Abstract
We describe the case of a patient with an acute subdural hematoma (SDH) that was removed using urokinase irrigation after burr hole trephination in a limited situation where craniotomy was not possible. A 90-year-old woman was admitted to our hospital with a stuporous mental status. Computed tomography (CT) scans revealed a chronic SDH, and a burr hole procedure was performed. The patient's postoperative progression was good until the third day after surgery when we found that the acute SDH had increased on CT scans. The patient's guardian refused further surgery, and thus we drained the blood from the hematoma by injecting urokinase through a drainage catheter. We used urokinase for two days, and removed the catheter after confirming via CT scans that the hematoma was almost alleviated. The patient recovered gradually; she was discharged with few neurological deficits.
Acute subdural hematoma (SDH) can be treated conservatively if the neurologic symptoms are mild or the size of the hematoma is small; however, immediate surgical treatment should be considered if patient shows loss of consciousness, worsening of neurological symptoms, or a large size of hematoma.715) The primary surgical treatment for acute SDH is to perform craniotomy which can remove hematoma completely, but there may be complications from general anesthesia and procedure itself. One may consider burr hole surgery for removal of hematoma, but it is difficult to secure the clear view of surgical sight, completely remove hematoma, and decrease intracranial pressure in short period of time. We report the result of burr hole drainage with additional urokinase for removal of hematoma in a limited situation where craniotomy is not possible.
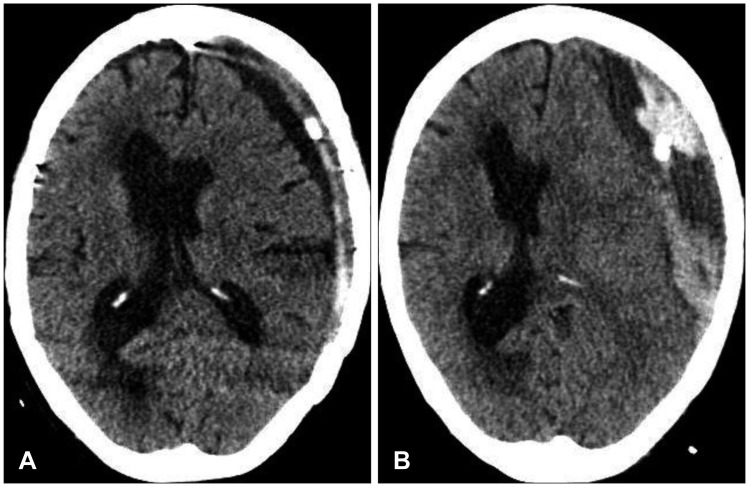
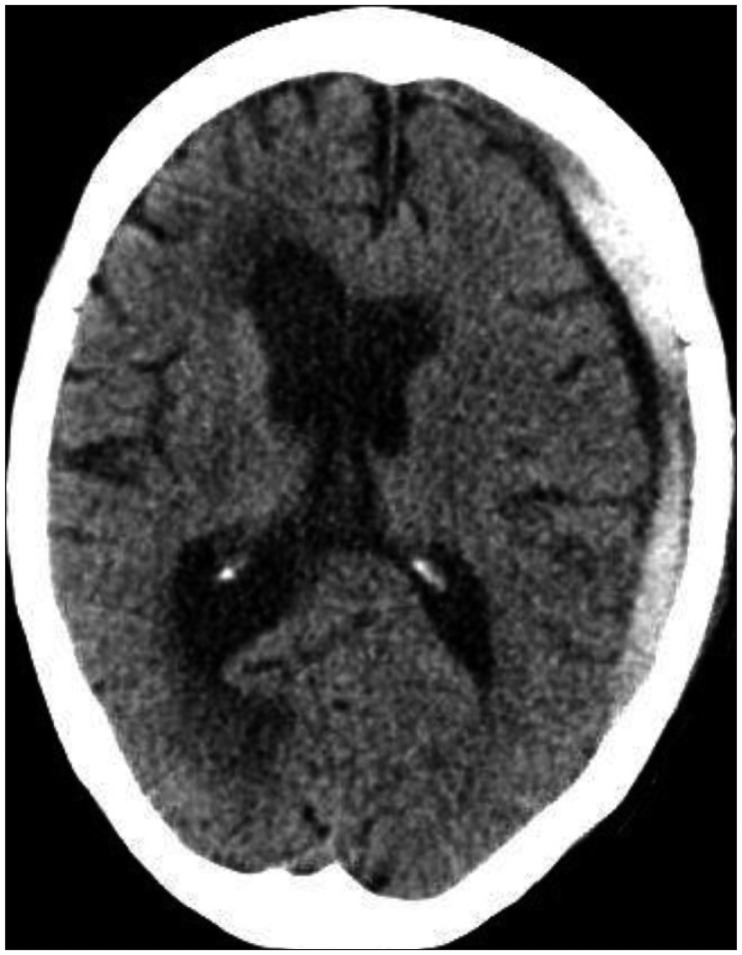
A 90-year-old female patient was admitted to our medical center due to a mental change. The patient was in a stuporous state, and Glasgow coma scale (GCS) was checked by E2M5V1. She had experienced a head injury two months before the admission, and a post-traumatic computed tomography (CT) scan performed immediately after trauma indicated chronic SDH in the left hemisphere (Figure 1A). Although she had no neurologic symptoms at first, symptoms such as dysphagia and right-sided weakness gradually appeared. The follow-up brain CT scan showed increase in volume of the hematoma at the left hemisphere (Figure 1B). She got the burr hole trephination with closed drainage in the left parietal area under the general anesthesia. Follow-up CT scan performed the day after the surgery revealed well-drained chronic SDH (Figure 2A). Her right side motor weakness improved after surgery and GCS was checked by E3M6V3. On day 3 after surgery, the patient abruptly showed stuporous mentality and CT scan revealed acute hematoma inside a cavity of chronic SDH with the midline shift toward the right (Figure 2B). The CT image indicated newly development acute SDH over the pre-existing chronic SDH cavity. Her family did not want more surgical treatment because of her age, and they wanted conservative therapy. We decided to liquefy and drain the solid hematoma by urokinase irrigation using the existing closed drainage system. 17,000 IU of urokinase was injected into the hematoma cavity once daily for 2 days and clamped for 30 minutes. The total drainage volume was 183 mL for two days, and only a small amount of residual hematoma was observed in the CT scan performed two days after irrigation (Figure 3). The patient made a remarkable recovery and had little neurological deficit. GCS was checked by E4M6V4 when discharged. A two-month follow-up CT scan indicated excellent brain re-expansion (Figure 4).
The number of elderly patients who are diagnosed with acute SDH or chronic SDH due to head trauma is increasing with the growth of elderly population. Despite advances in surgical and anesthetic techniques, the outcome of surgery for head trauma in the elderly is very poor because body's ability to maintain homeostasis decreases with aging, and various underlying diseases easily lead to complex systemic complication.817) Thus, careful selection and precise judgment are important in determining surgical treatment.
