TURP is the most commonly performed and gold standard procedure in the surgical management of BPH [
13]. Factors associated with increased complication rates of TURP include learning period, older patients, patients with cardiopulmonary comorbidities, and hemostatic disorders. Bleeding requiring blood transfusion, urethral stenosis, TUR syndrome, and prolonged catheterization times are still the most significant complications [
414]. Despite its clinical outcome, this increased complication rate has led to the need for development of alternative techniques of prostate ablation with similar clinical results but with lesser complications. Amongst these, laser ablation and vaporization procedures, such as KTP, diode, and HOLEP are promising surgical techniques [
91516]. It can be a challenge to select the appropriate laser to be used in the treatment of BPH. The parameters that must be considered include its effectiveness, mechanism, durability, rate of complications, catheterization time, hospital stay, and cost effectiveness. Therefore, it is necessary to know how laser works and its properties. Laser (light amplification by stimulated emission of radiation) can be produced by different medium with specific wavelength and direction [
11]. The medium and the excitation source establish the wavelength and the mode of emission (continuous or pulse) of each laser type [
17]. The prostatic tissue absorbs energy by its chromophores which are water and Hb. Absorption coefficients of these chromophores change with different wavelengths, resulting in differences in absorption of energy amongst laser types. Intracellular temperature is raised when energy is absorbed by prostatic tissue, leading to coagulation and subsequently vaporization of tissue [
1718]. In the treatment of BPH, the medium used in the treatment of BPH is either a crystal or semiconductor. Crystals used are Ho: YAG, thulium: YAG (Tm: YAG), KTP and lithium triborate, and semiconductors used are diode lasers. Multiple laser types, with different wavelengths and hence differing properties have been developed and substantial testing of their clinical safety, efficacy, and durability has been done [
9]. Among these, HOLEP has functional outcomes similar to those of TURP and open prostatectomy, but its biggest limitation is longer operation time and a steep learning curve [
919]. On the other hand, the safety of PVP with KTP laser (532 nm wavelength) and its effectiveness is well established and has the advantage of treating patients on anticoagulant and antiplatelet agents [
20]. Due to a high affinity for Hb, it has good hemostasis property with low morbidity, good medium term results, and small learning curve but prolong operative time [
1621]. On the contrary, newly developed diode lasers are less known to the world. They are semiconductors that generate and emit monochromatic light, which on passing through a crystal leads to the final wavelength [
