Abstract
Objective
The purpose of this study was to analyze the risk factors for hinge fracture (HF) and non-union during cervical open-door laminoplasty (CODL).
Methods
We included 25 patients who underwent CODL with available serial computed tomography scans acquired at 2 days and 1 year postoperatively. Patients' medical records and radiographic data were reviewed. Risk factors related to the surgical procedures were evaluated including the lamina angle, spinous angle, difference in the lamina angle, outer cortex location (OCL), and inner cortex location.
Results
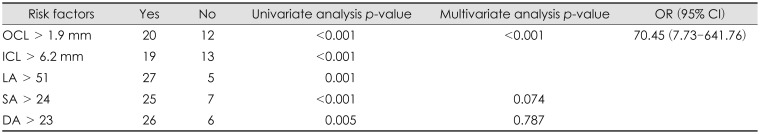
There were a total of 76 hinges. Of these, 44 laminae were classified as deformed hinges, and 32 were classified as fragmented hinges. Additionally, 66 laminae were healed completely, and 10 laminae were not healed by 12 months postoperatively. The OCL (odds ratio, 70.45; 95% confidence interval, 7.73–641.76) was identified as a predictor of HFs immediately following CODL. However, none of the factors we evaluated was related to hinge non-union.
Cervical open-door laminoplasty (CODL) is the standard surgical option for patients with multilevel cervical compressive myelopathy.29) The basic principle of laminoplasty have included linear laminectomy on one side and making greenstick deformation of opposite side laminas.19) These deformed laminas were called as hinges. The initial technique for laminoplasty had some problem such as lamina reclosure or hinge fractures (HFs).4) Therefore, new technique to fix the laminectomy side with titanium miniplates had been proposed and used widespread.57) Nevertheless, HFs had been reported.15) Some authors had been reported that HFs might be related with chronic neck pain or palsy, and had analyzed risk factors associated with HFs.356) However, there was few studies about surgical techniques related with HFs. The purpose of this study was to determine risk factors of HFs and surgical techniques for preventing HFs after CODL.
We included 25 patients (18 men, 7 women) who underwent open-door laminoplasty with available serial computed tomography (CT) scans at postoperative 2 days and a year. Medical records and radiographic data were reviewed after approval of Institutional Review Board. The mean age of patients at surgery was 62.7 years (range, 43–79 years).
We used a standard posterior approach of the cervical spine for open-door laminoplasty. The number of segments depended on the extension of spinal cord compression. At first, the junction of the lateral mass and lamina was drilled with a 3-mm burr under the microscope. Linear laminectomy was made and the ligament flavum was splitted with a Kerrison rongeur. Then, on the opposite side, removing the dorsal cortex and thinning the ventral cortex was performed until a greenstick deformation of the hinge. Laminas were elevated and the open side was stabilized with plates and screws (Arch; Synthes, Paoli, PA, USA). Bone grafting was not performed near the hinge. We tried that ventral cortex of lamina on hinge side was preserved, but some hinges were fragmented during drilling. These fragmented laminae to be identified via the microscope were excluded in this study.
