Abstract
Hip arthroscopy is currently being leveraged in the diagnosis and treatment of a wide range of hip joint problems. In fact, great advancements in hip arthroscopy have resulted in an ever-expanding number of indications to which it is being applied. Minimally invasive hip arthroscopy allows for quicker initiation of rehabilitation and has attracted much attention as the field becomes increasingly focused on surgeries designed to preserve joints. This review aims to summarize the recent advances, applications, and impact of hip arthroscopy.
Hip arthroscopy was first described in 1931 by Burman1) who used it to view the inside of a joint in his cadaver studies; the first clinical description was made in 1939 by Takagi2). Despite the early clinical applications of hip arthroscopy, the procedure did not gain popularity until the 1970s. Since 1977, when Gross3) first introduced hip arthroscopy as treatment for congenital dislocation of the hip, Johnson4), Eriksson et al.5), and others have further applied the technique to the diagnosis, management, and surgical intervention of other hip joint ailments. Subsequently, the procedure became well established by Glick et al.6), Sampson7), and Villar8). who contributed to significant advances in surgical approaches and anatomical aspects. Conventionally, hip arthroscopy has been applied to i) helping to diagnose the cause of hip pain, ii) diagnosis and treatment of labral tears, iii) removal of loose bodies, and iv) management of degenerative arthritis, cartilage damage, synovial lesions, avascular necrosis of the femoral head, pyogenic arthritis and other conditions910111213). As femoroacetabular impingement has emerged as a major cause of hip pain1415), arthroscopy has become even more widely used161718). Recent advancements in hip arthroscopy focus on maximizing joint preservation and range of motion following surgeries designed to treat: i) extra-articular lesions and ii) intra-articular lesions. Examples of extra-articular injuries being treated with hip arthroscopy include: i) subspinal impingement, ii) internal and external snapping hip, iii) greater trochanteric pain syndrome, and iv) deep gluteal syndrome. Examples of intra-articular injuries being treated with hip arthroscopy include: i) arthroscopic-assisted reduction and internal fixation for hip joint fracture; ii) labral repair, refixation, and reconstruction; and iii) reconstruction of damaged ligament teres. Given the frequency and significance of updates occurring within the field, the aim of this review is to outline and discuss an ever-increasing number of new indications and therapeutic applications of hip arthroscopy.
Femoroacetabular impingement syndrome is recognized as a major cause of hip pain and acetabular labral tears in young adults. Although a number of authors have documented improvements in hip joint range of motion and clinical symptoms after arthroscopic surgery161718192021), this is not always the case. There are some reports in the literature describing unsatisfactory improvements in hip joint range of motion and clinical symptoms, most often as a result of impingement remaining due to inappropriate decompression and arthroplasty after surgery2223). Recent studies have reported that hip impingement syndrome may be caused by extra-articular impingement, in particular, AIIS impingement, in patients without improvement in symptoms after surgery242526). AIIS impingement is categorized into three morphological variants according to the AIIS classification system proposed by Hetsroni et al.25) (Table 1). Patients with AIIS impingement during hip flexion experienced pain in the distal end during flexion and internal rotation of the hip. These symptoms improved with bump resection in the AIIS 242526). Previously, open reduction using the Smith-Peterson approach was used; however, a minimally invasive approach can now be attempted using advanced hip arthroscopy techniques27). The authors presented a case showing symptom improvement following arthroscopic decompression (Fig. 1). It is important to note, however, that a number of precautions are recommended when performing arthroscopic resection of the AIIS. For instance, since the AIIS is the origin of the direct head of rectus femoris, excessive excision during arthroscopic decompression may lead to rectus femoris injuries and a decrease in knee extension strength. Interestingly, Hapa et al.28) suggested that: i) these risks are lower because the rectus femoris does not attach to the anteromedial AIIS, and ii) injuries significant enough to induce a decrease in hip flexion strength are less likely to occur because the rectus femoris attaches to the AIIS extensively when an additional incision is made at the proximal and lateral aspects. Regardless of the variances in the perceived risk of this approach, surgeons should be cautious about proceeding with surgery.
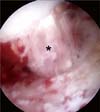
