This article has been
cited by other articles in ScienceCentral.
Abstract
A 43-year-old man was transferred to our hospital with recurring myelopathic symptoms after previous anterior and posterior surgical decompressions for mixed-type cervical ossification of the posterior longitudinal ligament (OPLL). Conventional magnetic resonance imaging (MRI) showed a preserved cervical curve and the achievement of successful decompression after the previous surgeries. The patient's symptoms were aggravated when he was in the extended neck posture. Dynamic MRI performed with the patient in an extended neck position revealed cord compression by OPLL from C3 to C4 with newly developed retrolisthesis of the C4–5 segment. We recommend the use of dynamic MRI to investigate motion-dependent cord compression caused by instability of the non-fused OPLL component.
Go to :

Keywords: Cervical, Dynamic, MRI, OPLL
Introduction
Ossification of the posterior longitudinal ligament (OPLL) can be treated by anterior or posterior decompression or both; the optimal surgical approach depends on the clinical characteristics, including the type of OPLL, cervical curvature, and previous cervical surgery.
18910) Even though most patients with OPLL could be treated with a single surgery, renewed or newly developed neurological deterioration often requires salvage surgery. The main reasons leading to additional surgery usually include the growing of remnant OPLL and progression of kyphosis after anterior and posterior surgery, respectively.
5)
In this study, we discussed a use of dynamic magnetic resonance imaging (MRI) for recurred cervical myelopathy by unstable changes of the non-fused OPLL component after previous surgeries.
Go to :

Case Report
A 43-year-old man was transferred from another hospital complaining of progressive weakness of the upper and lower limbs, gait disturbance and trembling in both legs after two anterior and posterior surgical decompressions.
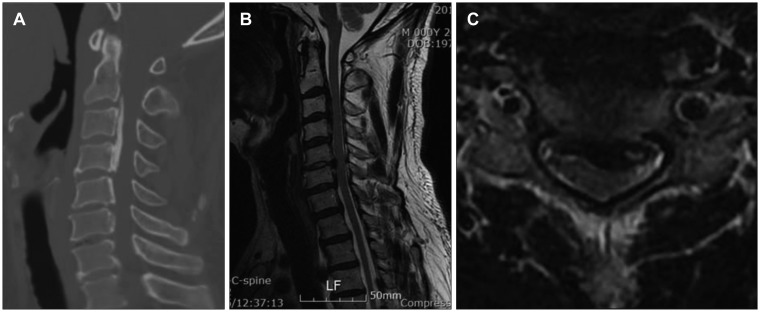
Initially, MRI revealed multi-level cord compression by OPLL from C2–6 with the mixed-type (non-fused component on C4–5); most severely, a compressed lesion with a protruded disc was identified on C5–6 segment (
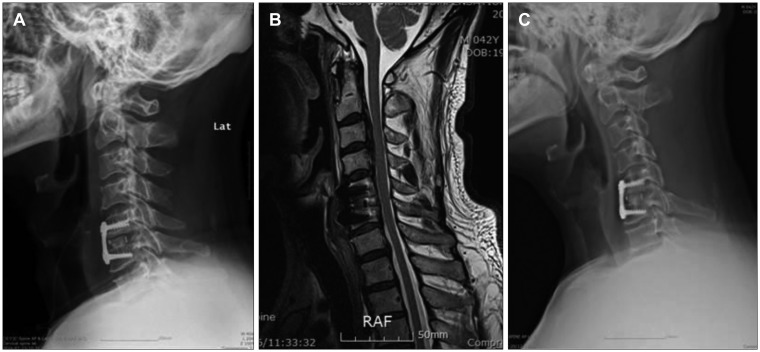
Figure 1). The patient underwent anterior cervical discectomy and fusion on C5–6 segment. There was a temporary improvement; 1 month postoperatively, the patient complained of newly developed urinary incontinence and upper motor weakness with gait disturbance. On the follow-up MRI, sustained cervical canal stenosis from C3–5 was identified. Decompressive laminectomy was performed to decompress the cervical cord from C3–5 (
Figure 2). The patient showed relieved gait disturbance and sensory changes after second surgery.
