Abstract
Cranial nerve palsies are relatively common after trauma, but trochlear nerve palsy is relatively uncommon. Although traumatic trochlear nerve palsy is easy to diagnose clinically because of extraocular movement disturbances, radiologic evaluations of this condition are difficult to perform because of the nerve's small size. Here, we report the case of a patient with delayed traumatic trochlear nerve palsy associated with a traumatic subarachnoid hemorrhage (SAH) and the related radiological findings, as obtained with high-resolution three-dimensional (3D) magnetic resonance imaging (MRI). A 63-year-old woman was brought to the emergency room after a minor head trauma. Neurologic examinations did not reveal any focal neurologic deficits. Brain computed tomography showed a traumatic SAH at the left ambient cistern. The patient complained of vertical diplopia at 3 days post-trauma. Ophthalmologic evaluations revealed trochlear nerve palsy on the left side. High-resolution 3D MRI, performed 20 days post-trauma, revealed continuity of the trochlear nerve and its abutted course by the posterior cerebral artery branch at the brain stem. Chemical irritation due to the SAH and the abutting nerve course were considered causative factors. The trochlear nerve palsy completely resolved during follow-up. This case shows the usefulness of high-resolution 3D MRI for evaluating trochlear nerve palsy.
Trochlear nerve palsy is an infrequent finding in the case of cranial nerve injuries after minor head trauma.51114) It can result from trauma because of its close proximity to the tentorial incisura and the long course of the nerve in the subarachnoid space.5614) The trochlear nerve palsy results in diplopia, which is secondary to the vertical and horizontal deviation, and occasional torsional difficulty.14) Although clinically noticeable because of the disturbance in extraocular movement, diagnosis of traumatic trochlear nerve palsy using imaging is not easy because of the small size of the nerve.19) The presented case shows delayed traumatic trochlear nerve palsy that developed after a traumatic subarachnoid hemorrhage (SAH) and demonstrates the usefulness of high-resolution three-dimensional (3D) magnetic resonance imaging (MRI) in evaluation and prognosis.
A 63-year-old female was brought to the emergency room for a head trauma after slipping and falling down. She had experienced brief loss of consciousness that lasted for 3 minutes; but later, she could not remember what had happened. A computed tomography (CT) scan of the brain taken at the emergency room revealed a small amount of SAH in the left ambient cistern (Figure 1A). The SAH was considered to be of traumatic origin. There was no definite focal neurological deficit at the initial evaluation except for mild dullness. She was hospitalized for close observation and conservative care.
She recovered from dullness at the hospital on day 1 and showed no neurological deterioration. An electroencephalogram, an echocardiogram, and Holter monitoring were performed to determine the cause of her sudden collapse. There was no specific finding from those tests. However, on day 3 at the hospital, she complained of diplopia, which was intensified on downward gaze. A neurological evaluation revealed trochlear nerve palsy on the left side (Figure 2). Although a follow-up CT evaluation showed resolution of the SAH, the diplopia showed no definite improvement (Figure 1B). She was discharged from the hospital on day 5 with stable condition except for the diplopia.
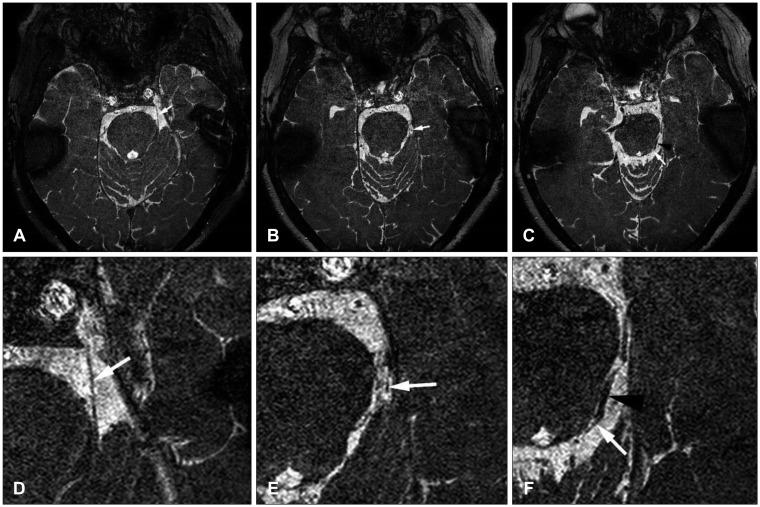
A brain MRI was performed 20 days after the trauma using a 3.0 Tesla MRI (Achieva 3.0T; Philips Medical Systems, Best, the Netherlands). After acquisition of conventional T2-weighted images in the axial and coronal planes, high-resolution 3D imaging was performed for detection of the cranial nerve (volume isotropic turbo-spin-echo acquisition technique, repetition time 10.5; echo time 5.3, 0.3 mm thickness). The MRI showed continuity of the left trochlear nerve without any change in contour. However, it was abutted by the posterior cerebral artery (PCA) branch at the brain stem (Figure 3). No aneurysm or other vascular abnormality was detected in the brain MRI. There was no definite enhancement of the trochlear nerve.
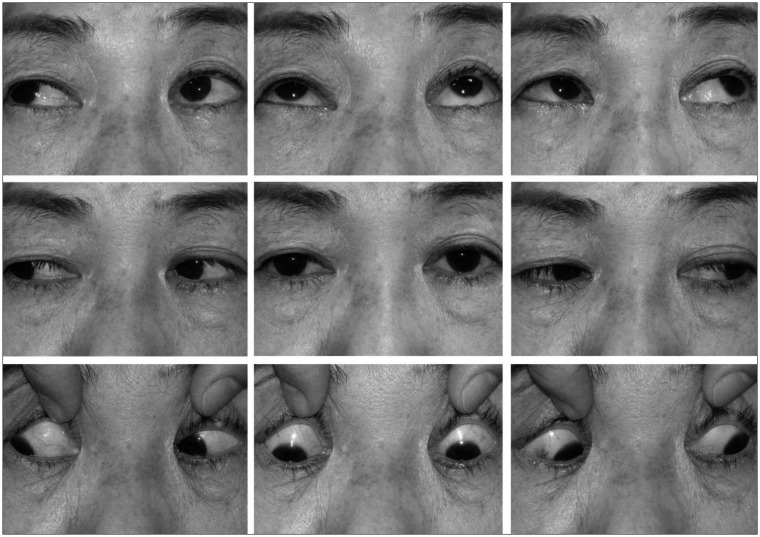
On follow-up ophthalmological examination 1 month after trauma, there was no definite improvement in the trochlear nerve palsy. It was slightly improved at 2 months after trauma and completely resolved at 5 months after trauma (Figure 4).