11]. Multiple diode lasers of different wavelengths (940, 980, or 1,470 nm) are available. Unlike KTP laser, 980 nm wavelength diode laser has the highest simultaneous absorption of water and Hb, leading to better and quick tissue ablation with excellent hemostasis [
12]. These lasers have a major disadvantage of near-infrared wavelength which causes coagulation necrosis due to deep optical penetration. Dysuria, sloughing, and long-lasting storage symptoms occur due to the necrotic tissue [
22]. To overcome this, new diode laser systems are designed to reduce depth of penetration by modulation of their frequency, pulsation, power, and fiber design. A quartz head contact laser fiber was introduced to reduce penetration depth, leading to a decrease in incidence of dysuria from 42% to 17%, and in the passage of slough from 52% to 16% [
23]. The diode laser can be applied continuously or in pulsed mode. We used the continuous-wave mode with newly designed twister fiber. Fiber modifications led to a significant reduction in surgical time [
23]. Wendt-Nordahl et al. [
12] extensively studied diode laser. Various characteristics of KTP lasers (532 nm and 80 W) were compared with diode laser (980 nm and 120 W) in a well-established, isolated, perfused porcine kidney model. The diode laser has a thinner coagulation zone (290.1 µm vs. 666.9 µm; p<0.05) and tissue ablative properties were 7.24 g/10 min, nearly double that of KTP laser (3.99 g/10 min). This is lesser than in TURP, which has a resection capacity of 8.28 g/30 s. They reported parallel bleeding rates (0.21 vs. 0.14 g of Hb/min). The diode laser has coagulation rim of 0.5 mm (range, 0.2–1 mm) in prostate tissue and does not have any areas of hemorrhage [
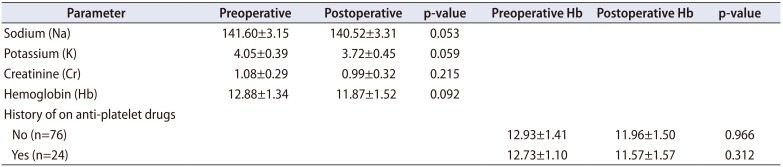
24]. As energy is mainly absorbed at the surface of prostatic tissue, it provides larger ablative and better hemostatic properties, even in patients who are on oral anticoagulation. Therefore, there is no need to discontinue anticoagulant therapy before procedure [
12]. In the diode laser at 980 nm, the speed of vaporization does not depend on the tissue being mucosa or fibromuscular stroma, which is not the case with other lasers [
2425]. Furthermore, diode laser also has the advantage of lower energy consumption and does not require high voltage connection, improving mobility of the laser generator, as compared to KPT and Ho: YAG laser devices [
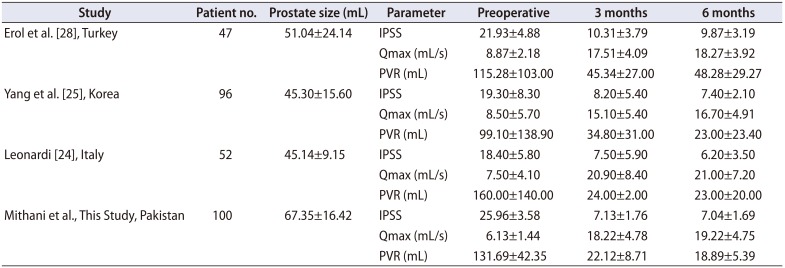
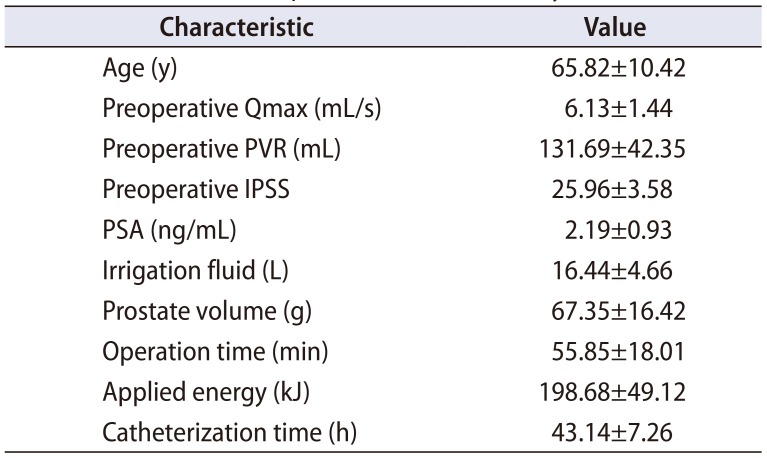
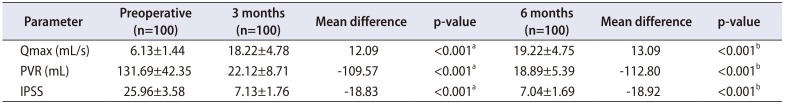
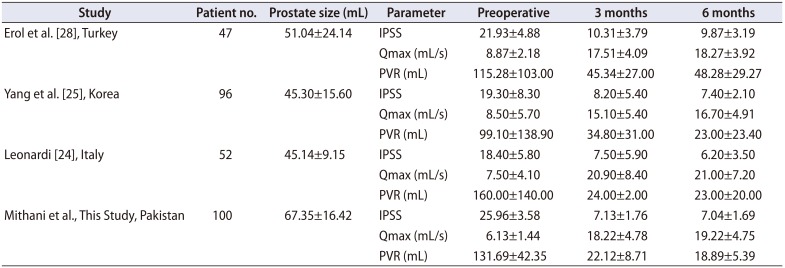
2627]. Although above evidence is highly suggestive that 980 nm diode laser is a novel technology for laser prostectomy, but in terms of surgical outcome, evidence is still sparse. Hundred patients were included in this study who underwent diode laser PVP and significant improvements in mean IPSS, Qmax & PVR were observed, and results are comparable to the similar case series (
Table 5) [
242528]. In recent years a few clinical trials with different techniques of diode laser enucleation have been reported [
