury factors, mode of delivery, subgaleal hematoma, cephalohematoma, greenstick skull fracture, EDH, tentorial hemorrhage, falx hemorrhage, brain swelling, and hypoxic injury displayed an indirect relationship with long-term development, and therefore these factors require particular attention for perinatal care.
The incidence of perinatal traumatic head injuries ranges 2% to 7% of all pregnancies, is responsible for 2% of neonatal deaths, and is reported to be increased in dystocic presentation or instrumental delivery.12,19) In macrosomic infants birth injury increases six-fold, and it has been shown that there is a relationship between Apgar scores and neonatal or infant mortality.9,11) Furthermore, there have been studies which observed that in the long-term subgaleal hematomas leads to increased neonatal or infant mortality rates, long-term observation of birth injury showed increased rates of epilepsy and neurological disabilities.6,10) It is also suggested that there may be a relationship with adolescent attention deficit hyperactivity disorder (ADHD) and mental disease in adults.4,17) Additionally, recent advancement of ultrasound, magnetic resonance imaging (MRI) and computed tomograpy (CT) has enhanced diagnostic efficiencies.2,3,7,18) Therefore, it is deemed that there is necessity for statistical investigation into the long-term neurodevelopmental prognostic factors such as perinatal factors and birth head injury factors.
The authors of the current study ascertained the relationship between perinatal factors and birth head injury factors among birth head injury neonates, and compared the long-term follow-up outcomes of developmental quotients which may lead to a reinterpretation of neurodevelopmental prognostic factors.
We included 73 infants who were born at the Ajou University Hospital and who were diagnosed with cephalhematoma, subgaleal hematoma, large cranium, and an Apgar score of less than 6 by CT or MRI for a period of 12 months from July 1, 2006 to June 31, 2007 for this study. We excluded those birth head injuries neonates with congenital anomalies, and hemophiliac disorders from study. A retrospective study of the above neonates with regard to perinatal factors and cranial injury factors, and post-birth development assessment by the Denver test was performed.
Perinatal factors included gender, head circumference, gestational age, body weight, mode of delivery, Apgar score at 1 minute, Apgar score at 5 minutes, frontal horn ratio and frontal-parietal width ratio. Among the 73 neonates there were 41 boys and 32 girls. The mean head circumference was 58.3±37.9 percentile, mean gestational age 38.4±2.4 weeks, mode of delivery was vaginal delivery in 49, Cesarean section in 22, and vacuum delivery in 2. The mean body weight was 3034±575 g, and the Apgar score at 1 minute was 7.1±1.8, and at 5 minutes 8.1±1.7.
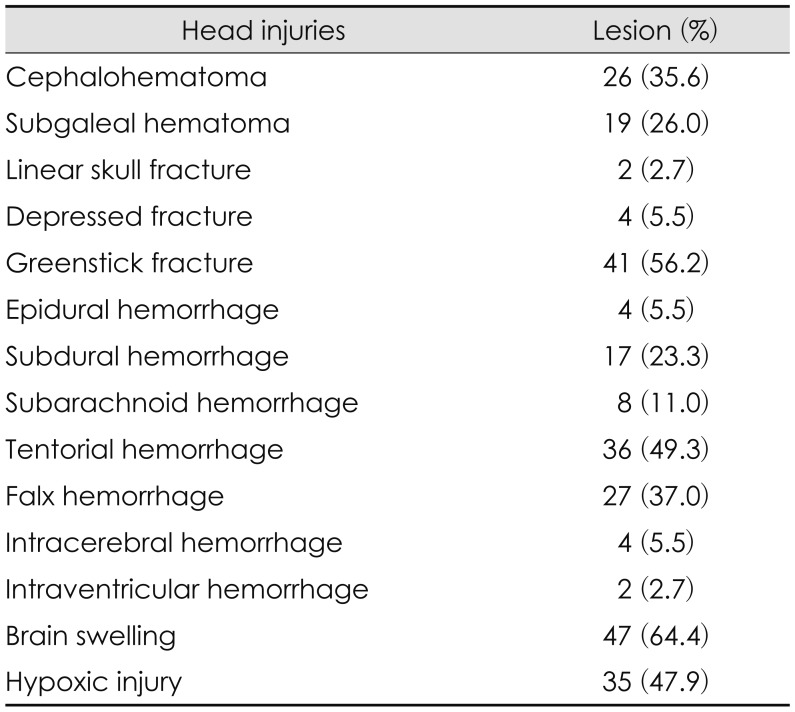
