Abstract
We describe the case of a patient who had infarction of the posterior inferior cerebellar artery (PICA) after a chiropractic cervical manipulation. A 39-year-old man visited the emergency room with signs of cerebellar dysfunction, presenting with a 6-hour history of vertigo and imbalance. Two weeks ago, he was treated by a chiropractor for intermittent neck pain. At the time of admission, brain computed tomography, magnetic resonance imaging, and angiography revealed an acute infarction in the left PICA territory and occlusion of the extracranial vertebral artery (VA; V1/2 junction) as a result of the dissection of the VA. Angiography revealed complete occlusion of the left PICA and arterial dissection was shown in the extracranial portion of the VA. He was treated with antiplatelet therapy. Three weeks later, he was discharged without any sequelae. The possibility of VA dissection should be considered at least once in patients presenting with cerebellar dysfunctions with a recent history of chiropractic cervical manipulation.
Chiropractic treatment of the cervical area is a technique used often in recent years to treat musculoskeletal lesions, but it can occasionally lead to significant complications, such as dissection of the vertebral artery (VA), vertebralbasilar insufficiency, and cerebellar or brainstem infarction.127910) Complications are relatively rare, but they can be fatal and should not be neglected. We describe the case of a patient who suffered from infarction of the posterior inferior cerebellar artery (PICA) after a cervical chiropractic manipulation.
A 39-year-old man visited the emergency room with a dizziness and balance impairment that occurred 6 hours before. At the time of admission, the patient showed alert consciousness, but neurological examinations showed the signs of cerebellar dysfunction. Finger to nose, heel to shin and rapid alternating movement test showed that cerebellar function was impaired on the left side, with intact function of the right side. Blood pressure was 150/80 mmHg, and pulse rate was 88 beats/min with normal sinus rhythm of electrocardiography. He had no underlying disease and no medication use. Routine laboratory tests of blood and electrolytes, were within normal ranges. He initially denied any trauma, but remembered severe pain when he underwent a cervical chiropractic manipulation about two weeks prior. Upon imaging, skull and cervical spine radiographs were normal. Brain computed tomography (CT) showed normal cerebellar parenchyma (Figure 1A). But magnetic resonance (MR) imaging (MRI) revealed acute infarction in the left PICA territory (Figure 1B and C). Gradient echo image suggested blood clot in left PICA (Figure 1D). MR angiography revealed complete occlusion of left VA with retrograde blood flow (Figure 1E).
Transfemoral cerebral angiography revealed the occlusion of left VA at V1/2 junction. And it showed the retrograde blood flow to the left VA to the V2 segment (C1 level) and also showed the occlusion of left PICA (Figure 2A and B). After angiography, the patient was admitted to a neurological intensive care unit, and he received antiplatelet therapy with the use of Aspirin® 100 mg/day (Bayer AG, Leverkusen, Germany). There was no embolic source in the heart transthoracic echocardiogram and heart CT. And doppler ultrasonography did not reveal atherosclerosis of both internal, external carotid arteries. So it is unlikely that the infarction was caused by cardiac thrombosis or other vascular abnormalities.
At 1 month later, axial CT imaging showed the change to the chronic phase of left PICA infarction (Figure 3A). And in neck CT subtraction angiography, previously obstructed VA flow was partially improved at V1/2 level (Figure 3B). Maximum intensity projection image from enhanced CT suggested suspicious dissected wall of left VA (Figure 3C).
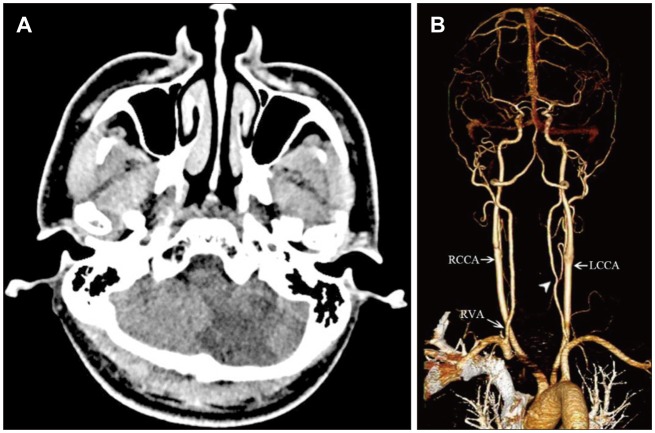
Three weeks later, he was discharged without sequelae and was regularly followed up with at an outpatient clinic using antiplatelet agents. During a follow-up at 3 months, brain and neck CT angiography showed low density in left PICA territory but showed more improved state of VA dissection at the left V1/2 junction with focal stenosis remained compared to the previous study (Figure 4A and B).
MRI vessel wall study was not performed at the first time so we did not prove the intravascular thrombosis directly. However, it could be diagnosed as a dissection because he was relatively young and healthy person and was improved so fast by only medical treatment.
To treat cervical and lumbar pain, chiropractic manipulation is considered an alternative therapy.17) This procedure can injure the neck vessels, typically representing the cervical segment of the VA, and this could produce a cerebral stroke and disability symptoms.9) Rates of VA dissection following a cervical manipulation are rarely reported, so the exact incidence is unknown.18)
VA dissection can injure the intima or media of the vessel, causing hematoma formation in the subadventitial or subintimal layer. As a result, blood flow is stopped and thrombosis or distal embolism of the dissection site appears.310) Focal ischemia occurs several hours or weeks after such a dissection, which occurs either because blood flow is reduced from the arterial blood supply or because the risk of thrombosis and embolism is increased due to the turbulence and irregularities in the vessel wall at the dissected location.24)
Any part of the carotid artery and VA can be injured, depending on the direction, degree, and force of cervical manipulation.56) But, damage to the V3 portion is the most common injury that may occur after chiropractic manipulation related to anatomical structures. The VA is located horizontally in a groove in the upper side of the atlas' posterior arch. During abruptly forced neck rotation and stretching, the gap between the atlas and the atlanto-occipital membrane, which the VA penetrates, can be stretched, resulting in dissection.1) In our case, it appeared that the V1/2 junction had been dissected due to excessive lateral bending of the neck, thought to be caused by an impact to the left transverse foramen of the sixth cervical spine, through which the left VA passes. It is presumed that there was a mechanical injury to the vessel wall at the time of the procedure, which caused dissection and then the thrombus generated, and two weeks after small emboli caused the occlusion of PICA.
Low-speed, high-amplitude manipulations that consist of a series of smooth, repetitive movements are configured in certain areas of the neck, and this does not often cause damage. However, a sudden thrust or high-speed, low-amplitude manipulation is often considered the cause of VA dissection.1) In particular, this type of manipulation can be theorized to result in a sudden, symmetrical rotation of the extended cervical vertebrae, leading to damage to the high cervical and proximal parts of the carotid artery and VA.
Rothwell et al.8) have not found an association between chiropractic treatment and stroke in elderly patients, but this may reflect a number of factors. Chiropractors assume that younger patient can actively manipulate the neck to increase the likelihood of arterial injury, and they tend to look for younger and more active chiropractic adjustments more often.
Dissection is unthinkable, and the results can be severe, so early diagnosis and treatment are essential. Patients with a recent history of seizure(s), dizziness, balance decline, and cervical chiropractic treatment should consider the possibility of VA dissection. The treatment for this is anticoagulant or antiplatelet therapy.310) Surgical intervention only applies to patients with persistent and fatal symptoms that are untreatable. Intravascular therapy, including balloon angioplasty and stenting, may be used as an initial treatment only if pharmacological treatment fails.310)
References
1. Albuquerque FC, Hu YC, Dashti SR, Abla AA, Clark JC, Alkire B, et al. Craniocervical arterial dissections as sequelae of chiropractic manipulation: patterns of injury and management. J Neurosurg. 2011; 115:1197–1205. PMID: 21923248.

