Abstract
A 59-year-old patient with a history of hepatocellular carcinoma presented with decreased consciousness and left hemiparesis. A rim-enhanced mass lesion without diffusion restriction was observed in contrast-enhanced MRI including diffusion-weighted imaging. Based on these findings, metastatic brain tumor was suspected. However, brain abscess (BA) was diagnosed after multiple bacterial colonies were observed in aspiration biopsy. Initial conventional antibiotic treatment including vancomycin had failed, so linezolid was used as second-line therapy. As a result, infection signs and clinical symptoms were resolved. We report a case with atypical imaging features and antibiotic susceptibility of a BA in an immunocompromised patient undergoing chemotherapy.
Brain abscess (BA) is a life-threatening central nervous system (CNS) infectious disease with substantial mortality and morbidity in spite of development in modality of cranial imaging, neurosurgical technique, and antimicrobial regimen [1]. BA is a dynamic focal form of intracranial suppuration that may progress rapidly and unexpectedly, irrespective of initial levels of disease severity [2]. The infectious origin of the BA causes significant damage to the CNS because of its incapability of mounting a sufficient defense against the pyogens [3]. For this reason, BA should be regarded as a serious infection and precise diagnosis and optimizing management should begin immediately for positive clinical outcomes [1]. However, only 20% of the patients with BA show the classic triad of fever, headache, and focal neurologic deficits [4]. In addition, laboratory studies add little to the diagnosis. Therefore, it is important to make a quick diagnosis through intracranial imaging when BA is suspected. CT is easily and widely used to convincingly make the diagnosis and locate the abscess. But to rely on CT alone can be difficult due to a number of other diseases showing similar symptoms and radiologic findings. Recently, magnetic resonance (MR) scans including diffusion-weighted imaging (DWI) have been very useful in early diagnosis because DWI has high sensitivity and specificity for the differentiation of BA from other nonabscess intracranial cystic lesion [5]. Unfortunately, not all abscesses follow this rule, and abscess showing lack of diffusion restriction in patients who have previously treated the tumor may cause considerable confusion in distinguishing between BA and necrotic tumors. It matters because the management of these two disease entities differs and can potentially affect the clinical outcome. Morbidity and mortality rate from a BA were significantly lower than in the past with advances in antimicrobials with greater cerebrospinal fluid (CSF) penetration. However, recently, there are many patients that do not respond to conventional therapy, such as vancomycin, due to the increase of the multi-drug resistant strain. Accordingly, this has increased the use of a new antibiotic, linezolid, and the effects have been reported to be superior [6]. Here, we describe a case of BA mimicking a brain tumor due to a lack of restricted diffusion, as well as being treated with linezolid because of refractoriness to standard treatment including vancomycin.
A 59-year-old male patient with chronic alcoholism and hepatitis B virus carrier was diagnosed with alcoholic liver cirrhosis and hepatocellular carcinoma (HCC) two years ago. Then, he received transcatheter arterial chemoembolization therapy three times and has been living without recurrence. The patient visited our emergency department with the symptoms of headache beginning 10 days prior and progressive left hemiparesis, altered mentality occurring two days prior. He was afebrile and his vital signs were stable. There were no leukocytosis and C-reactive protein (CRP) was 4.04 mg/L of blood. Upon a neurological examination, he was drowsy with disorientation and revealed decreased upper and lower extremities motor power to grade IV. DWI of the brain was performed because of suspicion of cerebral infarction. It showed a multi-lobulated cystic mass lesion and associated mild edema located in the right parieto-occipital lobe. We considered the possibility of a metastatic brain tumor at the first impression owing to negative diffusion restriction sign and a history of HCC. Contrast enhanced MRI combined with DWI revealed a multi-lobulated cystic rim-enhancing mass with surrounding edema and hypointensity in the cystic cavity on the DWI (Fig. 1). Stereotactic biopsy with aspiration was performed on the assumption of HCC multiple metastasis in the brain and the result revealed BA involving multiple bacterial colonies. However, because the bacteria was not cultured, an initial antimicrobial therapy was started on the basis of the standard empirical treatment that consists of vancomycin plus a third-generation cephalosporin and metronidazole. Despite the use of the above antimicrobial therapy, clinical deterioration with an increasing abscess size on cranial imaging (Fig. 2A, B) made further stereotactic aspiration and cultures including fungus, parasite and tuberculosis mycobacterium. The amount