Abstract
Malignant melanomas sometimes present with nail or periungual pigmentation, as a subungual melanoma. This pigmentation also occurs in nonmelanoma skin disorders. Therefore, biopsy is mandatory for the absolute diagnosis. We present an atypical presentation of subungual melanoma in an 81-year-old female patient with no specific periungual pigmentation. She suffered from a crushing injury in her right thumb 2 years ago and had undergone repetitive stump plasty at a local clinic. Recently, she felt intermittent pain at the thumb tip. During the revisional stump plasty, we unexpectedly noted a spread out of dark colored soft tissues the distal phalanx. Pathological examination revealed subungual malignant melanoma. This unusual form of melanoma has a predilection for an acral location, particularly the paronychial region. Even when small pigments are found on the periungual area, careful examination and identification of a component of melanoma is necessary in order to not miss any malignant finger lesion.
Subungual melanoma is an uncommon variant of melanoma that arises in the nail unit often causing difficulties in diagnosis for the clinician1. It has worse results compared to cutaneous melanoma in other sites due to its delayed diagnosis2. There are still controversies about which clinical features may affect prognosis2. These tumors usually present with typical local symptoms such as colorful nail streak or plate changes, ulceration, bleeding, and pain3. However, these lesions sometimes have been mistaken for hematomas, warts, paronychia, blisters, or nevi45. Misdiagnosis or delayed diagnosis have resulted in advanced stage lesions at first presentation. Therefore, early recognition of clinical signs and symptoms with punch biopsy of the nail bed is mandatory in the suspected lesions4.
Although it is usually regarded as a form of cutaneous melanoma, the causative factors of subungual melanoma remain unclear. There is no demonstrable association between the development of subungual melanoma and excessive exposure to ultraviolet light, and the nail plate has been shown to act as a protective barrier4. Antecedent trauma is reported in many patients, but its role in the pathogenesis of the disease process is not conclusively established6. Therefore, it is often held that trauma to the fingertip is likely to be coincidental in patient with subungual melanoma.
We report a rare case of primary subungual melanoma without any specific cutaneous pigmentation at the fingertip. It was missed by unwary clinicians and lead to misdiagnosis preoperatively.
An 81-year-old woman visited our outpatient clinic with fingertip pain and very small remnant nail tissue on the right thumb. She has suffered from a crushing injury in her right thumb 2 years ago. She had been underwent stump plasty with excision and nail extraction repetitively at a local clinic. The symptoms began 2 months ago before especially when she overused her hands. By physical examination, there were painful nail remnants on perionychium of the nail root on her right thumb (Fig. 1). During the exploration, to remove the nail remnants, we encountered the dark, black color tinged soft tissues and bone which were spread out like dye-tinged tissues (Fig. 2). All the dirty tissues were removed and sent for the pathological examination, and pathology revealed an atypical melanocytic proliferation, which implied melanotic malignant melanoma without regional lymphatic invasion. Additional skin lesions could not be observed at other sites. According to tumor, node, and metastasis (TNM) staging, this malignant melanoma was T4 N0 M0, stage IIC. Reoperation was performed immediately at the metacarpophalangeal (MCP) joint level for digital amputation (Fig. 3). Because she refused, we did not perform additional procedure. There are a frozen biopsy was implemented and neither local invasion nor metastasis was proved in pathological examination. This subsequent amputation showed no residual melanoma. Recurrence was not observed after the following 5 years.
Subungual melanoma has been considered as a deadly form of melanoma due to its high mortality with only 27% of 5-year survival rate7. While cutaneous melanoma has been found to be more common in Caucasians, melanoma in unusual sites such as hands and feet is thought to occur disproportionately more often in dark skinned race8. Subungual melanoma has the peak incidence in the 5th to 7th decades and known to be occurred most frequently in the thumb (34%) and the 3rd finger (14%)68.