2. Chen WL, Chern CH, Wu YL, Lee CH. Vertebral artery dissection and cerebellar infarction following chiropractic manipulation. Emerg Med J. 2006; 23:e1. PMID: 16373786.

3. Cho IY, Hwang SK. A case of lateral medullary infarction after endovascular trapping of the vertebral artery dissecting aneurysm. J Korean Neurosurg Soc. 2012; 51:160–163. PMID: 22639714.

4. Hutchinson PJ, Pickard JD, Higgins JN. Neurological picture. Vertebral artery dissection presenting as cerebellar infarction. J Neurol Neurosurg Psychiatry. 2000; 68:98–99. PMID: 10601413.
5. Liu D. Cervical manipulation leading to dissection was not performed by a chiropractor. Emerg Med J. 2007; 24:146.
6. Menéndez-González M, García C, Suárez E, Fernández-Díaz D, Blázquez-Menes B. Wallenberg's syndrome secondary to dissection of the vertebral artery caused by chiropractic manipulation. Rev Neurol. 2003; 37:837–839. PMID: 14606051.
7. Ramphul N, Geary U. Caveats in the management and diagnosis of cerebellar infarct and vertebral artery dissection. Emerg Med J. 2009; 26:303–304. PMID: 19307404.

8. Rothwell DM, Bondy SJ, Williams JI. Chiropractic manipulation and stroke: a population-based case-control study. Stroke. 2001; 32:1054–1060. PMID: 11340209.
9. Tarola G, Phillips RB. Chiropractic response to a spontaneous vertebral artery dissection. J Chiropr Med. 2015; 14:183–190. PMID: 26778932.

10. Yoon SY, Park SH, Hwang JH, Hwang SK. Multiple cerebral infarctions due to unilateral traumatic vertebral artery dissection after cervical fractures. Korean J Neurotrauma. 2016; 12:34–37. PMID: 27182500.

