1. Shigehara K, Namiki M. Late-onset hypogonadism syndrome and lower urinary tract symptoms. Korean J Urol. 2011; 52:657–663. PMID:
22087358.

2. Patel ND, Parsons JK. Epidemiology and etiology of benign prostatic hyperplasia and bladder outlet obstruction. Indian J Urol. 2014; 30:170–176. PMID:
24744516.

3. Parsons JK. Benign prostatic hyperplasia and male lower urinary tract symptoms: epidemiology and risk factors. Curr Bladder Dysfunct Rep. 2010; 5:212–218. PMID:
21475707.

4. Kalinchenko S, Vishnevskiy EL, Koval AN, Mskhalaya GJ, Saad F. Beneficial effects of testosterone administration on symptoms of the lower urinary tract in men with late-onset hypogonadism: a pilot study. Aging Male. 2008; 11:57–61. PMID:
18570056.

5. Vignozzi L, Morelli A, Corona G, Sebastianelli A, Serni S, Gacci M, et al. Testosterone protects the lower urinary tract from metabolic syndrome-induced alterations. Horm Mol Biol Clin Investig. 2012; 11:329–337.

6. De Nunzio C, Kramer G, Marberger M, Montironi R, Nelson W, Schröder F, et al. The controversial relationship between benign prostatic hyperplasia and prostate cancer: the role of inflammation. Eur Urol. 2011; 60:106–117. PMID:
21497433.

7. Vignozzi L, Gacci M, Maggi M. Lower urinary tract symptoms, benign prostatic hyperplasia and metabolic syndrome. Nat Rev Urol. 2016; 13:108–119. PMID:
26754190.

8. De Nunzio C, Aronson W, Freedland SJ, Giovannucci E, Parsons JK. The correlation between metabolic syndrome and prostatic diseases. Eur Urol. 2012; 61:560–570. PMID:
22119157.

9. De Nunzio C, Cindolo L, Gacci M, Pellegrini F, Carini M, Lombardo R, et al. Metabolic syndrome and lower urinary tract symptoms in patients with benign prostatic enlargement: a possible link to storage symptoms. Urology. 2014; 84:1181–1187. PMID:
25443931.

10. Cohen PG. Abdominal obesity and intra-abdominal pressure: a new paradigm for the pathogenesis of the hypogonadal-obesity-BPH-LUTS connection. Horm Mol Biol Clin Investig. 2012; 11:317–320.

11. Baas W, Köhler TS. Testosterone replacement therapy and voiding dysfunction. Transl Androl Urol. 2016; 5:890–897. PMID:
28078221.

12. Haider KS, Haider A, Doros G, Traish A. Long-term testosterone therapy improves urinary and sexual function, and quality of life in men with hypogonadism: results from a propensity matched subgroup of a controlled registry study. J Urol. 2018; 199:257–265. PMID:
28728990.

13. Wallis CJ, Lo K, Lee Y, Krakowsky Y, Garbens A, Satkunasivam R, et al. Survival and cardiovascular events in men treated with testosterone replacement therapy: an intention-to-treat observational cohort study. Lancet Diabetes Endocrinol. 2016; 4:498–506. PMID:
27165609.

14. Haider A, Zitzmann M, Doros G, Isbarn H, Hammerer P, Yassin A. Incidence of prostate cancer in hypogonadal men receiving testosterone therapy: observations from 5-year median followup of 3 registries. J Urol. 2015; 193:80–86. PMID:
24980615.

15. Shigehara K, Sugimoto K, Konaka H, Iijima M, Fukushima M, Maeda Y, et al. Androgen replacement therapy contributes to improving lower urinary tract symptoms in patients with hypogonadism and benign prostate hypertrophy: a randomised controlled study. Aging Male. 2011; 14:53–58. PMID:
21171937.

16. Ko YH, Moon du G, Moon KH. Testosterone replacement alone for testosterone deficiency syndrome improves moderate lower urinary tract symptoms: one year follow-up. World J Mens Health. 2013; 31:47–52. PMID:
23658865.