The trochlear nerve has a long intracranial course of about 60 mm and a very narrow diameter (0.75–1 mm).17) It can be divided into four segments: central, cisternal, cavernous, and orbital.10) The cisternal segment involved in this case. There are three sub-segments of the cisternal segment of the trochlear nerve: quadrigeminal, ambient, and tentorial.11519) The trochlear nerve exits the brain stem posteriorly, immediately below the inferior colliculus. It then rounds the cerebral peduncles in the ambient cistern, coursing (along with the oculomotor nerve) between the superior cerebellar artery and the PCA, and pierces the dura between the free and attached edge of tentorium cerebelli.319)
The mechanisms of trochlear nerve injury can be direct or indirect. The trochlear nerve can be affected by tumors, infections, vascular disorders, inflammatory disorders, or toxic substances.3) Trochlear nerve palsy may be caused by trauma because of its anatomy as mentioned above. It is suggested that ophthalmoplegia is caused by a contrecoup contusion against the delicate attachment of the trochlear nerve at the medullary velum with subsequent avulsion to the fourth nerve rootlets after a sudden speed deceleration or a blow to the forehead.714) Although clinically obvious, it is not easy to evaluate trochlear nerve palsy by conventional MRI technique. With high-resolution 3D MR sequences, it has become possible to get more precise imaging of the cranial nerves.2419) It has been reported that abnormal thickness, compression by vascular lesions, avulsion of roots, and hypoplasia of the nerve can be detected by MRI.69)
Our case has a unique point compared to previously reported cases. The initial CT scan showed a traumatic SAH at the left ambient cistern, but there was no clinical sign of trochlear nerve palsy at initial ophthalmologic exam. In a high-resolution 3D image taken 20 days after trauma, the trochlear nerve showed continuity without any change in contour except where it abuts the PCA branch at the brain stem. There are reported cases of immediate trochlear nerve palsy after various traumata.58) However, delayed trochlear nerve palsy associated with traumatic SAH has not been reported yet.
The perimesencephalic cistern is not an uncommon location for traumatic SAH,18) however not everyone who has perimesencephalic SAH has trochlear nerve palsy. In this case, high-resolution 3D MRI shows anatomic variation of the tight course of the trochlear nerve abutted by the PCA branch. It is speculated that chemical irritation due to products of degradation from the SAH superimposed on the tight course of the nerve resulted in delayed trochlear nerve palsy. When the blood clot in the subarachnoid space lyses, hemoglobin can induce neuronal apoptosis, decrease nitric oxide levels, increase endothelin-1 levels, and increase the amount of peroxide free-radicals.1213) A vasospasm of perforating vessel of PCA might play a role in the development of delayed palsy. However, the time of onset of symptoms is earlier than the usual period of vasospasm, which usually presents from day 3 to day 14 after the SAH.12) The small size of the trochlear nerve might conceal the possible contour and enhancement change caused by chemical irritation. Considering the clinical course of trochlear nerve palsy, it is unlikely to be caused by adhesion resulting from traumatic SAH.
Typically, the mainstay of treatment is observation and follow-up in cases without any pathologic findings. Most patients recover completely over a time course of 10 days to 2 months after onset.11) Our case showed a more protracted clinical course. The MRI also helps us predict the likelihood of recovery from trochlear nerve palsy, as long as the course of the nerve is intact. It has been reported that lesions involving nerve roots or the motor nucleus of the brain stem show poor functional recovery compared to injuries that preserve continuity of the peripheral segment of the nerve.16)
In this particular case, it is speculated that the combination of the anatomic variation of the trochlear nerve and chemical irritation after a traumatic SAH might have caused temporary trochlear nerve palsy. High-resolution 3D MRI is very useful for localization of pathology and for assessment of the prognosis for functional recovery. High-resolution 3D MRI could be an extremely useful imaging modality to help physicians arrive at a diagnosis in a variety of situations involving cranial nerves, as shown in our case.
References
1. Ammirati M, Musumeci A, Bernardo A, Bricolo A. The microsurgical anatomy of the cisternal segment of the trochlear nerve, as seen through different neurosurgical operative windows. Acta Neurochir (Wien). 2002; 144:1323–1327. PMID: 12478346.
2. Borges A, Casselman J. Imaging the cranial nerves: Part I: methodology, infectious and inflammatory, traumatic and congenital lesions. Eur Radiol. 2007; 17:2112–2125. PMID: 17323090.

