Abstract
Elbow arthrodesis is a predictable salvage surgery for advanced elbow joint disease. However, iatrogenic joint fusion impaired activity of daily living. In the presented case, a young woman suffered from an iatrogenic joint fusion which developed after several surgeries for comminuted intercondylar fracture of distal humerus. We tried to reconstruct the ulnohumeral joint, as she was too young to have a total elbow arthroplasty. Finally, she regained the motion of elbow and satisfied with the clinical outcome after two consecutive operations. We described the process of recovery and summarized the pearls and pitfalls.
Elbow arthrodesis is a predictable salvage surgery for advanced elbow joint disease, such as unilateral post-traumatic arthritis or deep infection1. However, the result of elbow arthrodesis is not always satisfactory. Complete loss of motion at the elbow should be compensated by the wrist and shoulder joints to perform the daily activities and sometimes residual pain is also a trouble to the patient and surgeon even after arthrodesis2. Furthermore, iatrogenic joint fusion of the dominant elbow in a young woman impaired activity of daily living and human dignity along with patient's dissatisfaction.
We attempted reconstruction of the dominant elbow joint that showed iatrogenic joint fusion which developed after several surgeries in a young woman with comminuted intercondylar fracture, and report the result with review of the literature. She gave an informed consent.
A 29-year-old female presented with a complaint of loss of motion in the right elbow resulting from surgeries performed three times at another hospital. She was a right-hand dominant dental hygienist and had a history of open, displaced, and comminuted intercondylar fracture of the distal humerus after a fall. The patient had no motion at the right elbow, which was fused at 70 degrees but achieved 45 degrees of pronation and 45 degrees of supination. She did not feel pain and her motor and sensory examination of the hand was normal. Laboratory data revealed no leukocytosis and normal value of C-reactive protein. Radiographs and 3-dimensional computed tomography (CT) scan of the elbow revealed a fusion of the ulnohumeral joint with a retained wire (Fig. 1). Disabilities of the arm, shoulder, and hand (DASH) score was 93.1 and Mayo elbow performance index was 60.
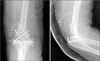
We could identify C2 fracture of the distal humerus according to the AO classification with review of the initial radiograph and CT scan. Crossed pinning with 3 K-wires was performed without accurate reduction of the articular surface and rigid fixation of both columns at index operation (Fig. 2). Loss of reduction was found at 1 week after the index operation and multiple pinning for fixation of articular fragments was performed in addition to repetitive crossed pinning through the trans-olecranon approach at the second operation (Fig. 3). Third operation was performed by using 3 percutaneous Steinmann pins to treat delayed union at 5 months after the previous operation (Fig. 4). Finally, she visited Hanyang University Hospital with a fused elbow at 1 year 4 months after the index operation.
She desired to achieve motion of the elbow and she had the strong will to overcome difficult rehabilitation. We decided to perform not total elbow replacement, but reconstruction of the ulnohumeral joint with elbow contracture release considering her young age. The patient was placed in a lateral position and a posterior incision was made following resection of the previous operation scar. Ulnar nerve had transposed anteriorly preserving the vascularity. There was a severe adhesion and contracture of both compartments of arm muscles. Circumferential adhesiolysis at both lateral and medial column and capsulectomy were performed thoroughly. The flexor-pronator was lifted off the medial supracondylar ridge with the posterior portion of the flexor carpi ulnaris tendon left attached to the epicondyle. Dissection of the anterior capsule to separate it from the brachialis muscle was done laterally. The posterior capsule of the joint was exposed after elevating of the triceps from the posterior distal surface of the humerus. The plane of the anterior dissection on the lateral approach was anterior to the anconeus and the posterior dissection was between the anconeus and the exntensor carpi ulnaris. We tried to preserve the common flexor and extensor group rather than the collateral ligament, because instability is of less concern in debridement arthroplasty for a stiff elbow. Although, the articular cartilage of radiocapitellar joint was intact, the ulnohumeral joint was destroyed. The ulnohumeral joint was reconstructed from a totally fused elbow with an osteotome and a burr. Osteotomy was performed while tracing evidence of the joint, such as fragments of the cartilage under fluoroscopic guidance and the cut surface of both the humerus and ulna was trimmed with burring to achieve congruity of the joint. In the operating room, passive flexion was possible to 20 degrees and passive extension was possible to 120 degrees after reconstruction of the ulnohumeral joint.
The elbow was fully immobilized with long arm splint for postoperative 3 days. And then customized hinged elbow brace was applied and the position of her elbow was switched to full flexion during the morning and to full extension during the afternoon for the first 2 weeks. The switch of the elbow position was increased two times a day during the following 2 weeks. Radiographs revealed indistinct and narrow ulnohumeral joint at 4 months after the first operation at Hanyang University Hospital (Fig. 5). However, the range of motion was decreased to 80 degrees of extension and 95 degrees of flexion even without any complication, such as infection. She could not endure the rehabilitation program due to severe pain and the motion of the elbow was decreased gradually. Although she could hardly bend and extend her elbow compared to that before the surgery, she longed to undergo an operation again.
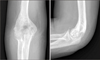
To avoid the same poor outcome, we required the strict prerequisite of muscle power of the arm. She achieved normal grade of muscle power after the 2-month isometric exercise program. We performed elbow contracture release again 5 months after the first release surgery at our hospital and achieved 20 degrees of passive extension and 120 degrees of passive flexion during the operation. In second surgery, reconstructed surface of ulnohumeral joint was intact and there was no additional take-down procedure for ankylosis. Protocol for postoperative rehabilitation was same as that for previous rehabilitation. Finally, she showed 30 degrees of flexion contracture, 135 degrees of active further flexion, 45 degrees of supination, and 80 degrees of pronation at 20 months after the last surgery (Fig. 6). DASH score was 38.3 and Mayo elbow performance index was 85 at last follow-up. She was completely satisfied with the motion of the elbow although there was mild pain (a visual analogue scale score of 2) during motion.
Advances in joint replacement, such as anatomic designs and improved polyethylene, have led to an interest in the conversion of a surgically or spontaneously fused joint. Takedown of hip and knee fusions with conversion to arthroplasty has already been well described and conversion to arthroplasty has also been reported in the shoulder and ankle34. Recently, there have been some published reports of takedown of an elbow arthrodesis to arthroplasty5.
We agree with the view that total elbow arthroplasty is a viable treatment for a fused elbow. However, the longevity of total elbow arthroplasty is not proved thoroughly yet and revision arthroplasty is still a challenging procedure6. We could not decide on the conversion to arthroplasty for her fused elbow because the patient was in her twenties and she needed to undergo at least more than two revision surgeries during her life. Although hemiarthroplasty provided reliable results in the complex intraarticular fracture in distal humerus, we hesitated to do a hemiarthroplasty in presented case due to same concerns of longevity7. Distraction interposition arthroplasty also was considered. However, there are few studies that addressed the result of distraction interposition arthroplasty in the fused elbow and this procedure might provoke instability of elbow due to extensive dissection89. And the dynamic joint distractor is essentially needed as a distractor and a fixator to permit postoperative rehabilitation under control of the varus/valgus stability. The dynamic joint distractor was not available in our country at that time.
Operative release is a challenging procedure for treatment of osseous ankyloses10. Hence, there were some important prerequisites for the satisfactory outcome in the presented case. First, the patient should recover the normal grade of muscle power preoperatively using isometric exercise. Adequate muscle power was essential to achieve substantial recovery of range of motion overcoming the pain and the stiffness during prompt active motion after the operation. Second, bone stock should be adequate for reconstruction of the joint and strong enough to withstand strenuous passive and active motion, such as flexion and extension. Some loss of bone was inevitable due to repetitive osteotomy and burring. Third, complete adhesiolysis and release of contracted muscle and capsule was also required intraoperatively, because the soft tissue tension was resistant to recovery of the range of motion. Finally, reconstruction to an almost normal shape of the ulnohumeral joint was needed to maintain smooth motion of the elbow.
Operative reconstruction of an ulnohumeral joint is absolutely challenging not only for the surgeon and but also for the patient. The patient in the presented case did not get frustrated by the poor outcome of the first operation at Hanyang University Hospital and accepted the challenge again to achieve additional motion of the elbow. She recovered the muscle power of her arm through a strenuous exercise program before the operation and achieved 30 degrees of flexion contracture and 135 degrees of further flexion at the last follow-up. This exceeded our expectation of 120 degrees of flexion observed in the operating room. It is undoubted that her effort for rehabilitation was responsible for satisfactory results.
The case presented in this report is the first documented reconstruction of the ulnohumeral joint and the operation and rehabilitation resulted in an excellent outcome in a young patient with a fused elbow. This operation has some inherent limitations, such as newly developed pain and only a temporary procedure before arthroplasty. However, it is certain that this operation will delay the need for total elbow arthroplasty and reduce the number of additional revision surgeries in her life.
Figures and Tables
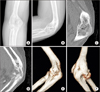 | Fig. 1(A, B) Plain radiographs showed the fused elbow with a retained wire. (C–F) Sagittal and 3-dimensional images of the computed tomography scan showed the bony fusion of ulnohumeral joint. |
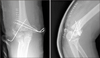 | Fig. 2Inaccurate reduction of articular fragments and inappropriate fixation with 3 K-wires were found after initial operation. |
 | Fig. 4Three Steinmann pins were placed to treat the delayed union and false motion at fracture site. |
References
1. Otto RJ, Mulieri PJ, Cottrell BJ, Mighell MA. Arthrodesis for failed total elbow arthroplasty with deep infection. J Shoulder Elbow Surg. 2014; 23:302–307.