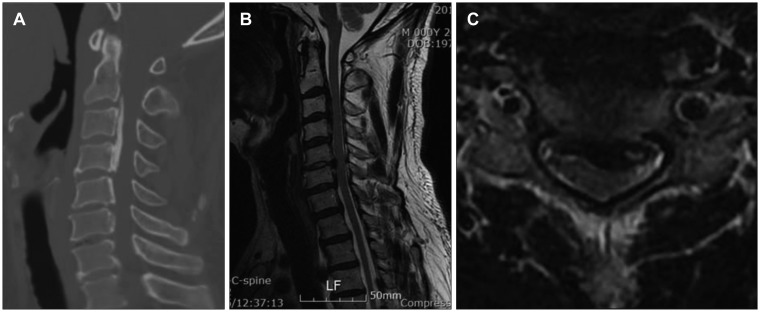 | FIGURE 1(A) Computed tomography scan and (B, C) magnetic resonance imaging reveal cord compression by ossification of the posterior longitudinal ligament (OPLL) from C2 to C6 with a mixed type (non-fused segment on C4–5). The cord is most severely compressed by OPLL and the protruded disc on C5–6 segment.
|
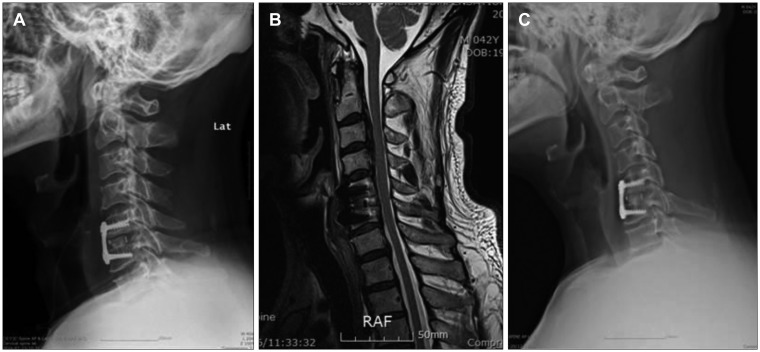 | FIGURE 2(A) There was a temporary neurological improvement following the first surgery. (B) However, the patient complained of newly developed urinary incontinence and upper motor weakness with progressing gait disturbance 1 month postoperatively. On follow-up magnetic resonance imaging, (C) there was sustained cord compression on C3 to C5. Decompressive laminectomy was performed to decompress the cervical cord on C3 to C5.
|
Unfortunately, preoperative myelopathic symptoms presented again after 3 months, it were aggravated especially in the extended neck position and lying down. On the visitation at our hospital, the patient presented grade 4 weakness of the overall limbs and only walkable with a cane. Myelopathic signs were demonstrated with a positive Hoffman sign and an increased deep tendon reflex bilaterally.
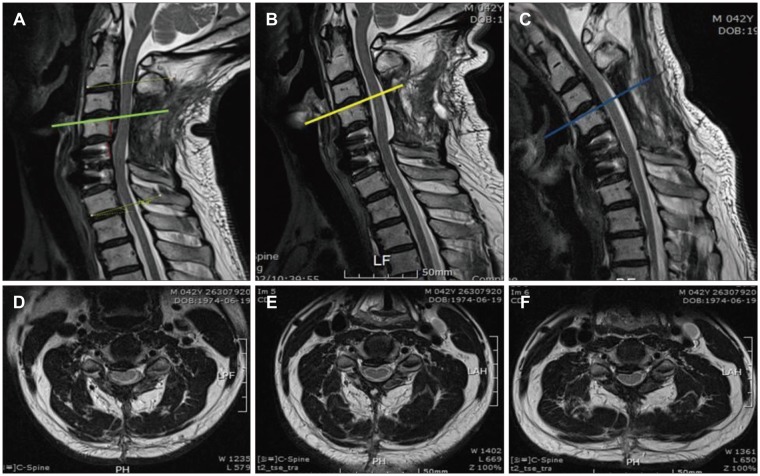
Based on the aggravation of symptoms with neck extension, dynamic MRI was applied to determine if there is cord compression depending on the cervical postures. Dynamic MRI revealed cord compression by OPLL mass from C3–4 with newly developed retrolisthesis of the C4–5 segment on the extended neck posture. However, there was no definite compressive effect of the posterior paraspinal muscles. Cord compression is partly suspected on flexed neck posture, even though there is no definite obliteration of ventral cerebrospinal fluid space. Unlike neutral neck position, cord compression was confirmed by dynamic MRI (
Figure 3).