Head injury factors which included cephalohematoma, subgaleal hematoma, linear skull fracture, depressed skull fracture, greenstick skull fracture, epidural hemorrhage (EDH), subarachnoid hemorrhage, tentorial hemorrhage, falx hemorrhage, intracerebral hemorrhage, intraventricular hemorrhage, brain swelling, hypoxic injury were assessed by CT and MRI. Greenstick skull fracture analysis was according to the definitions and classification of Cho et al.7) Among the 73 neonates, the numbers of patients with linear skull fracture, depressed skull fracture, greenstick skull fracture were assessed. In those neonates with cephalohematoma, subgaleal hematoma, EDH, subarachnoid hemorrhage, tentorial hemorrhage, falx hemorrhage, hypoxic injury, lesions less than 0.5 cm were defined as Grade 0, lesions 0.5 to 1.0 cm as Grade 1, lesions 1.0 to 1.5 cm as Grade 2, and lesions greater than 1.5 cm as Grade 3. The presence of intracerebral hemorrhage or intraventricular hemorrhage that was less than 5 mL was defined as Grade 0, more than 5 mL as Grade 1, 5 to 10 mL as Grade 2, and greater than 10 mL as Grade 3. When the distance of the cranial sutural distance in brain swelling was less than 0.5 cm it was defined as Grade 0, 0.5 to 1.0 cm as Grade 1, 1.0 to 1.5 cm as Grade 2, and greater than 1.5 cm as Grade 3. The frequency of head injury factors are shown in Table 1.
Follow-up developmental examinations were performed by the Denver test at the outpatient clinic visit, and consisted of social, fine motor, language, and motor functions which were compared with the normal developmental age that were calculated for relative developmental quotients as the percentage. The mean values for social, fine motor, language, and motor relative developmental quotients were 0.685±0.273, 0.716±0.255, 0.623±0.260, 0.709±0.247, respectively, the mean follow-up period was 10.0±7.3 years, and the ratio of developmental delay that was less than 0.7 was 34.2%, 41.1%, 57.5%, and 37.5%, respectively.
Statistical analyses were performed using a Logistic regression correlation, χ2 Fisher's exact test, and p-values were calculated. Apgar scores less than 7 were considered to be abnormal. When the social, fine motor, language, and motor relative developmental quotients less than 0.6, 0.7, and 1.0 were defined as abnormal and delayed, correlation analysis showed no statistical difference between cut off values of 0.6, 0.7, and 1.0, and we only displayed the cut off value of relative developmental quotients 0.7.
Logistic regression correlation among the perinatal factors including gender, head circumference, gestational age, body weight, mode of delivery, did not show statistical significant relationship with 1 minute Apgar scores, nor with the 5 minute Apgar scores. However, the χ2 analyses of 1 minute Apgar scores demonstrated that there was statistically significant difference when perinatal and head injury factors were compared with respect to greenstick skull fracture, tentorial hemorrhage, brain swelling, and hypoxic injury. When the 5 minutes Apgar scores were analyzed by χ2/analysis of variance, the comparison of perinatal and head injury factors in terms of mode of delivery, brain swelling, and hypoxic injury showed significant difference.