The initial status of hinges on postoperative 2 days CT scans were classified as two groups: ‘Deformed’ and ‘Fractured’. ‘Deformed’ defined that the ventral cortex remained intact and mean favorable greenstick deformation. ‘Fractured’ defined that the ventral cortex was broken and mean unfavorable greenstick deformation. And healing status of hinges was determined by evaluating the status of each cortex (dorsal and ventral).8) A hinge was defined as being ‘healed’ only if both the dorsal and ventral cortices were bridged by bone. If the ventral cortex had cortical bridging but the dorsal cortex had neither cortical nor cancellous bridging, the hinge was defined as ‘not healed’.8)
Factors related with surgical procedures included lamina angle (LA), spinous angle (SA), difference of lamina angle (DA), and hinge location. For LA and SA, virtual line crossing over posterior lateral mass was made. SA was defined as the angle between the parallel line to spinous process and the perpendicular line to virtual line crossing both lateral mass posteriorly. LA was defined as the angle between parallel line to the hinge side lamina and virtual line crossing both lateral mass posteriorly. Hinge location was divided to outer and inner cortex of the lamina. Outer cortex location (OCL) was defined as the distance from medial cortex of the pedicle to lateral wall of hinge gutter. Inner cortex location (ICL) was defined as the distance from medial cortex to the pedicle to midline of inner cortex of hinge gutter (Figure 1).
Statistical analysis was performed using SPSS statistical software package 18.0 for Windows (SPSS Inc., Chicago IL, USA). The independent t-test was used to compare quantitative data and evaluate the statistical significance, which was set at the p=0.05 level. For evaluating predictive factors associated with HF and nonunion, receiver-operating characteristics (ROC) curve was analyzed and 95% confidence interval (CI) was calculated. Cut off value was determined maximized value in sum of sensitivity and specificity. To identify variables independently related to HF and nonunion, univariate and multivariate logistic regression analysis were used.
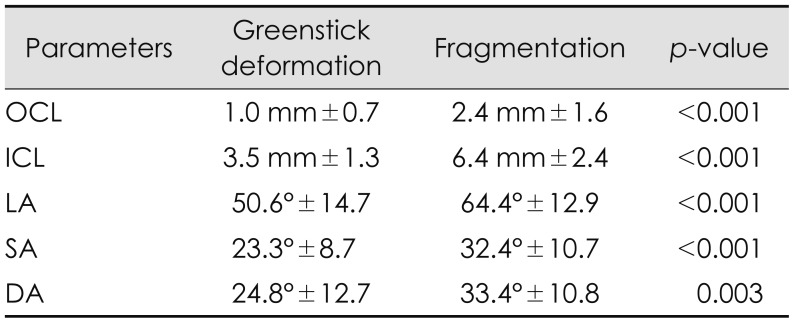
A total of 76 laminae from 25 patients were evaluated. In postoperative 2 days CT scans, 44 laminae were classed as deformed hinges, and 32 were classed as fragmented hinges. 66 laminae were healed completely, and 10 laminae were not healed on postoperative 12 months. The mean LA, SA, and DA were 56.4±15.5 (range, 18.8–82), 27.2±10.5 (range, 10.4–57), and 28.4±12.6 (range, 3.1–60.2) degrees. The average OCL and ICL were 1.6±1.4 (range, 0–5.9) and 4.7±2.4 (range, 0.9–11.5) mm, respectively.
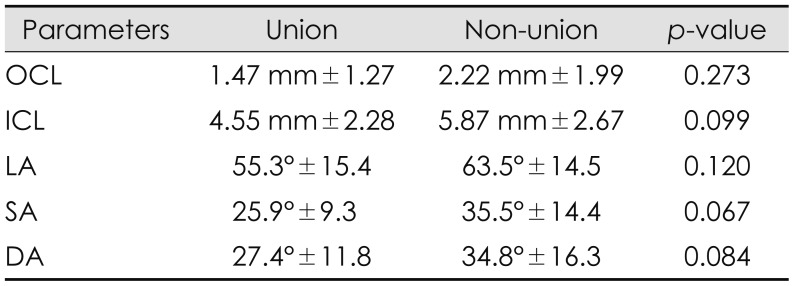
Factors related with surgical procedure had statistical significance between deformed and fractured hinge group. In fractured group, mean LA, SA, DA, OCL, and ICL were higher than deformed group (Table 1). The ROC curves were used for proper cut off value of fractured hinge. When OCL was over 1.9 mm, the area of fractured hinge group was largest. The area was 0.774 (p<0.001; 95% CI, 0.663–0.862). Sensitivity was 62.5% and specificity was 97.73%. When ICL was over 6.2 mm, the area of fractured hinge group was largest. The area was 0.851 (p<0.001; 95% CI, 0.751–0.922). Sensitivity was 59.38% and specificity was 100%. When LA was over 51 degrees, the area of fractured hinge group was largest. The area was 0.760 (p<0.001; 95% CI, 0.648–0.851). Sensitivity was 59.38% and specificity was 100%. When SA was over 24.18 degrees, the area of fractured hinge group was largest. The area was 0.752 (p<0.001; 95% CI, 