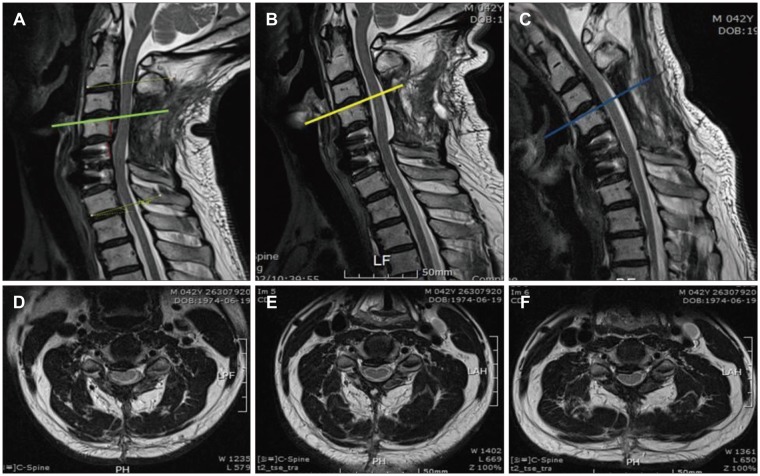 | FIGURE 3(A, D) Dynamic magnetic resonance imaging (MRI) on the extended neck posture revealed cord compression with obliteration of ventral cerebrospinal fluid (CSF) space from the C3 to C4 levels by ossification of the posterior longitudinal ligament (OPLL) with newly developed retrolisthesis of the C4–5 segment. There was no definite compressive effect of the posterior paraspinal muscles. (B, E) MRI of neutral neck posture shows no cord compression by OPLL and the posterior paraspinal muscles. (C, F) On the flexed neutral neck postures, cord compression is partially suspected on the axial view. There is slight amount of pressure on the cord without obliteration of ventral CSF space compared to extended neck posture.
|
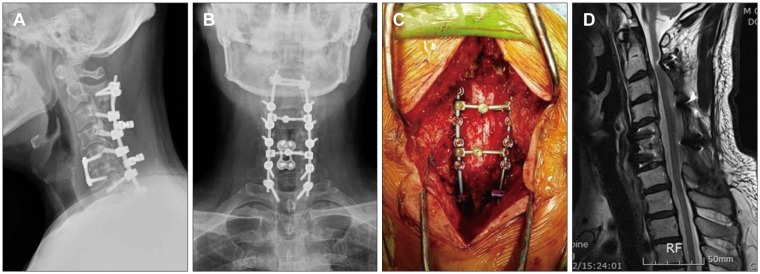
Additional decompressive laminectomy on the C6–7 levels was done, and then posterior screw fixation was conducted from C2 to T1 by placing a dome-shaped crosslink to prevent cord compression by the post-laminectomy membrane (
Figure 4). A few days after the operation, the patient showed the improvement of symptoms. After 18 months of follow-up, the patient was able to walk normally without any assistance, and there was only a slight numbness on the bilateral hands.