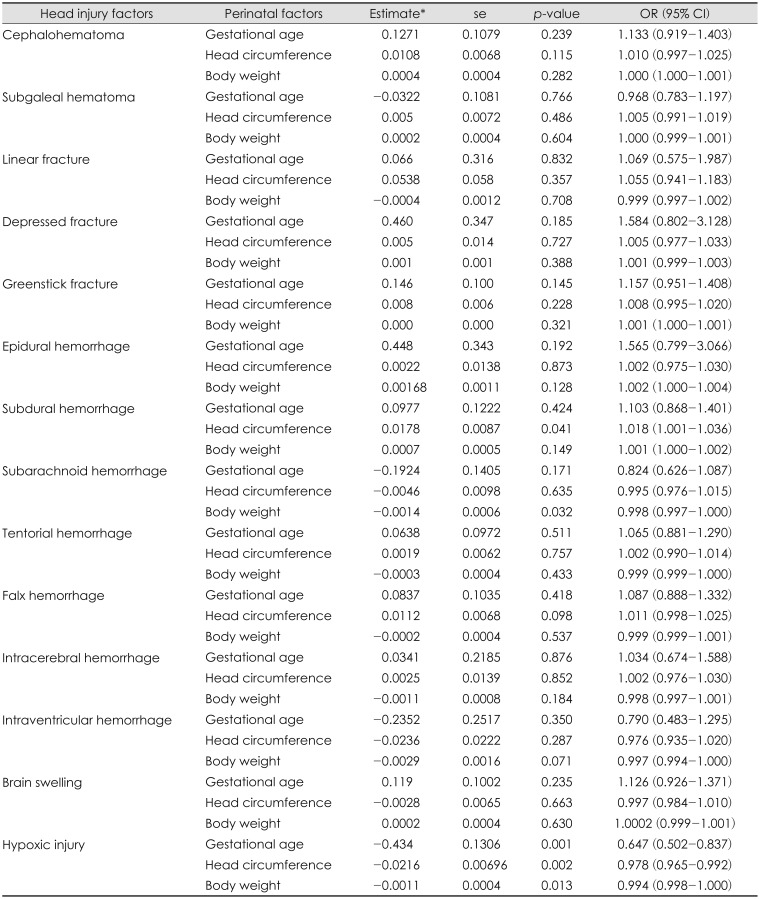
There was also significant logistic regression correlation difference between perinatal factors and head injury factors with respect to subdural hemorrhage and head circumference, subarachnoid hemorrhage and body weight, hypoxic injury and gestational age, hypoxic injury and head circumference, and hypoxic injury and body weight (Table 2).
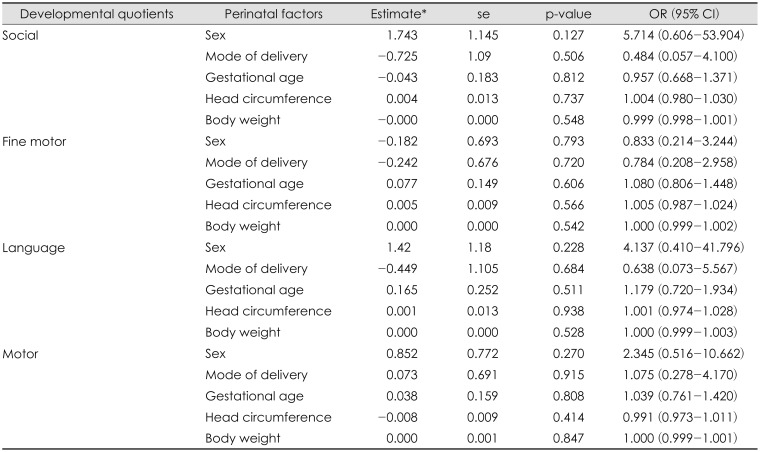
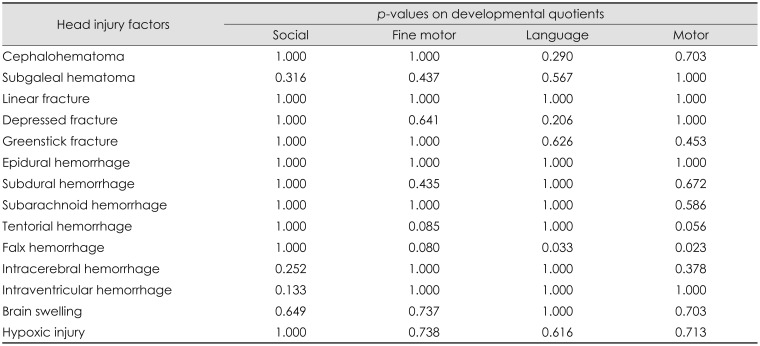
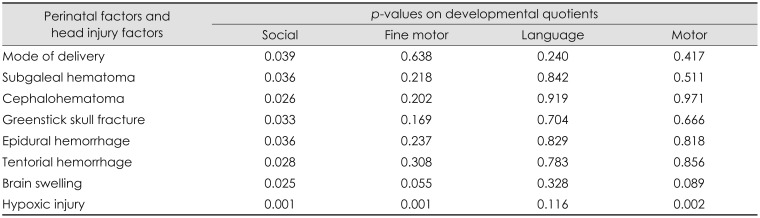
There was no significant association of perinatal factors such as gender, head circumference, gestational age, body weight, mode of delivery, with social, fine motor, language, motor developmental delay (Table 3). Fisher's exact test of head injury factors such as social, fine motor, language, and motor development demonstrated significant relationship with falx hemorrhage and language development, and falx hemorrhage and motor development (Table 4). When the 4 developmental quotients were compared by χ2 for perinatal factors and head injury factors, mode of delivery, subgaleal hematoma, cephalohematoma, greenstick skull fracture, EDH, tentorial hemorrhage, brain swelling, and hypoxic injury were significant factors for social development. Fine motor and motor development was only significant in hypoxic injury, while language development was nor significant in any fields (Table 5).
It has been shown in previous studies among the perinatal factors - mode of delivery, time of birth, low Apgar score at 5 minutes, gestational age at birth are associated with the neonatal death rate.9,15) Proposed predictors of birth trauma has been suggested to decreased fetal heart rate, shoulder dystocia, male gender, neonatal weight, neonatal head circumference, prolonged gestation, macrosomia, low Apgar scores, delivery during risk hours, instrumental delivery, fundal pressure, vaginal delivery, delivery by resident, induction of labor, second stage labor exceeding 60 minutes, epidural anesthesia, parity, and maternal age and delivery in a teaching hospital.1,13,14) In contrast, maternal age, ethnicity, diabetes, and operative vaginal delivery have not been related to birth trauma.16)
According to the results of our current research, the correlation analysis between perinatal factors and head injury factors and Apgar scores showed statistical relationships of Apgar scores with mode of delivery, greenstick skull fracture, tentorial hemorrhage, brain swelling, or hypoxic injury. In addition, the statistical analysis between perinatal factors and head injury factors revealed that head circumference, body weight, gestational age, and mode of delivery were associated with perinatal factors such as subdural hemorrhage, subarachnoid hemorrhage, hypoxic injury, and cephalohematoma. Therefore, while there is no direct relationship between most perinatal factors and Apgar scores, it is postulated that there may be an indirect association between Apgar scores and perinatal factors because relationships exist between perinatal factors and Apgar scores and between many head injury factors and Apgar scores.
