This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Despite meticulous techniques, surgical complications continue to be problematic in kidney transplant recipients. Role of routine stenting to reduce complications is controversial. In this study, we compare incidence of early urological complications, lymphoceles, urinary tract infections (UTI) and graft function; with or without double-J stenting.
Materials and Methods
All patients who underwent live related donor renal transplantation from February 2014 to February 2016 were included. Transplants prior to February 2015 were without routine stenting; subsequent transplants were with routine stenting. Patients with neurogenic bladder, previously operated bladder and delayed or low urinary output were excluded. Follow-up was for at least three months. Descriptive statistics was performed for all parameters. Chi square test and Fisher's Exact test were used for qualitative variables. For quantitative variables, Mann-Whitney test was used to test median difference and independent samples t-test for mean difference. The p-value ≤0.05 was considered significant.
Results
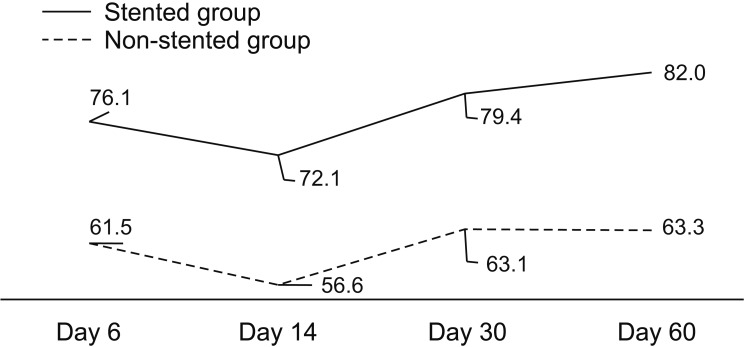
We analysed 74 patients (34 stented and 40 non-stented). There was no difference in the incidence of urinary leak, anastomotic obstruction, lymphoceles or UTI (p>0.4 for all comparisons). However, mean estimated glomerular filtration rate at sixth day, 14th day, one month and two months were 76.1 vs. 61.5 (p=0.025), 72.1 vs. 56.6 (p=0.005), 79.4 vs. 63.1 (p=0.002) and 82.0 vs. 63.3 (p=0.001) in the stented versus non-stented groups.
Conclusions
Placement of ureteral stent in renal transplant does not significantly affect the incidence of early urinary complications or UTI. However, graft function is significantly better in stented recipients, at least in the short term.
Go to :

Keywords: Complications, Kidney transplantation, Stent, Urinary tract infection
INTRODUCTION
Kidney transplant is one of the treatment options for patients with end stage renal disease. It offers a better quality of life than the other common option of dialysis. Despite meticulous surgical techniques and progress in the pre- and postoperative care of kidney transplant recipients, surgical and urological complications continue to be a problem. Early urological complications are defined as urinary leakage or obstruction occurring within the first three months after transplantation. In literature, rates of urological complication range between 0.22% and 14.1%. However, definitions vary and hence an accurate estimation of the incidence is difficult [
12]. They are associated with significant morbidity, prolonged hospital stay, frequent need of a second surgical procedure and occasionally mortality. Ureteral obstruction occurring after renal transplantation can reach an incidence of 4.5%, whereas urinary leaks are recorded in up to 8.9% of cases [
345].
The therapeutic benefits of stents in transplantation are still disputed but may include simplifying the creation of a watertight uretero-neocystostomy and reduction of anatomical kinking [
1]. The most significant theoretical complication is an increase in the number and severity of urinary tract infections (UTI) [
67]. There is still an active debate whether ureteral stenting can lower the urologic complication rates in transplant recipient patients [
1789101112131415]. In certain situations, such as delayed graft function, neurogenic bladders and in previously operated bladders, there is a definite role of stent placement.
At P. D. Hinduja National Hospital and Medical Research Centre, prior to February 2015, we had a policy not to stent transplant recipients, except in the certain situations mentioned above. After February 2015, all patients were stented.
In this study, we have compared the incidence of early urological complications, lymphoceles and UTI, and also graft function in renal transplant recipients; with or without ureteral double-J stenting; at our centre.
Go to :