Snapping hip syndrome may be due to external or internal causes and is thus characterized as either “internal” or “external” snapping hip. Internal snapping hip is associated with pain and an audible snapping sound as a thickened iliopsoas muscle travels across the anterior aspect of the femoral head, joint capsule of the hip, or iliopectineal eminence. In hip arthroscopy, the anterior, anterolateral, and posterolateral portals are considered standard options. After insertion of the arthroscope through the anterolateral portal, the iliopsoas tendon can be exposed through incision over the anterior joint capsule via the anterior portal. Iliopsoas tendon release can be done arthroscopically. During this procedure, care must be taken to avoid injury to adjacent neurovascular structures. Internal snapping hip may also result from the protrusion of an acetabular cup, formation of abnormal angle of the iliopsoas tendon, and excessvie femoral anteversion after total hip arthroplasty293031). We achieved satisfactory results in improving the symptoms of internal snapping hip by performing arthroscopic iliopsoas release in a patient who complained of persisting pain at the anterior aspect of the hip after receiving total hip arthroplasty due to avascular necrosis (Fig. 2).
External snapping hip is accompanied by a snapping noise associated with a thickening of the iliotibial band as the iliotibial band slides over/catches on the greater trochanter during hip extension from a flexed position. This syndrome is often associated with inflammation and tenderness in the greater trochanteric bursa. Asymptomatic snapping hip resolves spontaneously and when accompanied with pain typically resolves with conservative treatment. Surgical management is implemented only when conservative treatment fails32). Resection of the greater trochanteric bursa and iliotibial band release can be attempted with an open procedure3334), and favorable outcomes have been reported using an arthroscopic procedure3536). Arthroscopic removal of the bursa can be performed to manage greater trochanteric pain syndrome accompanying chronic inflammation in the greater trochanteric bursa. A 30° angled arthroscope was placed in the inferior portal (viewing portal) by making portals 3 cm distal and 3 cm proximal to the tip of the greater trochanter, and the iliotibial band was released by inserting radiofrequency probes via the superior portal (working portal) (Fig. 3).
Deep gluteal syndrome describes the presence of sciatica arising from non-discogenic and extrapelvic entrapment of the sciatic nerve37). Structures involved in sciatic nerve entrapment within the gluteal space include the piriformis muscle3839), fibrous bands containing blood vessels and gluteal muscles40), hamstring muscles4142), the gemelli-obturator internus complex4344) and others. Recently, the term ‘deep gluteal syndrome’ is preferred over ‘piriformis syndrome’. Differential diagnosis of deep gluteal pain is essential to discriminate from hip pain arising from the vertebral column. For this reason, history taking and physical examination are crucial. Patients should be assessed for: i) radiating pain to the lower limbs, ii) abnormal nerve sensations, and iii) abnormal nerve reflex and muscle weakness in the sciatic nerve; importantly, taking a sitting position in a chair is often reported to be associated with sciatic nerve entrapment in piriformis muscle404546). Upon physical examination, active piriformis test and seated piriformis test can be carried out. Injection of local anesthetics and steroids has been described to be effective and physical therapy can be performed39). Surgical measures can be implemented when the condition does not improve with conservative treatment, and open procedure or arthroscopic surgery can be considered. Martin et al.40) and Dezawa et al.47) documented symptom improvement following sciatic nerve decompression using arthroscopy in patients with deep gluteal syndrome, and we ourselves have reported symptom improvement following arthroscopic decompression in a patient with this syndrome caused by cysts surrounding the sciatic nerve48). Therefore, radiological diagnosis (e.g., magnetic resonance imaging and other imaging tests) is required to examine soft tissues along the sciatic nerve in cases of persistent nondiscogenic sciatica of unknown genesis. Intra-articular abnormalities should be checked because paralabral cysts resemble the clinical manifestations of perineural cysts as increased intra-articular pressure is placed on the sciatic nerve (articular synovial theory)49). The authors used triangulation based on fluoroscopy-guided radiographs by creating additional portals along the upper part of, and 5 cm distal to, the posterior greater trochanter and by placing patients in a semiprone position. Cystostomy was conducted using basket forceps after confirming the sciatic nerve and adjacent cysts with unaided eyes, and symptoms improved in all cases (Fig. 4).