2930], comparing diode laser enucleation of the prostate with bipolar TURP and reported equal improvement in functional outcomes with shorter hospital stay and catheterization time in patients who were treated with diode laser enucleation. However, there are only two randomized clinical trial reports on efficacy and safety of diode LVP in comparison with TURP. Both studies revealed that PVP with a diode laser is effective and a safe alternate to TURP for the treatment of BPH. PVP has the advantage of shorter catheterization time and hospitalization, and no need for discontinuation of anticoagulant therapy [
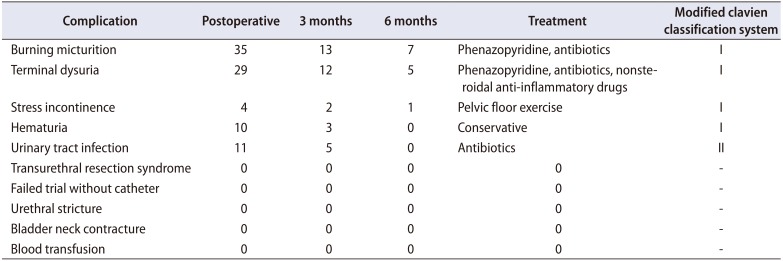
2627]. The literature has reported high rates of dysuria and burning micturition [
152627]. In this study, dysuria and burning micturition were 29% and 35% respectively. Furthermore, few studies have also reported high re-operation rates (8%–33%) and persisting stress urinary incontinence (9.1%) [
1526]. We did not encounter this in this study. As with any other laser vaporization technique, diode laser also has same limitation of lack of tissue retrieval for histopathology [
9]. Therefore patients must be evaluated for prostate cancer prior to diode laser vaporization through prostate specific antigen, digital rectal examination, and prostate biopsy wherever indicated. We excluded all patients who had clinical suspicion of prostate cancer. Another drawback of diode laser is the cost. Although it costs less compared to other lasers treatment for BPH but is still more expensive than TURP. In The Kidney Centre Post Graduate Training Institute, diode laser is 30% more expensive than TURP. There are a few limitations in our study. Preoperative and postoperative sexual dysfunction was not included in the study protocol. Other limitations were lack of long-term follow-up and unavailability of late complication data. Due to inappropriate selection of patients in initial days of our learning curve, 9 patients were converted to TURP due to very large prostate size (
Table 4).
Table 5
Study outcomes comparison with other studies
|
Study |
Patient no. |
Prostate size (mL) |
Parameter |
Preoperative |
3 months |
6 months |
|
Erol et al. [28], Turkey |
47 |
51.04±24.14 |
IPSS |
21.93±4.88 |
10.31±3.79 |
9.87±3.19 |
|
Qmax (mL/s) |
8.87±2.18 |
17.51±4.09 |
18.27±3.92 |
|
PVR (mL) |
115.28±103.00 |
45.34±27.00 |
48.28±29.27 |
|
Yang et al. [25], Korea |
96 |
45.30±15.60 |
IPSS |
19.30±8.30 |
8.20±5.40 |
7.40±2.10 |
|
Qmax (mL/s) |
8.50±5.70 |
15.10±5.40 |
16.70±4.91 |
|
PVR (mL) |
99.10±138.90 |
34.80±31.00 |
23.00±23.40 |
|
Leonardi [24], Italy |
52 |
45.14±9.15 |
IPSS |
18.40±5.80 |
7.50±5.90 |
6.20±3.50 |
|
Qmax (mL/s) |
7.50±4.10 |
20.90±8.40 |
21.00±7.20 |
|
PVR (mL) |
160.00±140.00 |
24.00±2.00 |
23.00±20.00 |
|
Mithani et al., This Study, Pakistan |
100 |
67.35±16.42 |
IPSS |
25.96±3.58 |
7.13±1.76 |
7.04±1.69 |
|
Qmax (mL/s) |
6.13±1.44 |
18.22±4.78 |
19.22±4.75 |
|
PVR (mL) |
131.69±42.35 |
22.12±8.71 |
18.89±5.39 |





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download