MATERIALS AND METHODS
All patients who underwent live related donor renal transplant between February 2014 to February 2016 were screened for inclusion in the study. Between February 2014 to January 2015, stents were not put routinely and these patients comprised the non-stented cohort. From February 2015 to February 2016, patients were routinely stented and they formed the stented cohort. The exclusion criteria for this study were as follows:
·Presence of a definite indication for stenting-i.e., those with neurogenic bladder, previous bladder surgery, those with low or delayed post transplant urine output or any other definite indication (since these were stented in both periods of time).
·Immediate postoperative death (within the first 30 days of transplant).
·Lack of consent.
The study was approved by the Institutional Ethics Committee at P. D. Hinduja National Hospital and Medical Research Centre, Mumbai, India (approval number: 933-15-VJ [MRC]). Written informed consent was taken from all patients. Standard preoperative work up was done for patients in both the groups.
1. Surgical technique
All donor and recipient surgeries were performed by same transplantation team. All the surgeons had minimum 15 years of experience in the field, with an average experience of about 25 years. Majority of the receipient surgeries were done by the seniormost surgeon, who has almost 40 years of experience in renal transplants.
Uretero-neocystostomy was done by Lich-Gregoir technique in all patients. The patients in group 1 had a 4 French 12 cm double-J stent placed at time of uretero-vesical anastomosis whereas same technique of anastomosis was done without any stent in group 2.
2. Postoperative care
All the patients were started on standard immunosuppression as per protocol. Clinical evaluation was done regularly and urine output also monitored on hourly basis for the first few days. Daily measurement of renal biochemistry and full blood count was done. All were given injection cefuroxime intravenously twice a day till urethral catheter was removed on sixth postoperative day. After that all the patients received 480 mg co-trimoxazole, if not allergic, for six months as prophylaxis. Those allergic were given fluoroquinolones as prophylaxis. Drain was removed when the drain output was nil or minimal. The stent was removed at four weeks, as a day care procedure using a flexible cystoscope under local anaesthesia.
3. Follow-up and outcome
Early urological mechanical complications are defined as urinary leakage or obstruction occurring within the first three months after transplantation. All patients were followed-up till at least three months after surgery.
Serum creatinine at sixth postoperative day, at 14th postoperative day, at one month (time of stent removal) and at two months postoperatively were recorded and estimated glomerular filtration rate (eGFR) was calculated using ‘Chronic Kidney Disease Epidemiology Collaboration equation’. Urine Routine and midstream urine for culture was sent at the time of catheter removal, at one month (before stent removal), at second month and third month, or in between if clinically indicated. Ultrasonography of transplant kidney was done on sixth postoperative day (on catheter removal), at one month (stent removal), at two months and at three months postoperatively, or in between if clinically indicated. Radioisotope scan, drain fluid creatinine or biopsy was done when clinically indicated. All episodes of urinary leakage, obstruction, UTI, lymphocele, stent related problems and graft rejection were recorded.
Descriptive statistics was performed for all parameters. Normality testing was done using Shapiro-Wilk test. Mann- Whitney test was used to test the median difference for quantitative data in stented vs. non-stented group of patients. Chi-square test and Fisher's Exact test were used for qualitative variables. Independent-samples t-test was used to test the mean difference for quantitative data in stented vs. non-stented group of patients. Statistical analysis was done by IBM SPSS Statistics ver. 20.0 software (IBM Co., Armonk, NY, USA). The level of significance was considered as p≤0.05 (two sided).
Go to :