A weak physical condition or low physiological reserve due to aging cannot be a contraindication to surgery.3) These factors rather delay operation, and such postponement rather increases the postoperative mortality rate in elderly patients. Often, guardians refuse craniotomy of elderly patients diagnosed with acute SDH and prefer conservative treatment even in the situation where the surgery is desperately needed because of the prejudice that old man may not tolerate brain surgery. In such cases delayed surgery, performed as last resort, depletes patient's recuperative, so it is not helpful at all for patient. When it is hard to persuade guardians, we believe that burr hole drainage of hematoma using urokinase is an option of treatment for patients with acute SDH.
In acute SDH, the hematoma should be removed immediately by craniotomy if the neurological condition gets worse with increase in intracranial pressure due to large size of hematoma, or if the thickness of the hematoma is more than 10 mm with midline shift more than 5 mm.2) It is difficult to drain the hematoma through burr hole because hematoma becomes solid in acute SDH unlike chronic SDH which contains liquid contents.916) Craniotomy should be considered for patient with thick, wide acute hematoma, but it may develop complications due to long surgical hours, general anesthesia, profuse bleeding, etc. Especially, it may be hard for elderly patient to undergo craniotomy who has high risk associated with general anesthesia due to underlying diseases or clotting problem due to antiplatelets or anticoagulants use.14) Rather, burr hole hematoma drainage with urokinase may be considered for those limited situations if the patient shows mild neurologic disorder and does not have high intracranial pressure.
Burr hole hematoma drainage with urokinase is commonly used as safe method to lower intracranial pressure or remove hematoma due to acute intracerebral hematoma or acute intraventricular hemorrhage.46) Treatment of chronic SDH or traumatic epidural/subdural hematoma which does not require emergency craniotomy with urokinase through burr hole shows good result as well.151011) Since this method slowly dissolves hematoma, the expansion of the contralateral lesion caused by craniotomy can be prevented as well as rebleeding and pneumocephalus. The disadvantage, however, is that it takes effort to dissolve hematoma using urokinase and patient's recovery pace is slow.
The rate of recovery after burr hole surgery of chronic SDH is high, but postoperative complications often occur. The common complications after chronic SDH surgery are acute SDH and tension pneumocephalus. Additionally, subarachnoid hemorrhage, supratentorial hemorrhage, intracerebral hemorrhage, intraventricular hemorrhage, and remote cerebellar hemorrhages may occur rarely.12) The most common complication in recent studies is acute SDH. It seems to be the result of direct flow of fresh blood from the scalp injury into the subdural space.13)
In this case report, the patient was admitted for chronic SDH and treated with burr hole surgery after which acute SDH occurred as postoperative complication. Although her family wanted conservative therapy, we removed the hematoma with urokinase and achieved good outcome. In limited cases where acute SDH develops as complication after drainage of chronic SDH, urokinase irrigation may be used if the patient has a few neurological change or is not in good physical condition for craniotomy.
Although this is a case report of only one patient, we believe that burr hole drainage of hematoma with urokinase is effective minimally invasive treatment which can be safely performed in patients with acute or subacute subdural hematoma as reported in other studies. We believe that this surgical approach is a good choice for patients who have risk of complication from general anesthesia or have family pessimistic about surgery. Safety and result of procedure should be further analyzed in near future with more cases through clinical experiences.
References
1. Arginteanu MS, Byun H, King W. Treatment of a recurrent subdural hematoma using urokinase. J Neurotrauma. 1999; 16:1235–1239. PMID: 10619201.

2. Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW, et al. Surgical management of acute subdural hematomas. Neurosurgery. 2006; 58:S16–S24. PMID: 16710968.

3. Cagetti B, Cossu M, Pau A, Rivano C, Viale G. The outcome from acute subdural and epidural intracranial haematomas in very elderly patients. Br J Neurosurg. 1992; 6:227–231. PMID: 1632921.

4. Chen X, Chen W, Ma A, Wu X, Zheng J, Yu X, et al. Frameless stereotactic aspiration and subsequent fibrinolytic therapy for the treatment of spontaneous intracerebral haemorrhage. Br J Neurosurg. 2011; 25:369–375. PMID: 20874455.

5. Cho JH, Kang DG, Lee CR, Kim SC. The use of urokinase in treatment of epidural hematoma. J Korean Neurosurg Soc. 1992; 21:1080–1087.
6. Gaberel T, Montagne A, Lesept F, Gauberti M, Lemarchand E, Orset C, et al. Urokinase versus alteplase for intraventricular hemorrhage fibrinolysis. Neuropharmacology. 2014; 85:158–165. PMID: 24846802.

7. Izumihara A, Yamashita K, Murakami T. Acute subdural hematoma requiring surgery in the subacute or chronic stage. Neurol Med Chir (Tokyo). 2013; 53:323–328. PMID: 23708224.