It has been suggested in many previous researches that a large fetal head will result in increased compression during passage through the birth canal, subsequently leading to more frequent head injuries. Likewise, our observation in the present study shows that increase of the head circumference by 1 cm will increase subdural hemorrhage by 1.018 fold, increase of newborn body weight by 1 kg will worsen subarachnoid hemorrhage by 0.9985 fold, longer gestational age by 1 week and increase of head circumference by 1 cm and increase of newborn body weight by 1 kg resulted in increased hypoxic injury by 0.65, 0.98, and 0.99 fold, respectively. It is therefore envisaged that newborn head size governing perinatal factors such as gestational age, body weight, head circumference all contribute partially to birth head injuries of newborns.
Perinatal factors or injury such as low birth weight, reduced head circumference, incubator, hypoxic-ischemic brain injury or intraventricular hemorrhage not only increases neonatal mortality rates but also may attribute to severe neurological impairment including cerebral palsy, seizures, mental retardation, and learning disabilities, or may be related to mental diseases such as ADHD, autism, and schizophrenia in the long-term period.3,5,8,17)
Among the 4 development fields, social development showed significant differences in many perinatal factors and head injury factors and motor and language development showed difference only in the falx hemorrhage factor, while fine motor did not show such difference over any factors. Therefore, detailed caution should be given to birth injuries such as mode of delivery, subgaleal hematoma, cephalohematoma, greenstick skull fracture, EDH, tentorial hemorrhage, falx hemorrhage, brain swelling, and hypoxic injury as long-term development differences may arise. Access from other perspectives are envisaged to be necessary pertaining to social development.
The perinatal and cranial injury factors including mode of delivery, subgaleal hematoma, cephalohematoma, greenstick skull fracture, EDH, tentorial hemorrhage, falx hemorrhage, brain swelling, hydrocephalus, and hypoxic injury showed indirect relationship with long-term development in this study. Therefore, particular attention requires especially these perinatal and head injury factors in perinatal care.
References
1. Abedzadeh-Kalahroudi M, Talebian A, Jahangiri M, Mesdaghinia E, Mohammadzadeh M. Incidence of neonatal birth injuries and related factors in Kashan, Iran. Arch Trauma Res. 2015; 4:e22831. PMID: 26064868.