FIGURE 1
(A) Radiologic images at admission. Initial brain computed tomography does not show the abnormal density in the cerebellum. (B) Brain magnetic resonance (MR) imaging (diffusion-weighted image) and (C) brain MR imaging (apparent diffusion coefficient map) reveals an acute infarction in the left posterior inferior cerebellar artery (PICA) territory. (D) Gradient-echo image of the brain MR imaging suggests the blood clot in the PICA (black arrow). (E) MR angiography reveals the obstruction in the left proximal vertebral artery at the level of the left subclavian artery (empty arrow) with retrograde flow (arrow head). RCCA: right common carotid artery, RVA: right vertebral artery, LCCA: left common carotid artery.
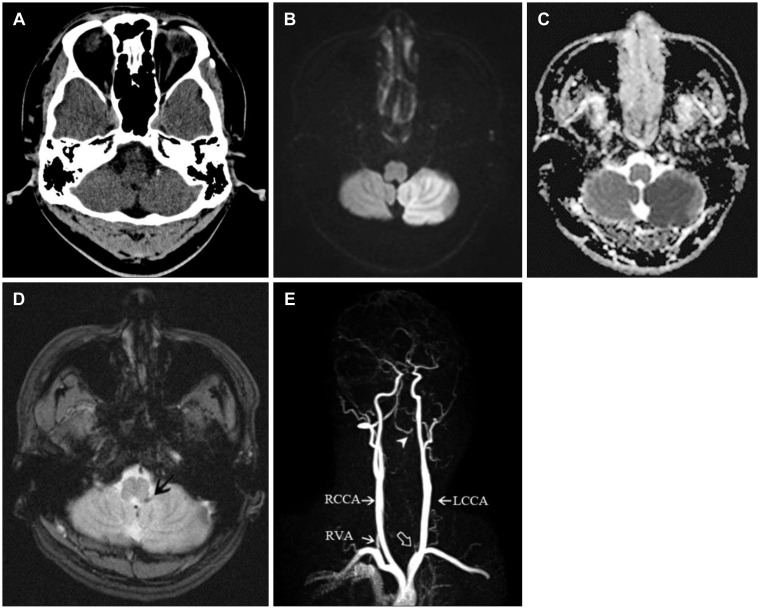
FIGURE 2
Transfemoral cerebral angiography. (A) Left vertebral artery (VA) angiography shows an occlusion of VA at extracranial portion near the transverse foramen of C6 (arrow head). (B) Right VA angiography shows a retrograde blood flow to the left VA and the occlusion of left posterior cerebellar artery (arrow head).
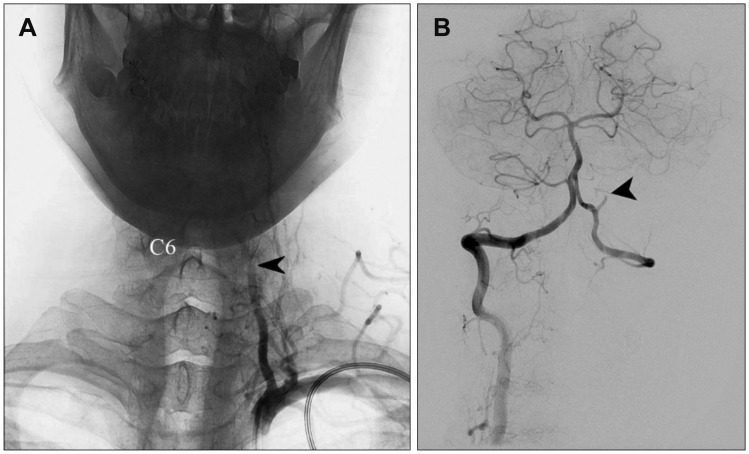
FIGURE 3
Computed tomography (CT) and CT angiography after 1 month. (A) Brain CT shows the changes for the chronic phase of the cerebellar infarction in the posterior cerebellar artery territory. (B) Three-dimensional CT angiography reveals recanalization of the dissected vertebral artery (arrow head). (C) CT angiography suggests a suspicious dissected wall of left vertebral artery (arrow head). RCCA: right common carotid artery, RVA: right vertebral artery, LCCA: left common carotid artery.
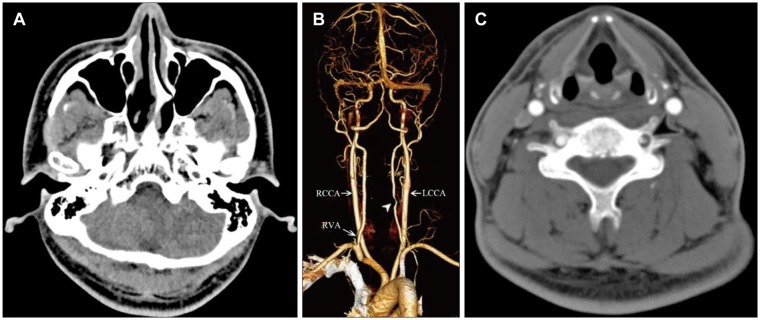
FIGURE 4
Computed tomography (CT) and CT angiography after 3 months. (A) Brain CT shows the low density in left posterior cerebellar artery territory. (B) CT angiography shows improvement of the dissection of the left vertebral artery, but still remaining of focal stenosis. RCCA: right common carotid artery, RVA: right vertebral artery, LCCA: left common carotid artery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download