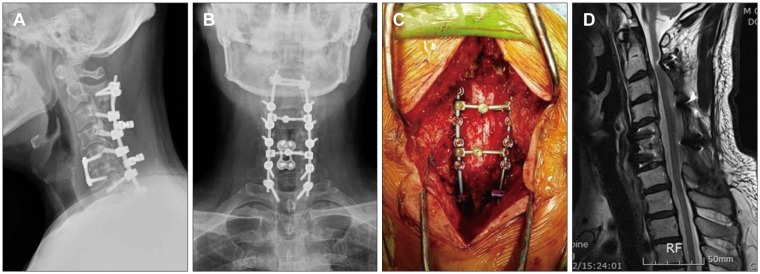 | FIGURE 4(A–C) Additional decompressive laminectomy was performed on the C6 and C7 levels with excoriation of adherent tissue around the previous laminectomy site, and then posterior screw fixation was done from C2 to T1 by placing a dome-shaped crosslink to prevent cord compression by the posterior stuructures. (D) After 18 months of follow-up, there was no cord compression either anteriorly and posteriorly on magnetic resonance imaging.
|
Go to :

Discussion
Generally, posterior surgery such as laminoplasty may be recommended in multi-segment cervical OPLL with a relatively preserved lordotic curve. One reason leading to further surgery after posterior decompression is re-pressuring at the main existing lesion by progression of cervical kyphosis. The other reason is the growing of OPLL.
5) The incidence of OPLL progression after laminoplasty has been reported in 70% to 73% of cases and is greatest in younger patients.
26) Additionally, Lee et al.
7) reported that the ossified mass at each disc level with range of motion over 5 degrees can be a risk factor for OPLL progression following laminoplasty. With the above hypotheses, we think postoperative changes in cervical alignment on the overall cervical curve and single segment might reflect dynamic instability, which can develop more frequently on the segment with an incomplete formed bone bridge of OPLL.
OPLL progression and instability are found more often in mixed-type OPLL. It can occur in the most vulnerable area, such as an incomplete bone bridge with the increased dynamic load in the environment where the movement of the upper and lower structures is lost. In this study, our patient showed increased range of motion and development of retrolisthesis on C4–5 segment with non-fused OPLL mass following posterior decompression. The upper and lower fused segments around the C4–5 lost its normal movement by fused continuous OPLL segments and anterior fusion surgery, respectively. As a result, overload occurred in C4–5 segment to compensate for the loss of movement in the other segments. On the contrary to the existing theory, progression of cervical kyphosis; unstable changes with retrolisthesis on the vulnerable segment were the main reason for cord compression.
Recently, dynamic MRI has been used to detect cervical cord compression by the paraspinal muscles after laminectomy or the change of cervical canal depend on neck position.
34) We also considered the possibility of cervical cord compression by posterior structures because of the characteristics of symptoms that aggravated with extended neck posture. However, dynamic MRI identified cervical cord compression with the anterior structure developed by instability and retrolisthesis as the cause of symptoms, with were not of posterior origin.
When considering surgical treatment in the posterior approach in multi-segment cervical OPLL, the degree of bone bridge formation at each OPLL segment should be considered with the cervical curve. Posterior fusion and screw fixation are also considered if there is a non-fused OPLL segment that tends to become unstable despite a lordotic cervical curve. Additionally, when renewed neurological deterioration has developed under a preserved cervical lordotic curve and successful decompression was shown on static MRI following laminoplasty or laminectomy, it can be helpful to investigate cord compression by instability of non-fused OPLL segment using dynamic MRI. Further studies with more patients using dynamic MRI and about the clear mechanism are required.
Go to :

Conclusion
We think the degree of bone bridge formation at each OPLL segment is also a significant factor when surgical treatment is indicated in mixed-type multi-segment cervical OPLL. We recommend the use of dynamic MRI to investigate motion-dependant cord compression by the instability of non-fused OPLL component, even if the preserved cervical curve and the achievement of successful decompression are obtained.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download