Abstract
Pediatric seat-belt fracture is a rare condition, and its management has not been well defined. The authors report a case of pediatric Chance fracture that was managed conservatively and that demonstrated rapid bone healing. A 7-year-old boy presented with back pain after a motor vehicle accident. Plain lumbar spine radiography, three-dimensional computed tomography (CT), and magnetic resonance imaging revealed a seat-belt fracture type C (classified by Rumball and Jarvis), and the patient's condition was managed conservatively. The patient started to ambulate with a brace 2 weeks after the injury. Spine CT performed 100 days after the injury revealed a remodeled fracture, and dynamic radiography did not show any evidence of instability or kyphotic deformity. We suggest that if there are no neurological deficits or severe deformities, then a pediatric seat-belt fracture should be managed conservatively, because the bone healing process is far more rapid in children than it is in adults and because of possible growth problems after surgery.
Flexion-distraction injury of the spine, as described by Chance, is a three-column injury. Sometimes it is treated conservatively, but usually requires surgical treatment for instability, pure ligament injury, the prevention of kyphotic deformity, and due to the possibility of additional neural injury in adults.5) In children, this injury is related to seatbelt use and treatment options are obscure because of a paucity of literature on the topic.67) Recently, we encountered a 7-year-old boy diagnosed with a seat-belt injury of the lumbar spine, who was treated conservatively. Solid bone fusion was observed at only 4 months post-injury in this case. Here, we report the case and review the possible cause of the rapid bone healing and remodeling.
A 7-year-old boy presented with back and abdominal pain after a motor vehicle accident. He was wearing seatbelt and sitting in the rear seat at the time. He complained of back pain scored at 5 on a visual analogue score (VAS) scale, and his vital signs were stable. A physical examination revealed direct tenderness on the lower back. The abdominal wall was rigid, but showed no skin lesion. He did not present any symptoms of neurological compromise.
Lumbar plain radiography showed a slight decrease in L2 body height, a widened interspinous space at the L1/2 level, and fracture lines in the middle column. Three-dimensional computed tomography (CT) showed bilateral middle and posterior column fractures involving the posterior portion of the vertebral body, pedicle, and upper lamina of L2 (Figure 1A and B). Magnetic resonance imaging (MRI) revealed additional injuries, including contusion of the L1 and L2 vertebral bodies, injury of the interspinous ligament at L1/2, and extensive contusion of back muscles (Figure 1C). An abdominal study, which included a CT scan, showed no abnormal findings.
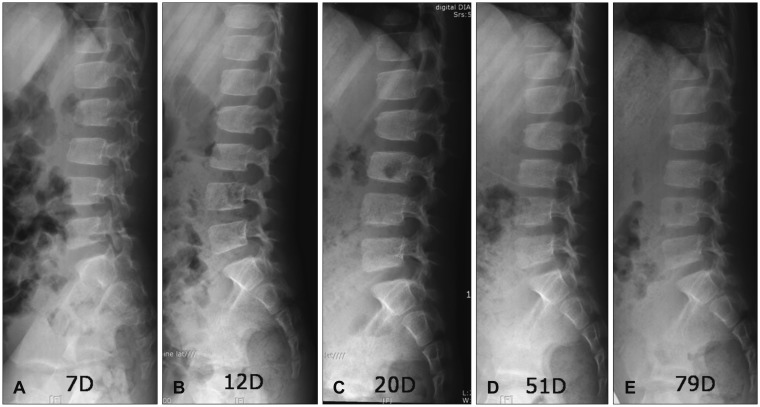
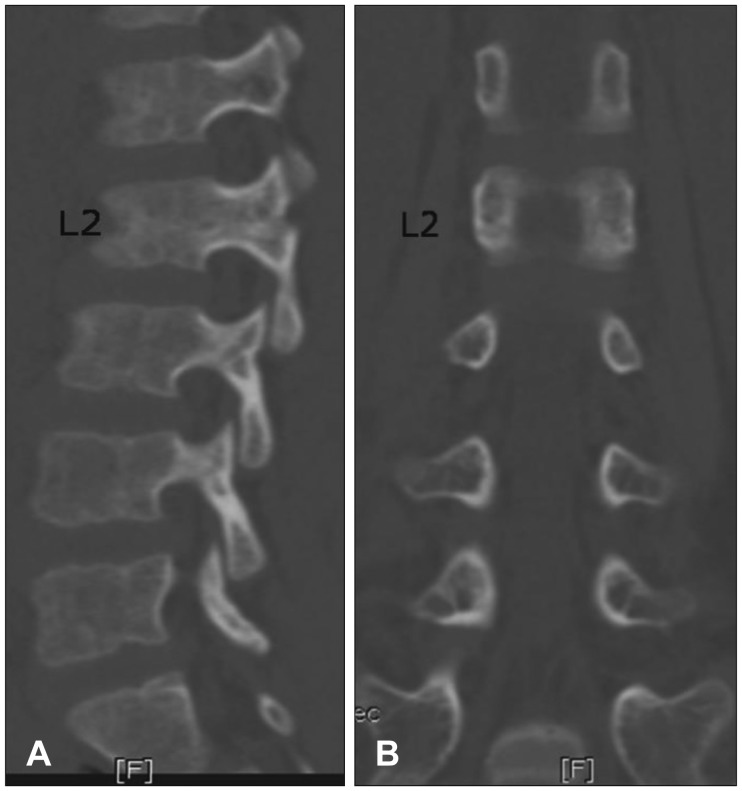
The patient was diagnosed as having a seat-belt fracture type C as classified by Rumball and Jarvis7), and we decided on delayed surgery if there were any kyphotic deformity or neurologic compromised symptoms. The back pain improved to a VAS score of 1 at 5 days post-injury. A follow-up radiographic check at 7 days showed no evidence of any change. He started to ambulate with a brace at 2 weeks postinjury, and did not complain of any pain or neurologic symptom during ambulation (Figure 2). Spinal CT at 100 days post-injury showed complete fracture healing and dynamic radiography showed stable healing (Figure 3). A bone scan performed at 8 days post-injury showed hot uptake at the L2 fracture, but growth plates of the knee and shoulder showed greater uptake (Figure 4). At 13 months post-injury, the patient had no pain and was able to lead a normal life with no evidence of kyphotic change.
This case report about the conservative management of pediatric seat-belt injury presents radiologic findings of the natural fracture healing process over 100 days and demonstrates the greater rate of bone formation in children who has intact growth plates.
