Abstract
Immunoglobulin G4 (IgG4)-related lung disease has been actively studied over the past few years. Radiologic findings of IgG4-related lung disease vary among patients, but there are no long-term follow up studies regarding variations in imaging features over the course of disease progression. In two cases with relatively long-term follow up, diverse early and late computed tomography (CT) findings of IgG4-related lung disease are reviewed in this report. In contrast to nodular or diffuse ground-glass opacity, which was predominantly noted in CT scans at earlier stages of disease, honeycombing and traction bronchiectasis were regarded as late radiologic manifestations. Solid nodules might be visible in both early and late stages; however, development of new solid nodules and enlargement of preexisting nodules could occur during disease progression. Interlobular septal thickening and mediastinal/hilar lymphadenopathy were persistent, even in later stages of the disease. These findings might be useful in making an accurate and timely diagnosis of IgG4-related lung disease.
Immunoglobulin G4 (IgG4)-related disease is still a poorly understood systemic condition having specific histologic features related to inflammation and fibrosis. Particularly, imaging findings of IgG4-related disease involving the lungs have many components to be identified. The objective of this report is to reveal variable imaging features which might be masked during the course of disease process. Here, we are reporting cases of two patients with pathologically proven IgG4-related lung disease, focused on the sequential imaging findings of disease.
A 73-year-old male presented with general weakness and dyspnea for 1 month, and 3 kg of weight loss over 5 months. He had a past history of occupational exposure to carbon disulfide for 20 years and a history of right hemicolectomy due to colon cancer 25 years ago. He was an ex-smoker who quit smoking 30 years ago and had a 22 pack-year smoking history. No significant findings were demonstrated upon physical examination. Initial laboratory tests showed an elevated C-reactive protein (6.55 mg/L) and erythrocyte sedimentation rate levels (21 mm/h); the total white blood cell count (WBC) was in a normal range (8.0 × 109/L), but the ratio of neutrophil was mildly increased (76.4%). Tumor markers, including alpha-fetoprotein, carcinoembryonic antigen, cancer antigen 19–9, and squamous cell carcinoma antigen were all within a normal range. A chest radiograph showed a patchy increased opacity in the right upper lobe.
A chest CT was conducted for further evaluation, and it revealed two spiculated nodular consolidations with an air bronchogram in the right upper lobe (Fig. 1A). The lesions showed a slightly heterogeneous contrast enhancement (about 86 Hounsfield units) and the longest diameters of these two lesions were 21 and 22 mm, respectively. An approximately 4 mm sized satellite ground-glass nodule was shown adjacent to the larger one. Diffuse and nodular wall thickening of trachea and esophagus was also noted, but mediastinal lymph nodes were unremarkable. The first clinical impression was primary lung cancer, and a radiologic differential diagnosis included focal pneumonia such as fungal pneumonia and granulomatous inflammation. The pathologic specimen obtained by a percutaneous core needle biopsy (PCNB) revealed interstitial chronic inflammation with organizing fibrosis. There was neither granuloma nor fungal hyphae in the specimen, proven by Periodic acid-Schiff and Grocott's methenamine silver stains.