0.640–0.844). Sensitivity was 78.12% and specificity was 65.91%. When DA was over 23.34 degrees, the area of fractured hinge group was largest. The area was 0.699 (p=0.001; 95% CI, 0.583–0.799). Sensitivity was 81.25% and specificity was 52.27% (Figure 2). Multivariate logistic regression analysis were used to identify risk factor for fractured hinge. OCL (odds ratio, 70.45; 95% CI, 7.73–641.76) was identified as a predictor of hinge fragmentation (Table 2). On the other hand, there was no statistical difference between healed and not healed hinge group (Table 3).
Surgical procedures of CODL were composed of linear laminectomy, making hinges, elevation of lamina, and fixation.4) The laminectomy did not influence to hinge status because hinges were made on the opposite site of laminectomy. Fixation of lamina was achieved with miniplates recently, and there was no implant failure in our series. Therefore, the fixation did not affect to hinge status. Process of making hinge gutters and degree of lamina elevation may affect hinge status in CODL. Locations, widths and types of drill burr could be varied during making hinge gutters. In our series, drill burrs for making gutter were same, so, widths of gutters also were same. Therefore, we chose gutter location and degree of lamina elevation as risk factors related with HFs.
Hinge gutter location proposed to be an important risk factor for HF.45) In our study, medially placed hinge over 1.9 mm from pedicle had significant p-value in multivariate logistic regression analysis and high OR. This means that the medially positioned hinge tends to break easily. The reason might be related the thickness of bone. Medial portion of laminar is generally thinner than lateral portion.5) Thin hinge may be weak and easily break during handling.
In our series, univariate analysis indicated that wide angle of elevated lamina leaded to HF. Hur et al.5) also reported that open angle and initial hinge status might be correlated with each other. Wide angle might make the hinge gutter more stressful, which could induce fragmentation of the hinge. However, in multivariate analysis, there was no statistical significance in both studies.5) We did not perform multivariate analysis using ICL and LA because these factors could not calculate intraoperatively.
There was no statistical significance between these surgical variables and hinge healing status on postoperative 12 months in this study. On the other hands, Hur el al.5) reported that medial hinge location was important risk factor for delayed HF in both univariate and multivariate logistic regression analyses. However, they defined delayed HF as abnormal hinge status after postoperative 4 months. In generally, the healing rates of hinges increased as time went on. On postoperative 6 months, rates were reported from 57.4% to 80%, but rates had been known over 85% on postoperative 12 months.368) Therefore, delayed HF in Hur's study might change to healed status. And because the healing rate of hinge gutter was high, nonunion might be irrelevant to surgical techniques. Larger studies needed to determine exact risk factors. And, for sufficient decompression, large angle must be made intraoperatively because angle was not related with hinge nonunion.
References
1. Byard RW, Langlois N, Gilbert JD. Positive “water test”-an external indicator of base of skull hinge-ring fracture. J Forensic Sci. 2010; 55:519–520. PMID: 20102468.