Multiple case reports have been published describing symptom improvements in patients with persistent pain caused by intra-articular loose bodies resulting from hip fracture and dislocation when these loose bodies are removed arthroscopically505152). In addition to mechanical actions of giant loose bodies and incongruency of the joint, Evans et al.53) showed, using an experimental model, that the etiology of traumatic arthritis seems to result from increased activity of chondrolytic enzymes by free cartilaginous particles remaining after a traumatic event. This provides a theoretical foundation for performing arthroscopy after hip fracture and dislocation. Hip fracture and dislocation are frequently associated with a tear of the anterior labrum which may generate post-injury joint pain and instability. For this reason, labral repair can be done using minimally invasive arthroscopic surgery when patients with labral tear complain of persisting pain after primary internal fixation in fractures5455). In recent years, direct reduction of fractures has been attempted using an arthroscope. Matsuda56) reported arthroscopic fixation of an isolated femoral head fracture, and Yang et al.57) and Kim et al.58) described case reports on the use of percutaneous screw fixation via an arthroscope for management of an acetabular fracture. Arthroscopic reduction of fractures allows surgeons to visualize the fractured joint surface and simultaneously enables arthroscopic treatment of intra-articular lesions (labral tear, removal of loose bodies) (Fig. 5).
The ligamentum teres was once considered to have no role in the stabilization of the hip joint; however, it is now recognized to contribute to the distribution of synovial fluid within the hip joint and internal stability. Importantly, it has also been shown to play a critical role in the flaccid joint capsule5960). According to Leunig et al.61), ligamentum teres injuries have shown to contribute to hip joint pain since this structure consists of free nerve endings involved in the production of pain, pressure, and deep sensation. Haviv and O'Donnell62) documented improvement in clinical symptoms after arthroscopic treatment for isolated ligamentum teres tears. Furthermore, using a cadaveric study, Kivlan et al.63) highlighted the key roles that the ligamentum teres plays including: i) stabilizing the hip joint during multi-plane movements involving flexion and abduction and ii) contributing to stability by providing tensile strength during flexion and abduction motions. Until recent years, ligamentum teres tears were commonly treated by debridement and shrinkage with either shavers or radiofrequency probes. However, a number of authors have recently investigated reconstruction of the ligamentum teres. Although Philippon et al.64) obtained favorable outcomes in a few patients, additional follow-up studies are warranted 64656667) (Fig. 6).
The labrum plays a significant role in increasing joint stability by trapping synovial fluid and sealing the central compartment6869). It has been suggested that labral injuries are a potential contributor to the early development of arthritis of the hip70). Thus, because of important functions of the labrum, sutures were used to repair labrum tears using an arthroscope. However, there are examples in which the structure was not preserved, (e.g., cases of severe injuries or defects to the labrum where it was not possible to use a suture because of significant degenerative changes). In these cases, debridement was performed following arthroscopic surgery. Recent studies have reported satisfactory results based on short-term follow-up by performing reconstruction of the iliotibial band, gracilis, ligamentum teres, and other structures where the native labrum cannot be preserved in patients of younger age7172) (Fig. 7).
Minimally invasive arthroscopy is widely used to diagnose and treat various hip joint problems. A variety of previously undetected diseases are being diagnosed as the anatomic characteristics and mechanisms of the hip joint are better understood and with recent advances in diagnostic imaging technology. Clinical applications of hip arthroscopy have expanded as a result of advancements in portal location, traction technique, surgical equipment, surgeons' accumulated experience in arthroscopic surgery and others. Surgery of intra-articular lesions has shifted from joint-reconstructive procedure using joint-replacement surgery to joint-preserving procedures in order to maintain clinical functions as much as possible and improve mid- and long-term quality of life. Minimally invasive surgical procedures are also increasingly preferred to treat extra-articular lesions. With these recent trends and minimally invasive surgical characteristics, hip arthroscopy is projected to be a safer and more effective treatment modality in diagnosing and treating extra- and intra-articular injuries of the hip.
Figures and Tables
Fig. 1
A 23-year-old man complained pain on flexion and limited range of motion in the right hip joint. (A) Preoperative axial computed tomography (CT) scan shows anterior inferior iliac spine (AIIS) extends distally to the acetabular rim. (B) Postoperative CT scan shows resected AIIS prominence.
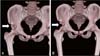
Fig. 2
A 33-year-old man who had anterior groin pain and limitation of flexion after total hip arthroplasty with a diagnosis of avascular necrosis of femoral head. After arthroscopic iliopsoas release (asterisk), his symptom was improved.