8. Jacobs DG. Special considerations in geriatric injury. Curr Opin Crit Care. 2003; 9:535–539. PMID: 14639075.

9. Kenning TJ, Dalfino JC, German JW, Drazin D, Adamo MA. Analysis of the subdural evacuating port system for the treatment of subacute and chronic subdural hematomas. J Neurosurg. 2010; 113:1004–1010. PMID: 20509728.

10. Liu W, Ma L, Wen L, Shen F, Sheng H, Zhou B, et al. Drilling skull plus injection of urokinase in the treatment of epidural haematoma: a preliminary study. Brain Inj. 2008; 22:199–204. PMID: 18240049.

11. Lu T, Guan J, An C. Preoperative trepanation and drainage for acute subdural hematoma: Two case reports. Exp Ther Med. 2015; 10:225–230. PMID: 26170939.

12. Modesti LM, Hodge CJ, Barnwell ML. Intracerebral hematoma after evacuation of chronic extracerebral fluid collections. Neurosurgery. 1982; 10:689–693. PMID: 7110541.

13. Mori K, Maeda M. Surgical treatment of chronic subdural hematoma in 500 consecutive cases: clinical characteristics, surgical outcome, complications, and recurrence rate. Neurol Med Chir (Tokyo). 2001; 41:371–381. PMID: 11561347.

14. Rohde V, Uzma N, Rohde I, St Clair E, Samadani U. Fibrinolytic therapy versus craniotomy for anticoagulant-associated intracerebral hemorrhage. Clin Neurol Neurosurg. 2009; 111:518–522. PMID: 19297083.

15. Son S, Yoo CJ, Lee SG, Kim EY, Park CW, Kim WK. Natural course of initially non-operated cases of acute subdural hematoma: the risk factors of hematoma progression. J Korean Neurosurg Soc. 2013; 54:211–219. PMID: 24278650.
16. Takeuchi S, Takasato Y, Otani N, Miyawaki H, Masaoka H, Hayakawa T, et al. Subacute subdural hematoma. Acta Neurochir Suppl. 2013; 118:143–146. PMID: 23564121.

17. Yoon SM, Lee KS, Lee JH, Doh JW, Bae HG, Yun IG. Surgical outcome following evacuation of traumatic intracranial hematomas in the elderly. J Korean Neurosurg Soc. 2003; 33:477–482.
FIGURE 1
(A) The initial computer tomography (CT) scan performed immediately after the trauma shows isodense subdural hematoma at the left frontotemporoparietal convexity. (B) At admission, CT scan shows low dense subdural hematoma at the left convexity.
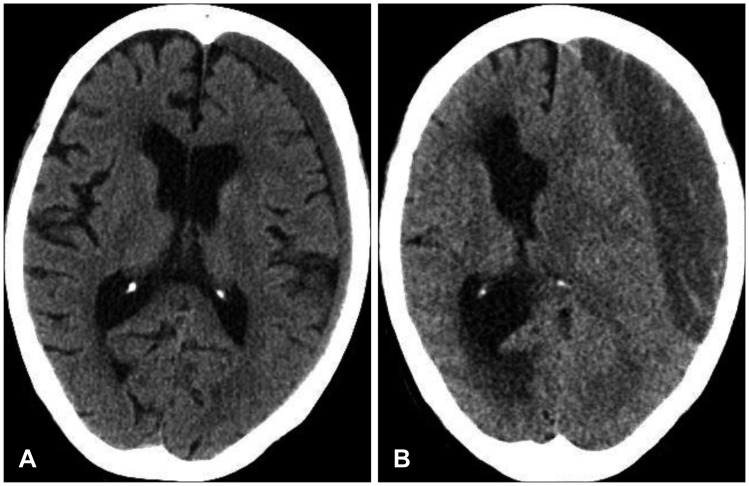
FIGURE 2
(A) Computer tomography (CT) image on the day after the burr hole surgery shows that the chronic subdural hematoma (SDH) was partially drained. (B) Aggravation of symptoms occurred on postoperative day 3. The follow-up CT scan shows newly developed acute subdural hematoma over the chronic SDH.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download