In the follow-up chest CT 3 months later, previous consolidative lesions were slightly decreased in size (21 mm → 16 mm, 22 mm → 16 mm). However, about 5 mm to 7 mm sized new noncalcified nodular lesions had developed in both upper lobes. Over this period, no specific medication for these lesions was taken except for antibiotics. Additional follow-up chest CT after 7 months showed a markedly increased size in the prior lesions of both upper lobes. The largest one was measured to be 32 mm in size. The next follow-up chest CT was also taken 7 months later with contrast enhancement. In this CT scan, a mass larger than 5 cm was shown in the right upper lobe (Fig. 1B). This mass was thought to be enlarged and coalesced previous nodular lesions in the right upper lobe. Significant enlargement of a spiculated nodule in the left upper lobe was also noted (14 mm → 22 mm). In addition, prominent interstitium and interstitial nodules were shown in both upper lobes, with progression of tracheal and esophageal wall thickening (Fig. 1C). Multiple mediastinal, right hilar and interlobar lymph nodes were also enlarged. For all these findings, primary lung cancer with multiple metastasis involving both lungs and mediastinum was considered to be a radiologic impression, and PCNB was repeated for pathologic confirmation. Fibrosclerotic lesion with lymphoplasmacytic infiltration was finally reported with 20 cells of IgG4-positive plasma cells per high-power field, and the ratio of IgG4-positive plasma cell to IgG-positive plasma cell was 0.34 (34%). There were neither granulomas nor malignant cells in the specimen. The level of serum IgG4 was slightly elevated (91.8 mg/dL). By the comprehensive diagnostic criteria for a IgG4-related disease, a diagnosis of IgG4-related lung disease was probable in this patient (1).
A 65-year-old male with a history of carcinoid tumor in the stomach was incidentally found to have abnormal findings in the basal lungs on a contrast-enhanced stomach CT scan. He was a non-smoker and had a past history of old pulmonary tuberculosis, which was cured 30 years ago. A physical examination was unremarkable and revealed no issues. Initial laboratory findings were compatible with systemic lupus erythematosus; decreased levels of serum C3 (16.2 mg/dL) and C4 (3.47 mg/dL), decreased total count of WBC (3.7 × 109/L and 2.93 × 109/L, measured consecutively), high titer of fluorescent antinuclear antibody (> 1:1280) with a homogeneous pattern, and a positive serum anti-dsDNA. A chest radiograph showed bronchiectasis in the left lower lung zone and an inactive pulmonary tuberculosis lesion in the right upper lobe.
In the chest CT scan after an endoscopic mucosal resection of carcinoid tumor, localized bronchiectasis and multiple nonspecific small nodules were shown in the left lower lobe and lingular segment of the left upper lobe. Paraseptal emphysema was found in the left lower lobe and calcified nodules with fibrotic bands in the right upper lobe. Since he did not have any respiratory complaints, no further evaluation but observation was performed.
Three years later, he was hospitalized due to dyspnea developed one day before, along with coughing and sputum for fifteen days. Crackle was audible in the right lower lung field, and bilateral patchy increased opacity was noted on the chest radiograph. Despite the administration of antibiotics for three days under the impression of pneumonia, clinical symptoms and radiologic findings had not improved. In a high-resolution CT scan for further evaluation, multifocal diffuse and patchy groundglass opacity (GGO) with interlobular septal thickening in both lungs were characteristic findings (Fig. 2A). Additionally, focal nodular consolidations in the area of subpleural GGO were demonstrated in the right upper and lower lobes. With slightly increased extent of emphysematous change in the left lower lobe, bronchiectasis in both lungs was also observed. For these bilateral diffuse and subpleural GGO with focal nodular consolidations, atypical pneumonia such as Pneumocystis jirovecii pneumonia was suggested as a possible differential diagnosis. However, bronchoalveolar lavage did not reveal any pathogens, so a video-assisted thoracoscopic surgery biopsy targeted for consolidative lesions in the right lung was performed. Biopsies from the right upper and lower lobes showed diffuse alveolar damage in interstitial lung disease of an undetermined type associated with IgG4-related lung disease. Diffuse lymphoplasmacytic infiltration and increased IgG4-positive plasma cells (IgG4-positive plasma cell to IgG-positive plasma cell ratio: about 0.28) were shown in fibrotic stroma. Initial serum IgG4 concentration of the patient was significantly elevated (275.98 mg/dL). By the comprehensive diagnostic criteria for IgG4-related disease, a diagnosis of IgG4-related lung disease was definite in this patient (1). The patient had started glucocorticoid therapy.