of vancomycin dosage was increased in order to increase the CSF concentration of vancomycin but intermittent spiking fever continued and patient's clinical symptoms did not improve. Even though there were no bacterial growth in the cultures, considering the situation that antimicrobialresistant gram-positive strains is increased, we had to change the previous antibiotics to linezolid which is excellent on CSF penetration. Then, infection signs including fever, erythrocyte sedimentation rate, CRP, and leukocytosis were decreased immediately. The abscess size was also reduced in follow up brain CT after about 4 weeks of using the antibiotics (Fig. 2C, D) and the post-linezolid clinical course was uneventful. This case was approved by the Institutional Review Board of the hospital (EMCIRB18-77).
BA is a focal suppurative intracranial infection that begins as a localized area of cerebritis and develops into a collection of pus surrounded by a well-vascularized capsule. Its causative agent is bacteria, mycobacteria, fungus, or parasite and the reported incidence ranges from 0.4 to 0.9 cases per 100,000 population [7]. The rate of BAs of intracranial mass lesions is 8% in developing countries, whereas in the West the rate is 1–2% [8]. The most common isolated organisms are Streptococcus and Staphylococcus species. BA is known to often occur in immunocompromised patients who have underlying disease such as human immunodeficiency virus (HIV) infection, a history of treatment with immunosuppressive drugs, disrupted natural protective barriers surrounding the brain, or a systemic source of infection [4]. There are no pathognomonic clinical signs of BA. Nevertheless, the most common clinical symptom is headache, and the triad of symptom including fever and neurological deficit can be seen in 15–30% of patients [9]. A number of neurological symptoms may appear depending on the location of the abscess and up to 25% of patients present with seizures [4]. The differential diagnosis includes brain tumor, stroke, bacterial meningitis, epidural abscess, subdural empyema and CNS lymphoma in patients infected with HIV [1].
Intracranial imaging is important to the immediate diagnosis of BA, because it gives information for stereotactic localization and is useful for monitoring response following the treatment. From the advent of CT era, the diagnosis of BAs has become easier and less invasive. But BAs appear as ring-enhancing lesions in contrast enhanced CT along with a variety of other diseases, such as metastatic tumor, high-grade gliomas, cerebral infarction, resolving cerebral hematoma, lymphoma, toxoplasmosis, demyelinating disease, and radiation necrosis, which all can have similar patterns [10]. MRI is more sensitive than CT in the detection of BA as follows [11]: 1) It has greater sensitivity to changes in tissue water content, resulting in greater contrast between edematous brain and normal brain during the abscess formation; 2) It facilitates exact localization, accurate characterization, and staging of the abscess; 3) It better demonstrates the complications from BA including intracranial herniation, meningitis, venous thrombosis and ventriculitis. The characteristic MRI features of the necrotic center of a mature BA include fluid hyperintense relative to CSF and hypointense relative to white matter on the T1-weighted sequence. On T2-weighted sequences, the fluid in the abscess cavity is iso- to hyperintense to CSF and gray matter. This characteristic pattern of T2 prolongation relative to normal brain and T1 shortening relative to CSF reflects the proteinaceous nature of the abscess fluid. In immunocompromised patients with an impaired inflammatory response, there may be a lack of ring enhancement and less vasogenic edema in comparison with immunocompetent patients, a feature which is considered to be a poor prognostic finding [12]. When the contrast-enhanced MRI including DWI is performed, abscess is defined as a rimenhancing lesion which shows diffusion restriction. Diffusion restriction is defined as hyperintense signals on diffusion imaging with corresponding hypointense signals on apparentdiffusion-coefficient (ADC) imaging. The reason for restricted diffusion characteristic in the cavity of a BA is thought to be necrotic debris, macromolecules, highly viscous proteinaceous exudates, viable bacteria and inflammatory cells in the abscess cavity while necrotic material in tumors contains necrotic tissue debris, fewer inflammatory cells, and much clearer serous fluid [13]. Most necrotic tumors show mildly increased diffusion with low-to-intermediate signal intensity on DWI and high ADC values. The sensitivity and specificity of DWI for the differentiation of BAs from non-abscesses lesion was 96% and 96%, respectively [14]. However, restricted diffusion within a ring-enhancing mass is characteristic, but not pathognomonic of a BA. Facilitated diffusion in abscess might result from changes in pus composition reflects adequate antibiotic therapy, variable concentrations of inflammatory cells, different pathogenic organisms, the host immune response, and the age of an abscess might influence pus