RESULTS
A total of 121 renal transplants were done between February 2014 to February 2016. Of these 74 met the inclusion - exclusion criteria and were included in the study. Reason for exclusion of the 47 patients were as follows - 13 cadaveric transplants (5 in non stent period and 8 in stent period), 4 immediate postoperative deaths (2 in each period), 12 definite indication for stenting, 6 because of missing records and 12 because of lack of consent.
We analysed 74 patients (34 stented and 40 non-stented). General characteristics of donors and recipients were comparable in both the groups (
Table 1). No patient in either group had graft loss during the study period. There was no significant difference in median hospital stay between the two groups (
Table 1). The median time to stent removal was 30.5 days (range, 9–197 days). Our initial plan was to remove the stent at 4 weeks post-transplantation. In 8 patients stent was removed early (3 patients due to UTI, 1 patient coupled with lymphocele drainage, 1 patient due to younger age and 3 patients wanted to get it removed early because of social reasons). In 2 patients, stent was forgotten and hence removed late. However those 2 patients did not have any other adverse effects in terms of urological complications, UTI, or graft dysfunction. None of the patients had any other stent related complications; like stent dysuria, stent encrustation, stent migration, haematuria, stent obstruction or broken stent.
Table 1
Patient characteristics

|
Variable |
Group 1 (stented) |
Group 2 (non-stented) |
p-value |
|
No. of patients |
34 |
40 |
|
|
Mean recipient age |
38.21 (14–70) |
34.80 (14–67) |
NS |
|
Male/female |
30/4 |
27/13 |
NS |
|
Mean donor age |
47.47 (21–69) |
50.0 (32–65) |
NS |
|
Percentage of left donor nephrectomy |
79.41 |
85 |
NS |
|
Mean donor GFR (mL/min) |
100.13 |
88.78 |
Significant (0.045) |
|
No. of diabetic patients |
7 (20.59) |
7 (17.5) |
NS |

None of the stented patients had urinary leak compared to 2 patients (5.0%) in non-stented group who had urinary leak (p=0.496). One patient was managed with stenting and other patient needed surgical exploration and revision of ureterovesical anastomosis.
One patient (2.5%) of non-stented group developed anastomotic obstruction whereas none in the stented group (p=1.000). The patient who had developed obstruction was treated by antegrade stenting.
In stented group, 3 patients (8.8%) had lymphocele which required intervention in form of formal surgical drainage whereas 4 patients (10.0%) of non-stented patients required surgical drainage of lymphocele (p=1.000).
A total of 23 patients (31.1%) had one or more episodes of UTI. Eleven patients fell in stented group (32.4%) and 12 patients were from non-stented group (30.0%); (p=1.000). Seven patients (9.5%) had symptomatic UTI (either manifesting as dysuria, or other lower urinary symptoms, or fever) out of which 3 patients (8.8%) were from stented group and 4 patients (10.0%) from non-stented group (p=1.000). Three patients (1 patient from group 1 and 2 patients from group 2) required re-admissions for treatment of UTI. The remaining 16 patients had asymptomatic UTI (they had positive urine cultures with colony count of >105, but no symptoms). The most common organism isolated was Escherichia coli. Three of the patients had multiple organisms detected. Both the groups had similar organisms detected in their cultures.
The mean eGFR at postoperative sixth day, 14th day, one month and two months were significantly better for stented transplant recipients than for non-stented transplant recipients (
Table 2,
Fig. 1).
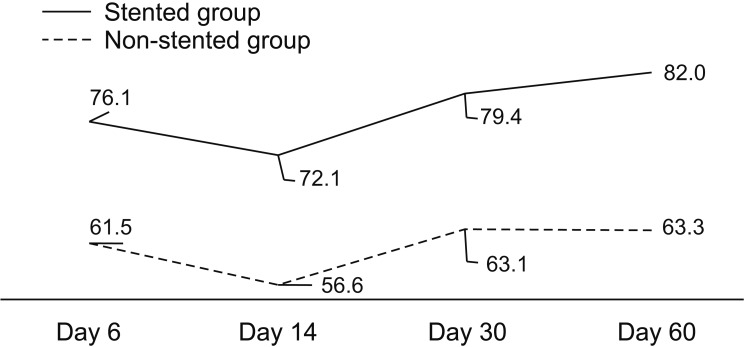 | Fig. 1Mean estimated glomerular filtration rate in stented versus nonstented group at various time points.
|
Table 2
Estimated GFR

