Dear Editor:
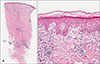
A 53-year-old man presented with asymptomatic skin lesions that had persisted for a week on his back. He had been diagnosed with cutaneous lupus erythematosus 10 years prior and had been taking medication for it occasionally. He did not complain of other systemic symptoms of lupus erythematosus related to renal function, joint, or neurologic function. The physical examination revealed multiple grouped erythematous papules on his back, initial differential diagnosis included herpes infection, insect bite, and prurigo simplex (Fig. 1). As erythematous grouped vesiculopapules are characteristic features of herpes infection and back is common affected site of herpes zoster, herpes infection was highly suggested based on clinical background. Laboratory test showed elevation of antinuclear antibody titer (1:320, speckled type) and the other laboratory results including anti-DNA antibody and complement levels were within normal limit. A skin punch biopsy was performed on one of the papules. Hematoxylin-eosin staining showed a lymphohistiocytic infiltration along the dermoepidermal junction and around appendages, from the superficial to the deep dermis (Fig. 2A). In addition, there were hydropic changes in the epidermal basal layer and mild mucin deposition in the dermis (Fig. 2B). The patient was diagnosed with cutaneous lupus erythematosus (CLE) and was treated with oral prednisolone (5 mg) and hydroxychloroquine (200 mg) twice a day and a topical mometasone furoate 0.01% cream once a day. After 6 weeks, the rash resolved with hyperpigmentation and scars. We received the patient's consent form about publishing all photographic materials.
CLE can manifest as a variety of skin conditions1. According to the classification proposed by Gilliam and Sontheimer, the cutaneous lesions of CLE are largely divided into LE-specific and LE-nonspecific skin lesions, based on the presence or absence of interface dermatitis2. In other words, LE-specific lesions show inflammatory infiltration in the basal membrane zone of the interfollicular epidermis and can be subdivided into acute, subacute, and chronic, according to the clinical morphology. In the present case, the lesions appeared to be symptomatic of chronic CLE because the lesions showed histopathologic features of interface dermatitis and healed with scars after treatment. However, discoid LE, the most common form of CLE, manifests as erythematous-infiltrated coin-shaped plaques with hyperkeratosis in the center, not as multiple grouped papules as in this case. In addition, the known rare and atypical manifestations of chronic CLE such as lichenoid, edematous, or hemorrhagic LE do not resemble the manifestation in this case1.
Regarding the manifestation of CLE along the dermatomes, two cases of systemic LE appeared on a previously affected site of herpes zoster have been reported34. Though, there were no reports that LE showed different clinical features as grouped papules like this study.
In conclusion, we report the atypical case of CLE presenting as localized erythematous grouped papules mimicking herpes infection in an adult. This manifestation adds to the various known clinical features of CLE, and should raise suspicions of CLE when encountered.
Figures and Tables
References
1. Obermoser G, Sontheimer RD, Zelger B. Overview of common, rare and atypical manifestations of cutaneous lupus erythematosus and histopathological correlates. Lupus. 2010; 19:1050–1070.

2. Costner MI, Sontheimer RD, Provost TT. Lupus erythematosus. In : Sontheimer RD, Provost TT, editors. Cutaneous manifestations of rheumatic diseases. 2nd ed. Philadelphia: Lippincott Williams and Wilkins;2004. p. 15–64.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download