Spinal injury of children are rare injury and most common courses are fall and accident.9) In the cases of thoracolumbar fractures, traffic accident is most common course.3) Seatbelt injuries of the adult spine have been well described and usually present as three-column injuries requiring surgical instrumentation. However, the incidence of seat-belt injury in children is obscure, presumably because of its rarity.4) Andras et al.2) reported delayed diagnosis of pediatric Chance fracture or thoracolumbar compression fracture were also common. Rumball and Jarvis7) reported only 10 patients managed between 1974 and 1991, and according to Santschi et al.8), 28 children aged between 2 and 16 years with seat-belt injury were reported in Canada over a two year period. However, seat-belt spinal injuries in children may be more common than previously thought.4678)
The mechanism of this spinal injury is associated with failing of the posterior element in tension and of the anterior column in compression.4) In particular, the relative large head as compared with the size of the body and the poorly developed iliac crest seem to add to the vulnerability of children to this injury. On the other hand, poorly fitting and inappropriate seat-belt adjustment are also regarded to be related to this injury in children.
Many treatment related factors ranging from conservative management to surgical instrumentation contribute to the achievement of firm fusion. However, many different opinions have been expressed about treatment. Pure osseous fractures like the “Original Chance Fracture” are treated conservatively. However, surgical treatment may be required to prevent kyphotic deformity and/or neurologic deterioration. Furthermore, if MRI findings show ligament injury, surgical treatment may also be required because of the increased possibility of instability.4)
Surgical opinions have increased in-line with surgical technique and instrumentation developments. However, concerns have been expressed about instrumentation and fusion in children. In particular, there is some evidence of adjacent segmental degeneration after instrumentation and fusion, and there is always the possibility of growth problems associated with instrumentation and surgery.10) Nevertheless, an increasing number of surgical cases are being reported. Like adult injury, for whom Thoracolumbar injury classification and severity score (TLICs) was applied for surgical decision making, TLICs for children also applied recently.3)
Rumball and Jarvis7) reported 10 cases of Chance fracture in skeletally immature patients of average age 7.5 years. One patient required instrumentation and fusion because of scoliosis and kyphosis, and the other nine patients, including two paraplegias, were treated conservatively. Mulpuri et al.6) reported 25 skeletally immature patients with a Chance fracture that were managed between 1984 and 2001. Median age at injury was 12.1 years. Seven patients presented with some extremity neurologic deficit. Sixteen patients were treated using instrumentation and fusion, and the remaining 9 patients were managed conservatively with a hyperextension cast or bracing. Furthermore, three of these 9 conservatively managed patients required operative intervention due to progressive kyphosis and instability. Radiological parameters showed better outcomes in the surgical treatment group, but pain and disability questionnaire results were poor.
In our case, the fractured spine also raised the possibility of sustained back pain because of instability and ligament injury. However, the pain subsided rapidly and bone healing as determined by CT was evident at 100 days post-injury. We believe that this rapid bone healing was due to the age of our patient. Various growth plates and thick vertebral periosteum in children would make it easier to remodel fractured bone.1) In our patient, knee growth plates exhibited stronger uptake than the fractured vertebral body in a bone scan.
However, we had no serologic evidence of an increased rate of bone healing, or increased osteoblast metabolism or osteoclast function. Nonetheless, the bone scan images obtained suggest that the bone turnover rate was higher in our patient than in adults.
Pediatric seat-belt injuries are increasing, and treatment options are controversial. We believe that pediatric seat-belt injury differs from that observed in adults, and that the rate of bone healing is considerably greater in children. Furthermore, in view of the mortality and morbidity associated with surgical intervention, we advocate that in children who are confirmed to have intact growth plates by bone scan images, pediatric seat-belt injury without neurologic impairment and instability should be initially treated conservatively.
References
1. Abdelgawad AA, Kanlic EM. Orthopedic management of children with multiple injuries. J Trauma. 2011; 70:1568–1574. PMID: 21817996.