|
eGFR |
N |
Mean (mL/min/1.73 m2) |
Standard deviation |
Standard error mean |
p-value |
|
eGFR at 6th postoperative day |
|
|
|
|
|
|
Stented (group 1) |
34 |
76.1 |
28.1 |
4.8 |
0.025 |
|
Non-stented (group 2) |
40 |
61.5 |
26.3 |
4.2 |
|
|
eGFR at 14th postoperative day |
|
|
|
|
|
|
Stented (group 1) |
34 |
72.1 |
25.9 |
4.4 |
0.005 |
|
Non-stented (group 2) |
40 |
56.6 |
19.2 |
3.0 |
|
|
eGFR at 1 month post surgery |
|
|
|
|
|
|
Stented (group 1) |
34 |
79.4 |
23.9 |
4.1 |
0.002 |
|
Non-stented (group 2) |
40 |
63.1 |
19.3 |
3.1 |
|
|
eGFR at 2 months post surgery |
|
|
|
|
|
|
Stented (group 1) |
34 |
82.0 |
25.5 |
4.4 |
0.001 |
|
Non-stented (group 2) |
40 |
63.3 |
17.7 |
2.8 |
|

These results are summarized in
Table 3.
Table 3
Postoperative course in renal transplant recipients

|
Variable |
Stented |
Non-stented |
p-value |
|
No. of patients |
34 |
40 |
|
|
Hospital stay (d) |
14.65±3.5 |
15.18±2.93 |
0.540 |
|
Postoperative drainage (d) |
16.35±9.37 |
14.53±12.90 |
0.217 |
|
Urinary leak |
0 (0.0) |
2 (5.0) |
0.496 |
|
Urinary obstruction |
0 (0.0) |
1 (2.5) |
1.000 |
|
Lymphocele |
3 (8.8) |
4 (10.0) |
1.000 |
|
Stent related complications |
2 (5.9) |
0 (0.0) |
0.208 |
|
UTI |
11 (32.4) |
12 (30.0) |
1.000 |
|
Symptomatic UTI |
3 (8.8) |
4 (10.0) |
1.000 |

Go to :

DISCUSSION
Urological complications represent a significant cause in morbidity associated with renal transplantation. Despite preserving the vascularity of the ureter during donor nephrectomy and adhering to a meticulous anastomotic technique, complications can occur. Urological complications are the most common surgical complications after renal transplantation and they usually present early (within three months) after transplant [
1]. Double-J stent, although used extensively in routine vesico-ureteric reconstruction, has a controversial role in renal transplantation surgery, owing to higher chance of developing UTI, probably because of immune- compromised status of these patients. Surgeons are divided in to two groups, one who prefer to stent routinely to prevent urological complications despite more UTI and others who prefer to stent selectively for specific indications [
89]. The benefits of routine stenting are not universally accepted and evidence from previous randomized trials is inconsistent (
Table 4) [
16710111215]. The results of our study show that there was no significant difference between both groups with respect to early urological complications and lymphocele. In this study, the 5% incidence of urinary leak and 2.5% incidence of urinary obstruction in non-stented group are comparable to those reported by others. The 8.8% patients of stented group developed lymphocele whereas 10.0% patients from non-stented group had lymphocele (p=1.000). However, there was no increased incidence of UTI (32.4% in stented vs. 30.0% in non-stented, p=1.000) (
Table 3).
Table 4
Randomized studies comparing effect of ureteral stent in renal transplantation

|
Study |
No. of patients |
Stent duration |
Significant effect of stenting on |
|
Urological complications |
Incidence of urinary tract infections |
|
Pleass et al. [10] (1995) |
300 |
3 mo |
Yes |
No |
|
Bassiri et al. [11] (1995) |
77 |
54 d |
No |
Yes |
|
Benoit et al. [7] (1996) |
194 |
1 mo |
Yes |
No |
|
Kumar et al. [1] (2000) |
100 |
1 mo |
Yes |
No |
|
Dominguez et al. [6] (2000) |
280 |
7–10 d |
No |
No |
|
Osman et al. [12] (2005) |
100 |
14 d |
No |
Yes |
|
Tavakoli et al. [15] (2007) |
190 |
74.3 d |
Yes |
Yes |