17. Yucel C, Keskin MZ, Peskircioglu CL. The effect of transdermal testosterone administration on lower urinary tract symptoms and erectile dysfunction: a prospective, randomized, placebo-controlled trial. Curr Urol. 2017; 11:4–8. PMID:
29463970.

18. Francomano D, Ilacqua A, Bruzziches R, Lenzi A, Aversa A. Effects of 5-year treatment with testosterone undecanoate on lower urinary tract symptoms in obese men with hypogonadism and metabolic syndrome. Urology. 2014; 83:167–173. PMID:
24139347.

19. Debruyne FM, Behre HM, Roehrborn CG, Maggi M, Wu FC, Schröder FH, et al. Testosterone treatment is not associated with increased risk of prostate cancer or worsening of lower urinary tract symptoms: prostate health outcomes in the Registry of Hypogonadism in Men. BJU Int. 2017; 119:216–224. PMID:
27409523.

20. Kohn TP, Mata DA, Ramasamy R, Lipshultz LI. Effects of testosterone replacement therapy on lower urinary tract symptoms: a systematic review and meta-analysis. Eur Urol. 2016; 69:1083–1090. PMID:
26874809.

21. Kathrins M, Doersch K, Nimeh T, Canto A, Niederberger C, Seftel A. The relationship between testosterone-replacement therapy and lower urinary tract symptoms: a systematic review. Urology. 2016; 88:22–32. PMID:
26616095.

22. Kupelian V, Chiu GR, Araujo AB, Williams RE, Clark RV, McKinlay JB. Association of sex hormones and C-reactive protein levels in men. Clin Endocrinol (Oxf). 2010; 72:527–533. PMID:
19769617.

23. Lin PH, Freedland SJ. Lifestyle and lower urinary tract symptoms: what is the correlation in men? Curr Opin Urol. 2015; 25:1–5. PMID:
25393271.
24. Yelsel K, Alma E, Eken A, Gülüm M, Erçil H, Ayyıldız A. Effect of obesity on International Prostate Symptom Score and prostate volume. Urol Ann. 2015; 7:371–374. PMID:
26229329.

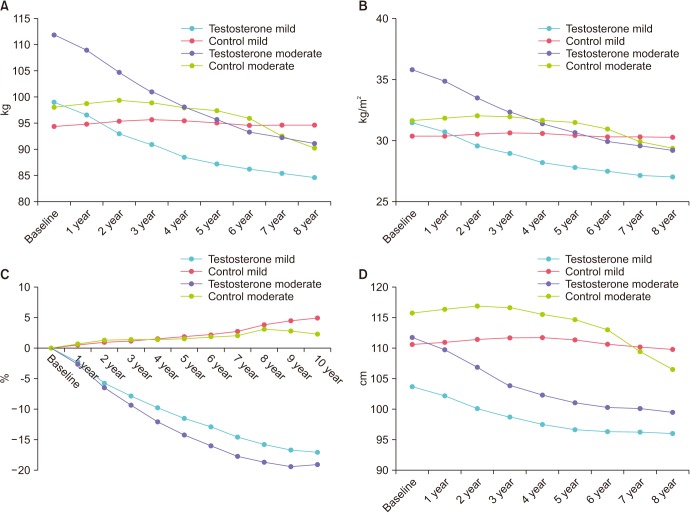
25. Saad F, Yassin A, Doros G, Haider A. Effects of long-term treatment with testosterone on weight and waist size in 411 hypogonadal men with obesity classes I-III: observational data from two registry studies. Int J Obes (Lond). 2016; 40:162–170. PMID:
26219417.

26. Gacci M, Corona G, Sebastianelli A, Serni S, De Nunzio C, Maggi M, et al. Male lower urinary tract symptoms and cardiovascular events: a systematic review and meta-analysis. Eur Urol. 2016; 70:788–796. PMID:
27451136.

27. Russo GI, Castelli T, Privitera S, Fragalà E, Favilla V, Reale G, et al. Increase of Framingham cardiovascular disease risk score is associated with severity of lower urinary tract symptoms. BJU Int. 2015; 116:791–796. PMID:
25601421.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download