Abstract
Deep neck infections (DNIs) are mainly caused by dental caries, tonsillitis, and pharyngitis; however, DNIs can also occur after head and neck trauma. A 79-year-old male patient underwent a craniectomy due to an acute subdural hematoma. The patient was unconscious and continued to have a fever, but no clear cause was found. On postoperative day 9, he suddenly showed redness and swelling on the anterior neck. Enhanced computed tomography of the pharynx revealed tracheal necrosis and an abscess in the surrounding area. An incision and drainage were performed and Enterobacter aerogenes and E. faecalis were identified. The infection was controlled after antibiotic treatment. High endotracheal tube cuff pressure was suspected as the cause of the tracheal infection. Although DNIs are difficult to predict in patients who cannot report their symptoms due to unconsciousness, prevention and rapid diagnosis are important, as DNIs have serious side effects.
Clinically, when body temperature rises above 38.3℃, this is classified as a fever.8) Fever is a common clinical symptom observed in 70% of intensive care unit (ICU) admissions. The most common causes of infection are pneumonia, surgical site infection, catheter-related urinary tract infection, clostridium difficile infection, and sinusitis.38) Deep neck infection (DNI) is uncommon, with an incidence of around 9–12/100,000 inhabitants/year.10) The use of broadspectrum antibiotics has greatly reduced the incidence and mortality of DNI, but delayed diagnosis or improper treatment can lead to serious complications.4) It is important to actively monitor and manage these infections, and if necessary, provide an appropriate antibiotic prescription and perform surgical incision and drainage. DNI cases due to high cuff pressure of endotracheal tubes (E-tubes) are rare.6) Here, we report a case of DNI due to high cuff pressure of an E-tube as a cause of fever in an unconscious patient.
A 79-year-old male patient visited our emergency department for a head injury following a fall down stairs. He underwent a brain computed tomography (CT) scan approximately 2 hours after the trauma. His initial neurologic examinations were as follows: vitals were stable, Glasgow Coma Scale (GCS) score was 14 (E4V4M6), pupils were normal bilaterally, and there was no history of loss of consciousness. Also, he had no recent history of any medical treatments or hematologic disorders, hypertension, diabetes mellitus, or alcoholism. A sudden onset of decreased consciousness (GCS E1V1M1) developed 4 hours after the trauma. Newly found increased acute subdural hematoma was detected in the left cerebral convexity on subsequent brain CT (Figure 1A). Intubation was performed preoperatively in the emergency room. Emergent surgical intervention of a craniotomy with hematoma removal was performed. After surgery, we administered ceftriaxone 2 g/qd for 4 days for operative wound care.
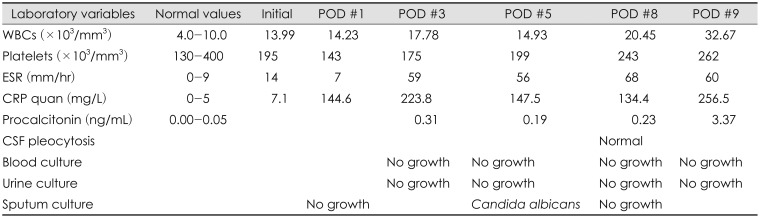
His body temperature was 39.1℃ on the first postoperative day. On laboratory evaluation, his white blood cell (WBC) count was 14,230/mm3. The erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were 7 mm/hr and 144.6 mg/dL, respectively (Table 1).
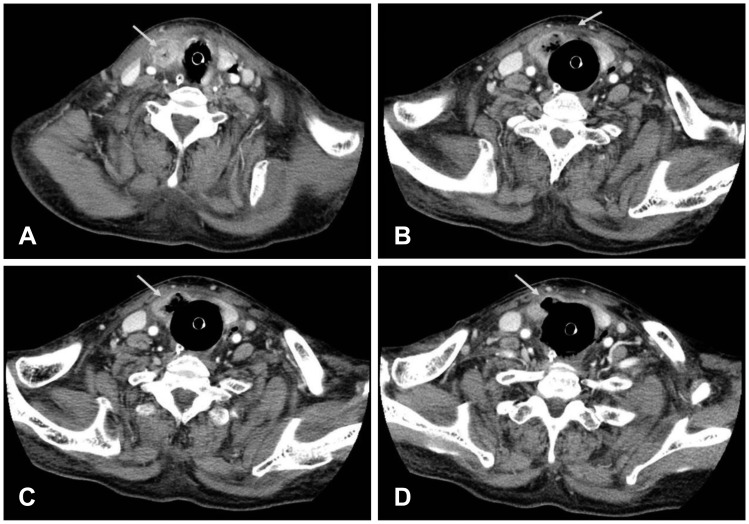
The fever focus was not found during the fever study, except lung atelectasis. We were consulted with the infectious medicine department and observed without any antibiotic prescription. However, he had a continuous fever until the eighth postoperative day, and laboratory evaluation showed no decrease in WBC, CRP, and ESR values. In a follow-up fever study, the cause remained unknown. A brain CT and cerebrospinal fluid (CSF) study were also performed to discriminate central nervous system (CNS) infection. The brain CT and CSF study did not show any specific findings (Figure 1B). On the ninth postoperative day, he suddenly showed redness and swelling on the anterior neck, and a pharynx enhanced CT (ECT) was performed. On the pharynx ECT, the E-tube cuff was found to have inflammatory findings and air bubbles in the soft tissue adjacent to the trachea were noted, extending to the right thyroid gland and both visceral spaces (Figure 2A–D). The cuff pressure of the E-tube was checked at 40 cmH2O. The cuff pressure was 25 cm-H2O when the patient was admitted to the ICU, but the tidal volume was not well-maintained and the cuff pressure increased. DNI was confirmed and an emergency operation was performed (incision and drainage with total thyroidectomy). Similar to CT findings, the inflammatory change and abscess around the E-tube cuff site were severe. Enterobacter aerogenes and E. faecalis were cultured during the operation, and sensitivity to ampicillin/sulbactam and piperacillin/tazobactam was high on antibiotic susceptibility testing. Piperacillin/tazobactam antibiotics were used to increase the antimicrobial activity against Gram negative bacteria. Following antibiotic treatment, 2 weeks of post-surgery, the injured trachea was reconstructed by covering the defect with an upper subplatysmal flap and strap muscle. After 1 week the E-tube was replaced with a tracheostomy cannula. The patient's condition improved.