Bassiri et al. [
11] in their randomized prospective study of 77 renal transplant recipients evaluated the effect of stenting on urological complications. In their study the average time to stent removal was 54 days. One of the 37 non-stented patients (2.7%) had urinary leakage vs. none of the 35 stented patients (p=NS). There was no statistically significant difference with respect to occurrence of urinary obstruction (2.7% vs. 0%). They found that 33% of stented patients developed UTI compared to 5% of non-stented patients (p<0.05). Possibly the increased incidence of UTI could be due to longer duration of stent
in situ.
In a prospective randomized control trial of 190 renal transplant recipients, published by Tavakoli et al. [
15] in 2007, mean time to stent removal was 74.3 days and there were no cases of stent related problems. They found a significant decrease in occurrence of urinary leakage (8.9% in non-stented group vs. 0.9% in stented group, p<0.008) and urinary obstruction (7.7% vs. 0%, p<0.004). Tavakoli et al. [
15] had total of 42 episodes of UTI in 35 patients in the stent group compared to 20 episodes in 13 patients in the nonstented group (p<0.02 for number of patients). Again this could be because of the longer duration of stent in their study.
The 3-phase longitudinal study by Kumar et al. [
1] demonstrated convincing results in favour of stenting. In this series of living related transplants there was a complication rate of 8% during phase 1, when no stents were used. This decreased to 3% in phase 2, when 100 patients were randomized to stenting or no stenting and to 0.04% in phase 3, when 400 transplanted patients were routinely stented. They had removed the stent at 1 month duration, similar to our study. Their study also did not show any significant difference in the incidence of UTI between the stented and non-stented groups.
Thus though stents can cause an increased incidence of UTI if kept for a longer duration, we speculate that removing them earlier (at about 4 weeks interval), might help eliminate the negative effect of stenting on UTI.
In a recent review Wilson et al. [
16] concluded that the routine prophylactic stenting decreases the incidence of major urological complications.
In our study, the mean eGFR was significantly better in stented group up to 2 months postoperatively (p<0.05). It can be seen from
Table 1 that the donor GFR was also better in the stented group. This may account partly for the better postoperative GFR in the stented group. However, the mean postoperative difference in the GFR is better than the mean preoperative difference. And as can be seen from
Fig. 1, the graft function improves with passage of time in the stented group, thereby suggesting the possible role of the stent.
Benoit et al. [
7] in their randomized prospective study found that renal function at 1 week post-transplant was better in stented group compared to non-stented group; although at 1 year the graft functions of both groups were comparable. Kumar et al. [
17] hypothesized that, in the early postoperative period oedema or blood clots can produce ureteral obstruction and high intraluminal pressure. With a stent in place these transient episodes of obstruction can be avoided; leading to better drainage and better graft function, as well as lesser complications like urinary fistulae.
Our study did have some limitations. First it is a single centre study. Secondly we have not done multivariate analysis because of the low number of events in each group. Lastly, it was a non randomized study because the prospective stented patients were compared with historical controls.
Go to :

CONCLUSIONS
Placement of ureteral stent in renal transplant does not significantly affect the occurrence of urinary leak, urinary obstruction and lymphocele. Stent related bothersome symptoms are not significant in case stent is placed in renal transplantation. There is no significant increase in the incidence of UTI. Graft function is significantly better in stented renal transplant recipients up to 2 months postoperatively although we cannot comment upon long term graft function due short follow-up period. Longer term multicentric studies, with multivariate analysis are required to find out whether stents can improve the graft function on a more durable basis.
Go to :









 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download