viscosity [13]. There are some reports of facilitated diffusion within pyogenic abscess cavity when empiric antimicrobial chemotherapy has preceded imaging [15]. Fungal and tuberculous abscesses may have elevated diffusivity and a low signal on DWI. The lack of an inflammatory response may be explained by the combination of the patient's immunocompromised state and the character of the infection that cause little inflammatory reaction such as Bacillus cereus [13]. We initially suspected a metastatic brain tumor in our case because the patient had a past history of HCC treatment and MR image revealed a ring-enhanced lesion in the absence of restriction. We inferred that the cause of low intensity on DWI probably is due to the little inflammatory reaction by the combination of the patient's immunocompromised state and the character of the infection among possibilities mentioned above. In addition, susceptibility-weighted imaging (SWI) or proton MR spectroscopy (PMRS) is helpful in distinguishing BA from intracranial cystic tumors. One study demonstrated the importance of SWI in the differentiation of necrotic glioblastomas and pyogenic abscesses, emphasizing the “dual-rim sign” visible on SWI, as the most specific imaging feature differentiating between them [16]. A number of PMRS studies have been used to characterize intracranial mass lesions and amino acid resonance is a sensitive marker of pyogenic abscesses although its absence does not rule out a pyogenic etiology [17].
An initial empirical antibiotic used in case of a BA is glycopeptides, typically vancomycin. However, as in our case, the antibiotic treatment including vancomycin often failed due to the increasing prevalence of vancomycin-resistant strains and limited and unpredictable penetration into the CSF. Recently, oxazolidinone derivative linezolid, which has good tissue penetration into CSF through the blood-brain barrier, has been used as a new antibiotic in the treatment of CNS gram-positive infections. Its anti-bacterial mechanism is binding to the 50S subunit of the ribosome and prevents formation of the initiation complex for protein synthesis [18]. Also, it has excellent bioavailability through the oral route of administration and no dose modification is needed in mild to moderate liver disease or any degree of renal impairment [6]. Therefore, outpatient follow-up with oral therapy may be an attractive option in terms of cost-effectiveness if conventional intravenous antibiotic therapy is required for a long period. The common adverse events are diarrhea, nausea and headache, without need for discontinuation of treatment. Also, neuritis, lactic acidosis, myelotoxic effects and thrombocytopenia were reported in rare cases leading to discontinuation of administration, especially when the treatment duration is prolonged [19]. The cause for peripheral and optic neuropathy is unknown but it is associated with prolonged linezolid treatment over a 4 week period [20]. The symptoms that usually manifest are paresthesia and numbness of the distal extremities and painless sudden-onset central vision loss, decreasing visual acuity and loss of color vision [19]. In this case, optic neuropathy can be recovered after immediate discontinuation of treatment but some of this deficit may remain. However, the symptom of peripheral neuropathy is not recovered well even after the drug is discontinued. Moreover, hematologic abnormalities such as thrombocytopenia and myelosuppression usually occur during prolonged treatment of more than 14 days and therefore, complete blood counts should be monitored weekly [20]. Although there are some adverse events mentioned above, the rate of adversity was not as high compared to other previous antibiotics. Few significant side effects have occurred when used within a short period of 4 weeks. Therefore, linezolid can be thought of as a tolerable and safety drug [19]. Given these many advantages, the new generation antibiotics, linezolid, may be considered for the treatment of multi-drug resistant gram-positive cocci CNS infection in case of failure of first-line therapy.
Although DWI provide an excellent capacity showing a high sensitivity and specificity in the diagnosis of BAs, it is still difficult to differentiate BAs from other intracranial cystic lesions. Therefore, it is important to increase the awareness of atypical image findings of BAs and complement it with multimodal study of advanced imaging to improve diagnostic confidence in case of uncertainty. In addition, linezolid, which has higher CSF penetration and exhibit better efficacy, may be considered for patients who do not respond to conventional empirical antibiotic therapy.
Figures and Tables
Fig. 1
Preoperative MRI images. A: T2-weighted fluid attenuated inversion recovery axial magnetic resonance (MR) image shows a multilobulated cystic mass lesion in the right parieto-occipital lobe with hemorrhagic and necrotic change. B: Rim enhancement mass-like lesions on post-contrast T1-weighted axial MR image. C: Diffusion-weighted MR image shows hypointensity in the cavity. D: Corresponding hypointensity on the apparent diffusion coefficient map.