Fig. 3
Endoscopic iliotibial band releases in external snapping hip. (A) Triangulation under the fluoroscopy; Radiofrequency device in superior portal and 30° arthroscope in inferior portal. (B) Arthroscopic iliotibial band (ITB) release.

Fig. 4
Entrapment neuropathy of the sciatic nerve caused by perineural cyst. (A) Magnetic resonance imaging of perineural cyst. (B) Two portals are utilized; the posterolateral portal and the distal accessary portal (arrows). (C) Intraoperative arthroscopic images; the perineural cyst (asterisk). (D) Decompression with cystostomy of the perineural cyst.

Fig. 5
A 35-year-old man with traumatic hip fracture and islocation caused by pedestrian traffic accident. The dislocated hip was reducted in other hospital. (A) Preoperative axial computed tomography scan shows loose body in joint and posterior acetabular fracture (red circles). (B) Loose body removal (inset) and percutaneous screw fixation under arthroscopic guide.

Fig. 6
A 47-year-old female had large size of anterior capsular defect and acetabular labral tear. Despite of conservative treatement and arthroscopic labral repair, she had hip instability by recurrent anterior dislocation. After reconstruction of ligamentum teres (asterisk), she had no experience of hip dislocation.
References
1. Burman MS. Arthroscopy or the direct visualization of joints: an experimental cadaver study. 1931. Clin Orthop Relat Res. 2001; (390):5–9.
2. Takagi K. The classic. Arthroscope. Kenji Takagi. J. Jap. Orthop. Assoc., 1939. Clin Orthop Relat Res. 1982; (167):6–8.
3. Gross R. Arthroscopy in hip disorders in children. Orthop Rev. 1977; 9:43–49.
4. Johnson LL. Diagnostic and surgical arthroscopy. Clin Symp. 1982; 34:2–32.
5. Eriksson E, Arvidsson I, Arvidsson H. Diagnostic and operative arthroscopy of the hip. Orthopedics. 1986; 9:169–176.

6. Glick JM, Sampson TG, Gordon RB, Behr JT, Schmidt E. Hip arthroscopy by the lateral approach. Arthroscopy. 1987; 3:4–12.

8. Villar RN. Hip arthroscopy. Br J Hosp Med. 1992; 47:763–766.
9. Conn KS, Villar RN. [Labrum lesions from the viewpoint of arthroscopic hip surgery]. Orthopade. 1998; 27:699–703. German.
10. Dameron TB Jr. Bucket-handle tear of acetabular labrum accompanying posterior dislocation of the hip. J Bone Joint Surg Am. 1959; 41-A:131–134.

11. Petersilge CA, Haque MA, Petersilge WJ, Lewin JS, Lieberman JM, Buly R. Acetabular labral tears: evaluation with MR arthrography. Radiology. 1996; 200:231–235.

12. Santori N, Villar RN. Acetabular labral tears: result of arthroscopic partial limbectomy. Arthroscopy. 2000; 16:11–15.

13. Okada Y, Awaya G, Ikeda T, Tada H, Kamisato S, Futami T. Arthroscopic surgery for synovial chondromatosis of the hip. J Bone Joint Surg Br. 1989; 71:198–199.

14. Byrd JW. Hip arthroscopy: patient assessment and indications. Instr Course Lect. 2003; 52:711–719.
15. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003; (417):112–120.
16. Byrd JW. Hip arthroscopy. The supine position. Clin Sports Med. 2001; 20:703–731.
17. Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006; 25:299–308. ix

18. Philippon MJ, Stubbs AJ, Schenker ML, Maxwell RB, Ganz R, Leunig M. Arthroscopic management of femoroacetabular impingement: osteoplasty technique and literature review. Am J Sports Med. 2007; 35:1571–1580.

19. Bardakos NV, Vasconcelos JC, Villar RN. Early outcome of hip arthroscopy for femoroacetabular impingement: the role of femoral osteoplasty in symptomatic improvement. J Bone Joint Surg Br. 2008; 90:1570–1575.
20. Sampson TG. Arthroscopic treatment of femoroacetabular impingement. Am J Orthop (Belle Mead NJ). 2008; 37:608–612.

21. Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy. 2011; 27:1379–1388.

22. Trompeter A, Colegate-Stone T, Khakha R, Hull J. Hip arthroscopy for femoroacetabular impingement: results of 118 consecutive cases in a district general hospital. Hip Int. 2013; 23:400–405.

23. Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007; 35:1918–1921.

24. Hetsroni I, Larson CM, Dela Torre K, Zbeda RM, Magennis E, Kelly BT. Anterior inferior iliac spine deformity as an extraarticular source for hip impingement: a series of 10 patients treated with arthroscopic decompression. Arthroscopy. 2012; 28:1644–1653.

25. Hetsroni I, Poultsides L, Bedi A, Larson CM, Kelly BT. Anterior inferior iliac spine morphology correlates with hip range of motion: a classification system and dynamic model. Clin Orthop Relat Res. 2013; 471:2497–2503.

26. Pan H, Kawanabe K, Akiyama H, Goto K, Onishi E, Nakamura T. Operative treatment of hip impingement caused by hypertrophy of the anterior inferior iliac spine. J Bone Joint Surg Br. 2008; 90:677–679.

27. Larson CM, Kelly BT, Stone RM. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy. 2011; 27:1732–1737.

28. Hapa O, Bedi A, Gursan O, et al. Anatomic footprint of the direct head of the rectus femoris origin: cadaveric study and clinical series of hips after arthroscopic anterior inferior iliac spine/subspine decompression. Arthroscopy. 2013; 29:1932–1940.

29. Ward WT, Fleisch ID, Ganz R. Anatomy of the iliocapsularis muscle. Relevance to surgery of the hip. Clin Orthop Relat Res. 2000; (374):278–285.
30. Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004; (429):170–177.
31. Taher RT, Power RA. Iliopsoas tendon dysfunction as a cause of pain after total hip arthroplasty relieved by surgical release. J Arthroplasty. 2003; 18:387–388.

32. Jacobson T, Allen WC. Surgical correction of the snapping iliopsoas tendon. Am J Sports Med. 1990; 18:470–474.

33. Allen WC, Cope R. Coxa saltans: the snapping hip revisited. J Am Acad Orthop Surg. 1995; 3:303–308.

34. Provencher MT, Hofmeister EP, Muldoon MP. The surgical treatment of external coxa saltans (the snapping hip) by Z-plasty of the iliotibial band. Am J Sports Med. 2004; 32:470–476.

35. Ilizaliturri VM Jr, Martinez-Escalante FA, Chaidez PA, Camacho-Galindo J. Endoscopic iliotibial band release for external snapping hip syndrome. Arthroscopy. 2006; 22:505–510.

36. White RA, Hughes MS, Burd T, Hamann J, Allen WC. A new operative approach in the correction of external coxa saltans: the snapping hip. Am J Sports Med. 2004; 32:1504–1508.

37. McCrory P, Bell S. Nerve entrapment syndromes as a cause of pain in the hip, groin and buttock. Sports Med. 1999; 27:261–274.

39. Filler AG, Haynes J, Jordan SE, et al. Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine. 2005; 2:99–115.

40. Martin HD, Shears SA, Johnson JC, Smathers AM, Palmer IJ. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy. 2011; 27:172–181.

41. Puranen J, Orava S. The hamstring syndrome. A new diagnosis of gluteal sciatic pain. Am J Sports Med. 1988; 16:517–521.
42. Young IJ, van Riet RP, Bell SN. Surgical release for proximal hamstring syndrome. Am J Sports Med. 2008; 36:2372–2378.

43. Cox JM, Bakkum BW. Possible generators of retrotrochanteric gluteal and thigh pain: the gemelli-obturator internus complex. J Manipulative Physiol Ther. 2005; 28:534–538.

44. Meknas K, Kartus J, Letto JI, Christensen A, Johansen O. Surgical release of the internal obturator tendon for the treatment of retro-trochanteric pain syndrome: a prospective randomized study, with long-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2009; 17:1249–1256.

45. Benson ER, Schutzer SF. Posttraumatic piriformis syndrome: diagnosis and results of operative treatment. J Bone Joint Surg Am. 1999; 81:941–949.
46. Papadopoulos EC, Khan SN. Piriformis syndrome and low back pain: a new classification and review of the literature. Orthop Clin North Am. 2004; 35:65–71.

47. Dezawa A, Kusano S, Miki H. Arthroscopic release of the piriformis muscle under local anesthesia for piriformis syndrome. Arthroscopy. 2003; 19:554–557.

48. Lee WY, Hwang DS, Kang C, Zheng L. Entrapment neuropathy of the sciatic nerve caused by a paralabral cyst: three cases treated arthroscopically. JBJS Case Connect. 2016; 6:e82.