2. Andras LM, Skaggs KF, Badkoobehi H, Choi PD, Skaggs DL. Chance fractures in the pediatric population are often misdiagnosed. J Pediatr Orthop. 2016; epub ahead of print. DOI: 10.1097/bpo.0000000000000925.

3. Dawkins RL, Miller JH, Ramadan OI, Lysek MC, Kuhn EN, Rocque BG, et al. a reliability study. J Neurosurg Pediatr. 2018; 21:284–291. PMID: 29328004.
4. Le TV, Baaj AA, Deukmedjian A, Uribe JS, Vale FL. Chance fractures in the pediatric population. J Neurosurg Pediatr. 2011; 8:189–197. PMID: 21806362.

5. Mikles MR, Stchur RP, Graziano GP. Posterior instrumentation for thoracolumbar fractures. J Am Acad Orthop Surg. 2004; 12:424–435. PMID: 15615508.

6. Mulpuri K, Jawadi A, Perdios A, Choit RL, Tredwell SJ, Reilly CW. Outcome analysis of chance fractures of the skeletally immature spine. Spine (Phila Pa 1976). 2007; 32:E702–E707. PMID: 18007230.

7. Rumball K, Jarvis J. Seat-belt injuries of the spine in young children. J Bone Joint Surg Br. 1992; 74:571–574. PMID: 1624518.

8. Santschi M, Lemoine C, Cyr C. The spectrum of seat belt syndrome among Canadian children: Results of a two-year population surveillance study. Paediatr Child Health. 2008; 13:279–283. PMID: 19337593.

9. Saul D, Dresing K. Epidemiology of vertebral fractures in pediatric and adolescent patients. Pediatr Rep. 2018; 10:7232. PMID: 29721244.

10. Smith JT. The use of growth-sparing instrumentation in pediatric spinal deformity. Orthop Clin North Am. 2007; 38:547–552. PMID: 17945134.

FIGURE 1
Three-dimensional (3D) computed tomography (CT) and magnetic resonance imaging (MRI) at presentation. (A) Sagittal 3D-CT image showing a fracture line in the L2 vertebra body. (B) Coronal 3D-CT image showing a fracture line invading bilateral pedicles. (C) T2-weighted sagittal lumbar MRI showing interspinous ligament injury and widening of the interspinous distance between L1 and 2.
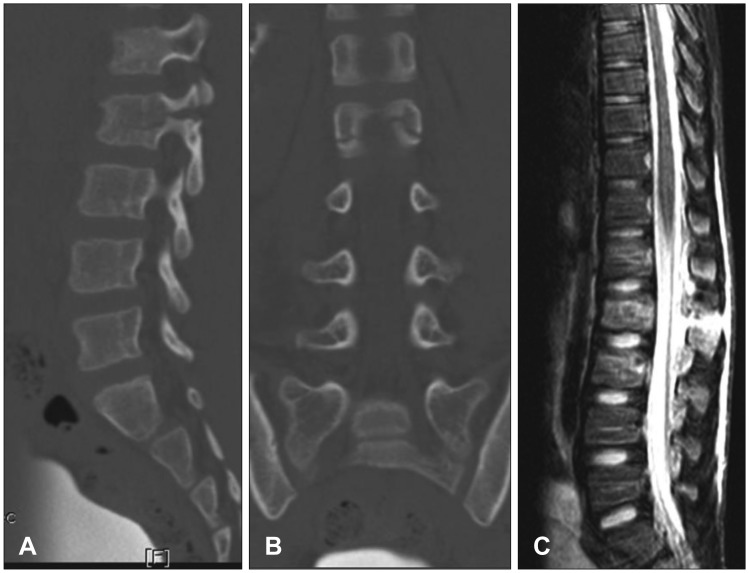
FIGURE 2
(A–D) Serial lumbar lateral radiographs were taken at 7, 12, 20, and 51 days post-injury, respectively, showing an L2 pedicle radiolucent fracture of increasing radiopacity. There was no evidence of any on-going kyphotic deformity. (E) Lumbar lateral radiograph obtained at 79 days post-injury showing similar pedicle density with other adjacent L1 and 3 pedicle.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download