One month later, a follow-up chest CT was done and it revealed a newly developed extensive consolidation with air bronchogram, predominant in the right lung (Fig. 2B). Instead, prior GGO lesions showed a slight decrease. Next, a follow-up CT taken 8 months later demonstrated peripherally located reticular densities, replacing the previous consolidation and GGO areas. Honeycombing cysts in both basal lungs were the key image finding in this CT scan. Progression of traction bronchiectasis in both lungs was also noted. Steroid administration was completely tapered off at this time. Aggravation of these honeycombing cysts and fibrosis was shown in the last follow-up CT four years later, combined with a new nodular lesion in the right upper lobe and multiple enlarged mediastinal lymph nodes (Fig. 2C).
IgG4-related diseases have recently attracted significant interest over the last decade, since Hamano et al. (2) first reported the elevation of serum IgG4 concentration in patients with sclerosing pancreatitis in 2001. The existence of IgG4-related disease was proposed in 2003, which could involve not only the pancreas but also multiple extrapancreatic organs such as the bile duct, retroperitoneum, liver, salivary glands, etc (3). It is characterized by diffuse lymphoplasmacytic infiltration, fibrosis, and numerous IgG4-positive plasma cells in affected organs with or without elevated serum IgG4 concentrations (4).
IgG4-related lung disease accounts for about 14% to 54% of patients with IgG4-related disease, and the first case was reported in 2004 (5). Inoue et al. (6) found that IgG4-related lung disease presents a wide spectrum of radiologic features and can be categorized into four major subtypes: solid nodular type, round-shaped GGO type, alveolar interstitial type, and bronchovascular type. Due to an absence of follow-up image analysis, however, these categories have limitations in terms of the course of disease.
To the best of our knowledge, long-term follow up data has not been published yet and the prognosis of IgG4-related lung disease is still unclear. It is known that most patients respond well to steroid therapy but relapses are common, ranging from 20% to 30% after tapering of glucocorticoid (7). Although early intervention may show improvement of long-term outcomes in specific organ systems, it is still under debate whether medical treatment, such as glucocorticoids, in early stage of disease can modify the long-term disease course (8). Since all patients must be given proper treatment once a diagnosis is made, few details are known about the “pure” natural history of IgG4-related lung disease.
Our first case demonstrates, relatively well, the natural course of disease progression. No specific treatment for IgG4-related disease was performed until the last CT scan due to unintentional delayed diagnosis. Overall, the radiologic subtype progressed from a solid nodular type to mixed solid nodular and bronchovascular type in the last follow-up chest CT scan. A development of new solid nodules and an increase in size of pre-existing nodules between intervals might be one of the key CT findings, however, the progression of the radiologic subtype is also a remarkable finding. Features of the bronchovascular type, which the patient revealed, include a thickened interlobular septa and an enlargement of lymph nodes in the hilum and mediastinum. These findings well represent perilymphatic involvement, the most important and characteristic nature of IgG4-related lung disease (4). In addition, there was diffuse wall thickening of the trachea and esophagus, which is also an unusual and interesting finding.
The latter case shows findings that are more variable. In this case, it transitioned grossly from a round-shaped GGO type to an alveolar interstitial type. Initially, only multiple nodular GGO lesions and localized bronchiectasis were observed. These nodular GGO lesions were more diffuse and patchy in the second CT scan with a few focal nodular consolidations. In spite of intravenous steroid therapy, prior diffuse GGO areas changed into extensive consolidation with air bronchogram, like that of pneumonia. This is rather an atypical manifestation and does not belong to any of the four major subtypes. Kobayashi et al. (9) reported extensive airspace consolidation involving both upper and lower lobes in IgG4-related lung disease. In the end, bilateral and diffuse consolidative lesions evolved into reticular densities with honeycombing cysts and traction bronchiectasis, suggesting pulmonary fibrosis. These are the findings of the alveolar interstitial type. It seems like glucocorticoid did not play an important role in the prevention of disease progression in this case. Although there have been several reports about interstitial lung disease associated with IgG4-related lung disease, it is unclear whether IgG4-related lung disease causes interstitial lung disease or not (9).