Despite the apparent increase in attention to subungual melanoma, little progress has been made in the characterization of the diagnosis and prognosis. Hutchinson firstly published his experience with subungual melanoma in 1886 and reported that the lesion was usually attributed to a traumatic injury5. Some suggested an association with a history of nail trauma in addition to sun exposure4. Although, there has never been conclusive evidence that trauma is a causative factor, 29%–55% of patients report the relationship between direct trauma and the onset of subungual melanoma in recent studies6.
Subungual melanoma might appear initially as melanonychia striata longitudinalis in the nail plate. It is often neglected by patients and frequently misdiagnosed by physicians. Hutchinson's sign, which is periungual pigmentation accompanied by melanonychia, is the most significant sign in the differentiation between subungual melanoma and melanocytic nevus5. The estimated mean delay in diagnosis ranges from 3 to 24 months which is nearly double time of the diagnostic delay observed with cutaneous melanoma79. Therefore, it results more advanced stages of disease at presentation, and it frequently requires radical excision, such as amputation of the affected fingers. Optimal diagnosis could be made by punch biopsy of the nail bed, but has its limitations because accurate measurement of depth of invasion is often challenging2. Five percent of all cutaneous melanoma has known to occur on the hands and feet, where it is much more difficult to achieve adequate diagnosis and management1. Therefore, Melanoma within the digit necessitates a careful approach and precise diagnosis1.
American Academy of Dermatology recommends the safety margin of cutaneous melanoma as 0.5–1.0 cm for in situ tumors, 1.0 cm for tumors <1.0 mm, 1.0–2.0 cm for tumors 1.01–2.0 mm, and 2.0 cm for tumors >2.0 mm24. When melanoma presents on the digits or in the subungual area, amputation should be usually preformed as in our case3. However, this tendency has been recently broken with proven equivalent oncologic outcomes with more distal amputation for most lesions or even wide local excision for in situ lesions10.
The differential diagnosis includes single pigmented nail streak, soft tissue necrosis exhibiting ulceration or black color changing, other infection or cellulitis. Many of subungual melanomas have been initially mistaken for benign or traumatic lesions of the nail bed such as pyogenic granuloma, paronychia, hematoma, blister, and pigmented nevus2.
Our report focuses on one case of an extremely rare presentation of malignant melanoma with residual nail fragment. Although there was no pigmentation externally, only the following two notes; the periungual nail remnants, and dark colored tinged at the exploration revealed melanotic subungual melanoma in our case. It would appear that this unusual form of melanoma has a predilection for acral location, particularly the periungual region. Therefore, any colored pigments, chronic pain or recurred inflammation should be given special attention in the differential diagnosis malignant melanoma of the toes and fingers.
Figures and Tables
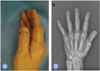 | Fig. 1(A) Bilateral fingertip nail remnants on the eponychium. (B) X-ray images of the first visit. She had been underwent stump plasty with nail extraction. |
References
1. Imakado S, Sato H, Hamada K. Two cases of subungual melanoma in situ. J Dermatol. 2008; 35:754–758.
2. Linares MD, Hardisson D, Perna C. Subungual malignant melanoma of the hand: unusual clinical presentation: case report. Scand J Plast Reconstr Surg Hand Surg. 1998; 32:347–350.
3. Yang Z, Xie L, Huang Y, et al. Clinical features of malignant melanoma of the finger and therapeutic efficacies of different treatments. Oncol Lett. 2011; 2:811–815.

4. Kottschade LA, Grotz TE, Dronca RS, et al. Rare presentations of primary melanoma and special populations: a systematic review. Am J Clin Oncol. 2014; 37:635–641.
7. Cohen T, Busam KJ, Patel A, Brady MS. Subungual melanoma: management considerations. Am J Surg. 2008; 195:244–248.

8. O’Leary JA, Berend KR, Johnson JL, Levin LS, Seigler HF. Subungual melanoma: a review of 93 cases with identification of prognostic variables. Clin Orthop Relat Res. 2000; (378):206–212.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download