3. Burger LJ, Kalvin NH, Smith JL. Acquired lesions of the fourth cranial nerve. Brain. 1970; 93:567–574. PMID: 4319184.

4. Choi BS, Kim JH, Jung C, Hwang JM. High-resolution 3D MR imaging of the trochlear nerve. AJNR Am J Neuroradiol. 2010; 31:1076–1079. PMID: 20093316.

5. Coello AF, Canals AG, Gonzalez JM, Martín JJ. Cranial nerve injury after minor head trauma. J Neurosurg. 2010; 113:547–555. PMID: 20635856.

6. Eisenkraft B, Ortiz AO. Imaging evaluation of cranial nerves 3, 4, and 6. Semin Ultrasound CT MR. 2001; 22:488–501. PMID: 11770928.

7. Hara N, Kan S, Simizu K. Localization of post-traumatic trochlear nerve palsy associated with hemorrhage at the subarachnoid space by magnetic resonance imaging. Am J Ophthalmol. 2001; 132:443–445. PMID: 11530077.

8. Hoya K, Kirino T. Traumatic trochlear nerve palsy following minor occipital impact-four case reports. Neurol Med Chir (Tokyo). 2000; 40:358–360. PMID: 10927902.
9. Kim JH, Hwang JM. Hypoplastic oculomotor nerve and absent abducens nerve in congenital fibrosis syndrome and synergistic divergence with magnetic resonance imaging. Ophthalmology. 2005; 112:728–732. PMID: 15808269.

10. Laine FJ. Cranial nerves III, IV, and VI. Top Magn Reson Imaging. 1996; 8:111–130. PMID: 8784967.

11. Li G, Zhu X, Gu X, Sun Y, Gao X, Zhang Y, et al. Ocular movement nerve palsy after mild head trauma. World Neurosurg. 2016; 94:296–302. PMID: 27422684.

12. Macdonald RL, Pluta RM, Zhang JH. Cerebral vasospasm after subarachnoid hemorrhage: the emerging revolution. Nat Clin Pract Neurol. 2007; 3:256–263. PMID: 17479073.

13. Macdonald RL, Weir BK. A review of hemoglobin and the pathogenesis of cerebral vasospasm. Stroke. 1991; 22:971–982. PMID: 1866764.

14. Mansour AM, Reinecke RD. Central trochlear palsy. Surv Ophthalmol. 1986; 30:279–297. PMID: 3520909.

15. Marinković S, Gibo H, Zelić O, Nikodijević I. The neurovascular relationships and the blood supply of the trochlear nerve: surgical anatomy of its cisternal segment. Neurosurgery. 1996; 38:161–169. PMID: 8747965.