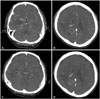
Fig. 2
Axial contrast-enhanced CT images showing multiple cystic lesions with rim enhancement in temporal and occipital lobe. A and B: About 3 weeks after the initial antibiotic treatment including vancomycin. C and D: After secondary abscess aspiration and a change in antibiotics as linezolid 4 weeks later.
References
2. Nathoo N, Nadvi SS, Narotam PK, van Dellen JR. Brain abscess: management and outcome analysis of a computed tomography era experience with 973 patients. World Neurosurg. 2011; 75:716–726. discussion 612-7.

3. Britt RH, Enzmann DR, Yeager AS. Neuropathological and computerized tomographic findings in experimental brain abscess. J Neurosurg. 1981; 55:590–603.

4. Brouwer MC, Coutinho JM, van de Beek D. Clinical characteristics and outcome of brain abscess: systematic review and meta-analysis. Neurology. 2014; 82:806–813.

5. Xu XX, Li B, Yang HF, et al. Can diffusion-weighted imaging be used to differentiate brain abscess from other ring-enhancing brain lesions? A meta-analysis. Clin Radiol. 2014; 69:909–915.

6. Birmingham MC, Rayner CR, Meagher AK, Flavin SM, Batts DH, Schentag JJ. Linezolid for the treatment of multidrug-resistant, grampositive infections: experience from a compassionate-use program. Clin Infect Dis. 2003; 36:159–168.

7. Helweg-Larsen J, Astradsson A, Richhall H, Erdal J, Laursen A, Brennum J. Pyogenic brain abscess, a 15 year survey. BMC Infect Dis. 2012; 12:332.

9. Xiao F, Tseng MY, Teng LJ, Tseng HM, Tsai JC. Brain abscess: clinical experience and analysis of prognostic factors. Surg Neurol. 2005; 63:442–449. discussion 449-50.

11. Goodkin HP, Harper MB, Pomeroy SL. Intracerebral abscess in children: historical trends at Children's Hospital Boston. Pediatrics. 2004; 113:1765–1770.

12. Yuh WT, Nguyen HD, Gao F, et al. Brain parenchymal infection in bone marrow transplantation patients: CT and MR findings. AJR Am J Roentgenol. 1994; 162:425–430.

13. Ozbayrak M, Ulus OS, Berkman MZ, Kocagoz S, Karaarslan E. Atypical pyogenic brain abscess evaluation by diffusion-weighted imaging: diagnosis with multimodality MR imaging. Jpn J Radiol. 2015; 33:668–671.

14. Reddy JS, Mishra AM, Behari S, et al. The role of diffusion-weighted imaging in the differential diagnosis of intracranial cystic mass lesions: a report of 147 lesions. Surg Neurol. 2006; 66:246–250. discussion 250-1.

15. Nath K, Agarwal M, Ramola M, et al. Role of diffusion tensor imaging metrics and in vivo proton magnetic resonance spectroscopy in the differential diagnosis of cystic intracranial mass lesions. Magn Reson Imaging. 2009; 27:198–206.

16. Toh CH, Wei KC, Chang CN, et al. Differentiation of pyogenic brain abscesses from necrotic glioblastomas with use of susceptibility-weighted imaging. AJNR Am J Neuroradiol. 2012; 33:1534–1538.

17. Pal D, Bhattacharyya A, Husain M, Prasad KN, Pandey CM, Gupta RK. In vivo proton MR spectroscopy evaluation of pyogenic brain abscesses: a report of 194 cases. AJNR Am J Neuroradiol. 2010; 31:360–366.

18. Livermore DM. Linezolid in vitro: mechanism and antibacterial spectrum. J Antimicrob Chemother. 2003; 51:Suppl 2. ii9–ii16.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download