In summary, these two cases represent a tumor-mimicking lesion formerly known as pulmonary inflammatory pseudotumor and an interstitial pneumonia-like lesion, respectively. All these various imaging findings are thought to be a part of a morphological spectrum in the same pathologic process, not a distinct pathologic condition (6). Therefore, an attempt to categorize the above findings by chronological order might be meaningful. We briefly reviewed the CT manifestations in early and late stages of our two cases.
Just as in usual interstitial pneumonia, GGO can be considered an early active lesion in our cases. Newly developed solid nodules were an initial finding of disease in the former case, and these nodules enlarged or coalesced into a larger mass as the disease progressed. In contrast, honeycombing and traction bronchiectasis suggest a late stage which is already progressed into fibrosis and an irreversible state. Mediastinal/hilar lymphadenopathy and interlobular septal thickening persist into advanced stage in both of our cases, suggesting perilymphatic involvement throughout the course of disease. Considering all these characteristics, the findings of perilymphatic involvement are likely to be shown even in later stage of the disease, and honeycombing and traction bronchiectasis might develop typically in advanced stage. However, because of limited findings in our cases, further large trials investigating the relationship of CT features with the natural course of IgG4-related lung disease should be conducted to overcome the limitations of this study.
In conclusion, we propose that the radiologic subtype of IgG4-related lung disease can vary during the natural course of disease, even in the same patient, and not only between different individuals. With two cases of relatively long-term follow up, we were able to ascertain variable early and late CT findings of IgG4-related lung disease. If a patient with suspicious IgG4-related lung disease has early radiologic features, especially with atypical manifestations of tumor or pneumonia, these may be helpful in establishing the correct and timely diagnosis through correlation with clinical and serologic evaluations leading to pathologic confirmation.
Figures and Tables
 | Fig. 1Contrast enhanced serial chest CT scans in a 73-year-old male (case 1) with immunoglobulin G4-related lung disease.
A. Spiculated nodular consolidation with air bronchogram is shown in the right upper lobe.
B. After 17 months, follow-up chest CT scan reveals a mass larger than 5 cm in the right upper lobe.
C. Interlobular septal thickening with satellite nodules are shown in both upper lobes (left), and diffuse and nodular wall thickening of the trachea and esophagus with interval aggravation is simultaneously noted in this CT scan (right).
|
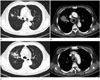
 | Fig. 2Serial chest CT scans in a 65-year-old male (case 2) with immunoglobulin G4-related lung disease.
A. Multifocal diffuse and patchy ground-glass opacities are noted in the bilateral lungs.
B. In the follow-up CT taken 1 month later, extensive consolidations with air bronchogram are shown in both lungs with right lung predominancy.
C. The last follow-up CT scan taken in 40 months reveals honeycombing and traction bronchiectasis in both basal lungs.
|
References
1. Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012; 22:21–30.

2. Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001; 344:732–738.

3. Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003; 38:982–984.

4. Matsui S, Hebisawa A, Sakai F, Yamamoto H, Terasaki Y, Kurihara Y, et al. Immunoglobulin G4-related lung disease: clinicoradiological and pathological features. Respirology. 2013; 18:480–487.

5. Ryu JH, Sekiguchi H, Yi ES. Pulmonary manifestations of immunoglobulin G4-related sclerosing disease. Eur Respir J. 2012; 39:180–186.

6. Inoue D, Zen Y, Abo H, Gabata T, Demachi H, Kobayashi T, et al. Immunoglobulin G4–related lung disease: CT findings with pathologic correlations. Radiology. 2009; 251:260–270.

7. Yamamoto M, Takahashi H, Ishigami K, Yajima H, Shimizu Y, Tabeya T, et al. Relapse patterns in IgG4-related disease. Ann Rheum Dis. 2012; 71:1755.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download