A DNI occurs when inflammation spreads within the cervical facial planes and space to form an abscess.4) In the preantibiotic era, odontogenic infection was the most common cause of oral hygiene problems. Other causes include tonsillary and pharyngeal infection and trauma.210) Despite recent improvements in health status, health care, and antibiotics, DNIs have been reported in all age groups and delayed or improper treatment is associated with high mortality.24)
The incidence of DNI increases with hematologic disorders, hypertension, diabetes mellitus, and alcoholism, and there are many reports of the association between diabetes mellitus and bacterial infection.9) Elevated blood glucose increases the incidence of infection. In animal studies, short-term or long-term hyperglycemic conditions decrease immunity, including neutrophil sterilization, cell immunity, and complement activation.2) Therefore, patients with diabetes or other related systemic diseases require careful attention when treating DNIs.
Clinical signs and symptoms are important in the diagnosis of DNIs. As reported by Ballenger and Snow1) the order that DNI symptoms occur is pain, dysphagia, radiating pain, and fever. Therefore, in patients with DNI, the early symptoms reported by patients are important. However, in this case, the physical examination was limited due to the unconscious state of the patient after traumatic brain injury. Because of this, it was difficult to diagnose the skin lesions until visual appearance.
The most common bacterial strains are aerobic Streptococcus viridans, β-hemolytic streptococci, Klebsiella pneumoniae, and Staphylococcus, and anaerobic strains Bacteroides and Peptostreptococcus.19) Among these, organisms such as Staphylococcus aureus (gram-positive cocci) and gram-negative rods that produce Pseudomonas aeruginosa and extended spectrum β-lactamase-producing Enterobacteriaceae may appear, especially in at-risk patients. Therefore, in the case of an immunocompromised host (e.g., patients with chemotherapy-induced neutropenia) or patients with diabetes mellitus, postoperative infection, or trauma, the abovementioned bacteria are likely to be identified.59)
E. aerogenes and E. faecalis were also identified in this study, suggesting that trauma caused by high cuff pressure of the E-tube was the cause of the DNI. An E-tube is the best ventilation aid for airway maintenance and is not only used for airway maintenance, but is also used as a pathway for removal of organ secretions and delivery of high concentrations of oxygen. Cuff pressure is applied after E-tube insertion to reduce air leakage during tube fixation, inhalation, and mechanical ventilation. The cuff pressure to prevent airway injury and aspiration is 20 to 30 cmH2O; if a pressure of 40 cmH2O or more lasts for 15 minutes, tracheal injury may occur.10) In this case, cuff pressure on the day of DNI diagnosis was checked at 40 cmH2O, which was higher than that at the time of ICU admission. Intubation was performed preoperatively in the emergency room. The patient was not short or thick, so intubation was not difficult. In addition, intubation was carefully performed and was successful on the first attempt, with no visible damage. Similar to CT findings, the surgical site showed that the inflammatory change and abscess around E-tube cuff site were severe. Therefore, bronchial damage and increased possibility of DNI may result from high pressure. Thus, maintaining normal pressure by frequently checking the E-tube cuff pressure is important, to minimize damage due to high pressure. Early diagnosis and broad spectrum antibiotic treatment are needed for DNI, and appropriate early surgical treatment is paramount.7) In this case, early diagnosis of DNI was difficult as the patient was unconscious. However, the patient's condition improved with appropriate antibiotic and surgical treatment. Therefore, if the cause of fever is difficult to find in an unconscious patient after trauma, although the incidence of DNI is low, investigating for DNI may improve patient outcomes.
DNI can cause life-threatening complications if diagnosis is delayed or inappropriate treatment is given. The most common causes of DNI are odontogenic infections, surgical trauma, trauma, and esophageal perforation. In rare cases, DNI can be caused by high cuff pressure, as in our case. Particularly in our case, there was a limitation in the physical examination, as the patient had impaired consciousness. Therefore, it is important to note that DNI due to E-tube high cuff pressure may occur when the cause of fever is unknown in patients with reduced consciousness after trauma.
References
1. Ballenger JJ, Snow JB. Otorhinolaryngology: head and neck surgery. ed 15th. Baltimore, MD: Williams & Wilkins;1996.
2. Daramola OO, Flanagan CE, Maisel RH, Odland RM. Diagnosis and treatment of deep neck space abscesses. Otolaryngol Head Neck Surg. 2009; 141:123–130. PMID: 19559971.