2. Koller H, Kolb K, Assuncao A, Kolb W, Holz U. The fate of elbow arthrodesis: indications, techniques, and outcome in fourteen patients. J Shoulder Elbow Surg. 2008; 17:293–306.

3. Hintermann B, Barg A, Knupp M, Valderrabano V. Conversion of painful ankle arthrodesis to total ankle arthroplasty. J Bone Joint Surg Am. 2009; 91:850–858.

4. Sperling JW, Cofield RH. Total shoulder arthroplasty after attempted shoulder arthrodesis: report of three cases. J Shoulder Elbow Surg. 2003; 12:302–305.

5. Burkhart KJ, Dargel J, Wegmann K, Müller LP. Conversion of elbow arthrodesis to total elbow arthroplasty. Unfallchirurg. 2013; 116:371–375.
6. Mansat P, Bonnevialle N, Rongières M, Mansat M, Bonnevialle P. French Society for Shoulder and Elbow SOFEC. Results with a minimum of 10 years follow-up of the Coonrad/Morrey total elbow arthroplasty. Orthop Traumatol Surg Res. 2013; 99:S337–S343.

7. Park SE, Kim JY, Cho SW, Rhee SK, Kwon SY. Complications and revision rate compared by type of total elbow arthroplasty. J Shoulder Elbow Surg. 2013; 22:1121–1127.

8. Hohman DW, Nodzo SR, Qvick LM, Duquin TR, Paterson PP. Hemiarthroplasty of the distal humerus for acute and chronic complex intra-articular injuries. J Shoulder Elbow Surg. 2014; 23:265–272.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download