49. Young NP, Spinner RJ. Nerve cysts and joint relationship. In : Tubbs RS, Rizk E, Shoja MM, Loukas M, Barbaro N, Spinner RJ, editors. Nerves and nerve injuries. Vol. 2. Philadelpiha: Acdemic Press, Elsevier;2015. p. 935–943.
50. Byrd JW. Hip arthroscopy for posttraumatic loose fragments in the young active adult: three case reports. Clin J Sport Med. 1996; 6:129–133. discussion 133-4.
51. Mullis BH, Dahners LE. Hip arthroscopy to remove loose bodies after traumatic dislocation. J Orthop Trauma. 2006; 20:22–26.

52. Lansford T, Munns SW. Arthroscopic treatment of Pipkin type I femoral head fractures: a report of 2 cases. J Orthop Trauma. 2012; 26:e94–e96.
53. Evans CH, Mazzocchi RA, Nelson DD, Rubash HE. Experimental arthritis induced by intraarticular injection of allogenic cartilaginous particles into rabbit knees. Arthritis Rheum. 1984; 27:200–207.

54. Park MS, Yoon SJ, Choi SM. Hip Arthroscopic management for femoral head fractures and posterior acetabular wall fractures (Pipkin Type IV). Arthrosc Tech. 2013; 2:e221–e225.

55. Hwang JM, Hwang DS, Lee WY, Noh CK, Zheng L. Hip Arthroscopy for incarcerated acetabular labrum following reduction of traumatic hip dislocation: Three case reports. Hip Pelvis. 2016; 28:164–168.

56. Matsuda DK. A rare fracture, an even rarer treatment: the arthroscopic reduction and internal fixation of an isolated femoral head fracture. Arthroscopy. 2009; 25:408–412.

57. Yang JH, Chouhan DK, Oh KJ. Percutaneous screw fixation of acetabular fractures: applicability of hip arthroscopy. Arthroscopy. 2010; 26:1556–1561.

58. Kim H, Baek JH, Park SM, Ha YC. Arthroscopic reduction and internal fixation of acetabular fractures. Knee Surg Sports Traumatol Arthrosc. 2014; 22:867–870.

59. Guanche CA, Sikka RS. Acetabular labral tears with underlying chondromalacia: a possible association with high-level running. Arthroscopy. 2005; 21:580–585.

60. Martin HD, Savage A, Braly BA, Palmer IJ, Beall DP, Kelly B. The function of the hip capsular ligaments: a quantitative report. Arthroscopy. 2008; 24:188–195.

61. Leunig M, Beck M, Stauffer E, Hertel R, Ganz R. Free nerve endings in the ligamentum capitis femoris. Acta Orthop Scand. 2000; 71:452–454.

62. Haviv B, O'Donnell J. Arthroscopic debridement of the isolated Ligamentum Teres rupture. Knee Surg Sports Traumatol Arthrosc. 2011; 19:1510–1513.

63. Kivlan BR, Richard Clemente F, Martin RL, Martin HD. Function of the ligamentum teres during multi-planar movement of the hip joint. Knee Surg Sports Traumatol Arthrosc. 2013; 21:1664–1668.

64. Philippon MJ, Pennock A, Gaskill TR. Arthroscopic reconstruction of the ligamentum teres: technique and early outcomes. J Bone Joint Surg Br. 2012; 94:1494–1498.
65. Simpson JM, Field RE, Villar RN. Arthroscopic reconstruction of the ligamentum teres. Arthroscopy. 2011; 27:436–441.

66. Amenabar T, O'Donnell J. Arthroscopic ligamentum teres reconstruction using semitendinosus tendon: surgical technique and an unusual outcome. Arthrosc Tech. 2012; 1:e169–e174.

67. Lindner D, Sharp KG, Trenga AP, Stone J, Stake CE, Domb BG. Arthroscopic ligamentum teres reconstruction. Arthrosc Tech. 2012; 2:e21–e25.

68. Field RE, Rajakulendran K. The labro-acetabular complex. J Bone Joint Surg Am. 2011; 93:Suppl 2. 22–27.

69. Crawford MJ, Dy CJ, Alexander JW, et al. The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res. 2007; 465:16–22.

70. McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001; (393):25–37.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download