Abstract
Objectives
Materials and Methods
Results
Conclusion
Figures and Tables
 | Fig. 1Serial radiographs of the neck in lateral view. A. Hospital day 1: Soft-tissue swelling and presence of air in subcutaneous tissues of the submandibular space, anterior neck, and retropharyngeal space (arrows). B. Hospital day 2: Air in the submandibular space and middle region of the neck had been partially absorbed (arrows), while air remaining above the scapula could still be observed (dotted arrow). C. Hospital day 3. D. Last visit (9 days after onset): Air in the mandibular and cervical regions had almost disappeared (arrows). |
 | Fig. 2Computed tomography images showing subcutaneous emphysema (hospital day 1). A. Axial view: Right buccal, parapharyngeal, and retropharyngeal space (arrows). B. Coronal view: Submandibular and buccal space (arrows). C. Sagittal view: Submandibular space and anterior neck region (arrows); deep neck space (dotted arrow). D. Axial view at the level of the heart: Air can be seen in the middle mediastinum (arrow). |
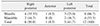
Table 1
Characteristics of the 11 patients included in this study

(F: female, M: male, RF: resin filling, RCT: root canal treatment, SAS: skeletal anchorage system, SD: standard deviation, CT: computed tomography, HU: Hounsfield unit, Anti: antibiotics, CS: cardiothoracic surgery, O2: oxygen-inhalation therapy, HP: hospitalization period, WBC: white blood cell count, Neut: neutrophil percentage, F/U: follow-up duration)
1Fisher's exact test. 2Mann-Whitney test.
3Teeth are numbered by Federation Dentaire Internationale tooth numbering system.
Table 2
Percentage of cases by air-orifice location
Values are presented as number (%).
Subcutaneous emphysema of one patient (patient no. 9; Table 1) occurred at two locations (upper right and lower right third molars). Thus, it was counted respectively.
Notes
Authors' Contributions C.H.J. participated in data collection, statistical analysis, and wrote the manuscript. S.Y. helped data collection and data analysis. S.W.C. reviewed and revised the manuscript. J.Y.K. reviewed and revised the manuscript. K.H.P. reviewed the manuscript critically. J.K.H. designed the study and reviewed the manuscript critically. All authors read and approved the final manuscript.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download