2. Badr LK, Bookheimer S, Purdy I, Deeb M. Predictors of neurodevelopmental outcome for preterm infants with brain injury: MRI, medical and environmental factors. Early Hum Dev. 2009; 85:279–284. PMID: 19141366.

3. Badr LK, Garg M, Kamath M. Intervention for infants with brain injury: results of a randomized controlled study. Infant Behav Dev. 2006; 29:80–90. PMID: 17138264.

4. Boksa P, El-Khodor BF. Birth insult interacts with stress at adulthood to alter dopaminergic function in animal models: possible implications for schizophrenia and other disorders. Neurosci Biobehav Rev. 2003; 27:91–101. PMID: 12732226.

5. Cannon M, Jones PB, Murray RM. Obstetric complications and schizophrenia: historical and meta-analytic review. Am J Psychiatry. 2002; 159:1080–1092. PMID: 12091183.

6. Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: associated risk factors, complications and outcome. J Paediatr Child Health. 1996; 32:228–232. PMID: 8827540.

7. Cho SM, Kim HG, Yoon SH, Chang KH, Park MS, Park YH, et al. Reappraisal of neonatal greenstick skull fractures caused by birth injuries: Comparison of 3-dimensional reconstructed computed tomography and simple skull radiographs. World Neurosurg. 2018; 109:e305–e312. PMID: 28989045.

8. Gardener H, Spiegelman D, Buka SL. Perinatal and neonatal risk factors for autism: a comprehensive meta-analysis. Pediatrics. 2011; 128:344–355. PMID: 21746727.

9. Iliodromiti S, Mackay DF, Smith GC, Pell JP, Nelson SM. Apgar score and the risk of cause-specific infant mortality: a population-based cohort study. Lancet. 2014; 384:1749–1755. PMID: 25236409.

10. Kilani RA, Wetmore J. Neonatal subgaleal hematoma: presentation and outcome--radiological findings and factors associated with mortality. Am J Perinatol. 2006; 23:41–48. PMID: 16450272.

11. Kolderup LB, Laros RK Jr, Musci TJ. Incidence of persistent birth injury in macrosomic infants: association with mode of delivery. Am J Obstet Gynecol. 1997; 177:37–41. PMID: 9240580.

12. Leestma JE. Forensic neuropathology. In : Duckett S, editor. Pediatric neuropathology. Baltimore, MD: Williams & Wilkins;1995. p. 243–283.
13. Levine MG, Holroyde J, Woods JR Jr, Siddiqi TA, Scott M, Miodovnik M. Birth trauma: incidence and predisposing factors. Obstet Gynecol. 1984; 63:792–795. PMID: 6728359.
14. Linder N, Linder I, Fridman E, Kouadio F, Lubin D, Merlob P, et al. Birth trauma-risk factors and short-term neonatal outcome. J Matern Fetal Neonatal Med. 2013; 26:1491–1495. PMID: 23560503.
15. Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012; 379:2151–2161. PMID: 22579125.

16. Mehta SH, Blackwell SC, Bujold E, Sokol RJ. What factors are associated with neonatal injury following shoulder dystocia? J Perinatol. 2006; 26:85–88. PMID: 16407959.

17. Milberger S, Biederman J, Faraone SV, Guite J, Tsuang MT. Pregnancy, delivery and infancy complications and attention deficit hyperactivity disorder: issues of gene-environment interaction. Biol Psychiatry. 1997; 41:65–75. PMID: 8988797.

18. Nongena P, Ederies A, Azzopardi DV, Edwards AD. Confidence in the prediction of neurodevelopmental outcome by cranial ultrasound and MRI in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2010; 95:F388–F390. PMID: 20870903.

19. Parker LA. Part 1: early recognition and treatment of birth trauma: injuries to the head and face. Adv Neonatal Care. 2005; 5:288–297. PMID: 16338668.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download