16. Richards BW, Jones FR Jr, Younge BR. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am J Ophthalmol. 1992; 113:489–496. PMID: 1575221.

17. Villain M, Segnarbieux F, Bonnel F, Aubry I, Arnaud B. The trochlear nerve: anatomy by microdissection. Surg Radiol Anat. 1993; 15:169–173. PMID: 8235957.

18. Wu Z, Li S, Lei J, An D, Haacke EM. Evaluation of traumatic subarachnoid hemorrhage using susceptibility-weighted imaging. AJNR Am J Neuroradiol. 2010; 31:1302–1310. PMID: 20190211.

19. Yousry I, Moriggl B, Dieterich M, Naidich TP, Schmid UD, Yousry TA. MR anatomy of the proximal cisternal segment of the trochlear nerve: neurovascular relationships and landmarks. Radiology. 2002; 223:31–38. PMID: 11930045.

FIGURE 1
Initial computed tomography (CT). (A) The subarachnoid hemorrhage (SAH) at the left ambient cistern (arrow). (B) A follow-up CT taken 6 days later that shows resolution of the SAH.
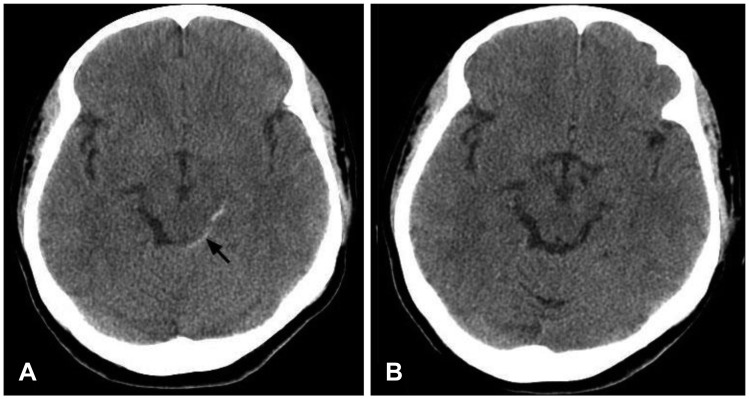
FIGURE 2
Nine-gaze photograph taken 1 week after injury that shows underaction of the left superior oblique muscle and mild overaction of the left inferior oblique muscle. The deviation is greatest when the patient was looking up and to the right (arrow 1), left hypertropia in primary position (arrow 2), overelevation in adduction (arrow 3), and limitation of depression when looking down and to the right (arrow 4).
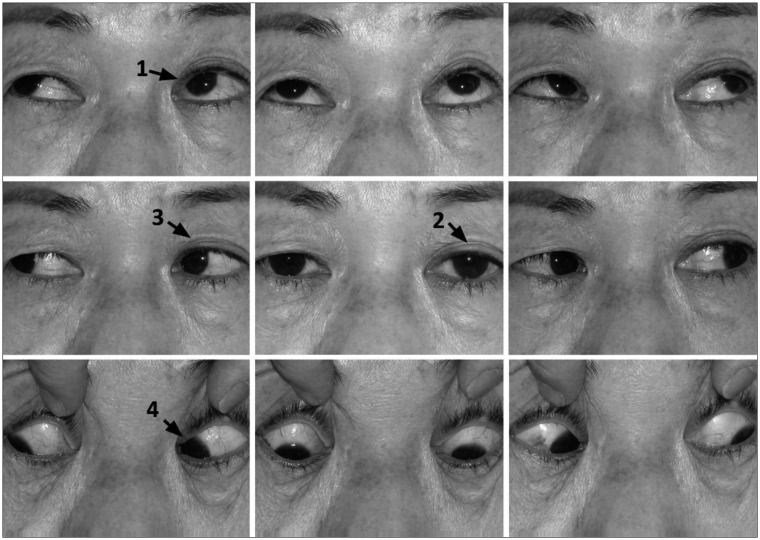
FIGURE 3
(A–F) High-resolution three dimensional magnetic resonance imaging, taken 20 days after trauma, shows continuity of the left trochlear nerve (white arrows) without any change in contour. It was abutted by the posterior cerebral artery branch (black arrow head) at the brain stem. (D–F) are magnified views of (A–C) for clearer demonstration of details (volume isotropic turbo-spinecho acquisition technique, repetition time 10.5, echo time 5.3, 0.3 mm thickness).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download