2. Chen H, Liu H, Zou L, Li T, Gong Q, Song Y, et al. Effect of miniplate fixation on hinge fracture and bony fusion in unilateral open-door cervical expansive laminoplasty. Clin Spine Surg. 2016; 29:E288–E295. PMID: 25023712.

3. Cho SH, Lee JH, Chough CK, Joo WI, Park HK, Lee KJ, et al. Hinge Fracture during Cervical Open-door Laminoplasty: Does it Affect Clinical and Radiographic Outcomes? Korean J Spine. 2014; 11:45–51. PMID: 25110482.

4. Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine (Phila Pa 1976). 1988; 13:870–876. PMID: 3143157.

5. Hur JW, Park YK, Kim BJ, Moon HJ, Kim JH. Risk factors for delayed hinge fracture after plate-augmented cervical open-door laminoplasty. J Korean Neurosurg Soc. 2016; 59:368–373. PMID: 27446518.

6. Lee S, Chung CK, Kim CH. Risk factor analysis of hinge fusion failure after plate-only open-door laminoplasty. Global Spine J. 2015; 5:9–16. PMID: 25648062.

7. O'Brien MF, Peterson D, Casey AT, Crockard HA. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization. A computerized morphometric analysis. Spine (Phila Pa 1976). 1996; 21:474–483. PMID: 8658252.
8. Rhee JM, Register B, Hamasaki T, Franklin B. Plate-only open door laminoplasty maintains stable spinal canal expansion with high rates of hinge union and no plate failures. Spine (Phila Pa 1976). 2011; 36:9–14. PMID: 21192219.

9. Takeuchi R, Ishikawa H, Kumagai K, Yamaguchi Y, Chiba N, Akamatsu Y, et al. Fractures around the lateral cortical hinge after a medial opening-wedge high tibial osteotomy: a new classification of lateral hinge fracture. Arthroscopy. 2012; 28:85–94. PMID: 21982387.

FIGURE 1
(A) Schematic diagram of the lamina angle (LA) and spinous angle (SA). SA (a) was defined as the angle between the parallel line to spinous process and the perpendicular line to virtual line crossing both lateral mass posteriorly. LA (b) was defined as the angle between parallel line to the hinge side lamina and virtual line crossing both lateral mass posteriorly. (B) Radiographic measurements of hinge gutter location. Inner cortex layer (c) was defined as distance from pedicle to inner cortical bone of hinge, and outer cortex layer (d) was defined as distance from pedicle to outer cortical bone of hinge.
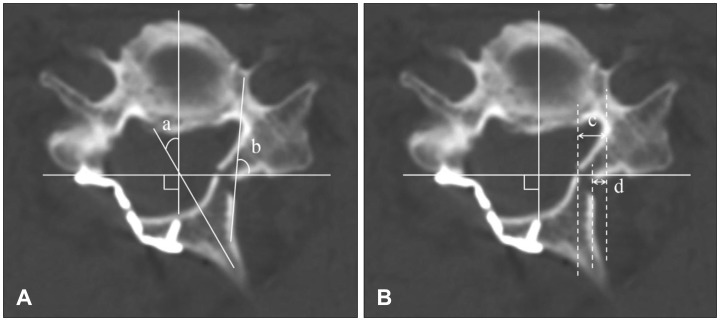
FIGURE 2
Receiver-operating characteristics curves of risk factors. (A) Outer cortex location, (B) inner cortex location, (C) lamina angle, (D) spinous angle, and (E) difference of lamina angle. AUC: area under curve.
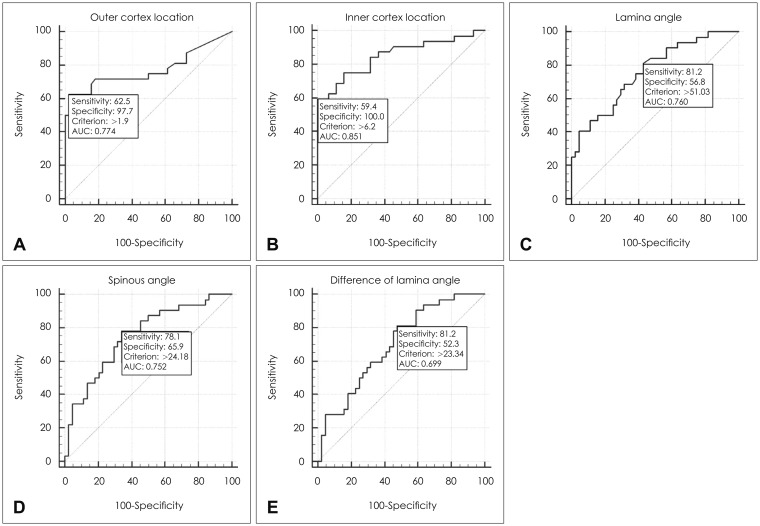
TABLE 1
Comparison of parameters for hinge status between greenstick deformation group and fragmentation group




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download