4. Kinzer S, Pfeiffer J, Becker S, Ridder GJ. Severe deep neck space infections and mediastinitis of odontogenic origin: clinical relevance and implications for diagnosis and treatment. Acta Otolaryngol. 2009; 129:62–70. PMID: 18607917.

5. Levi ME, Eusterman VD. Oral infections and antibiotic therapy. Otolaryngol Clin North Am. 2011; 44:57–78. PMID: 21093623.

6. Orta DA, Cousar JE 3rd, Yergin BM, Olsen GN. Tracheal laceration with massive subcutaneous emphysema: a rare complication of endotracheal intubation. Thorax. 1979; 34:665–669. PMID: 515988.

7. Osborn TM, Assael LA, Bell RB. Deep space neck infection: principles of surgical management. Oral Maxillofac Surg Clin North Am. 2008; 20:353–365. PMID: 18603196.

8. Ryan M, Levy MM. Clinical review: fever in intensive care unit patients. Crit Care. 2003; 7:221–225. PMID: 12793871.
9. Sethi DS, Stanley RE. Deep neck abscesses-changing trends. J Laryngol Otol. 1994; 108:138–143. PMID: 8163915.
10. Vieira F, Allen SM, Stocks RM, Thompson JW. Deep neck infection. Otolaryngol Clin North Am. 2008; 41:459–483. PMID: 18435993.

FIGURE 1
Preoperative and postoperative brain CT. (A) Preoperative brain CT scan shows increased right convexity subdural hematoma with midline shift to the left. (B) The CT scan from postoperative day 8 shows resolving hematoma and improved midline shifting.
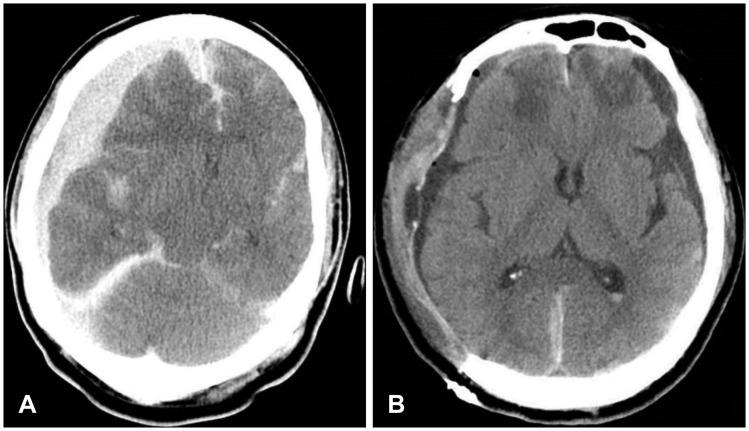
FIGURE 2
Contrast-enhanced neck CT scan. An over distension state of the upper (cervical) trachea and adjacent soft tissue with air bubbles around the trachea, the right thyroid gland, and both visceral spaces are shown (A and B). Severe infection and necrosis around the endotracheal tube cuff is revealed (C and D, white arrow).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download