INTRODUCTION
MATERIALS AND METHODS
Patient Population
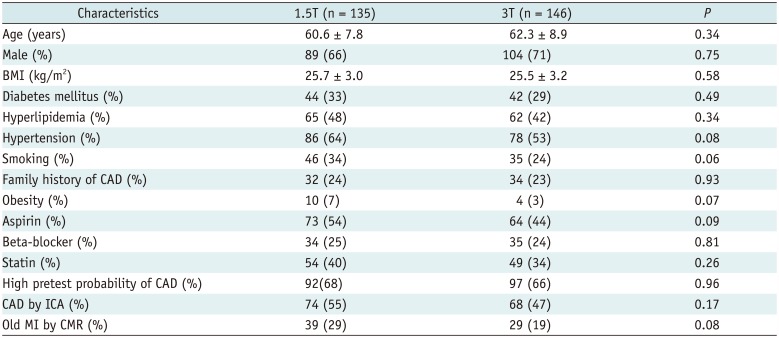
CMR Protocol
Table 1
Comparison of Scan Parameters between 1.5T vs. 3T CMR Perfusion Imaging
CMR Analysis
ICA Protocol and Analysis
Statistical Analysis
RESULTS
Baseline Characteristics
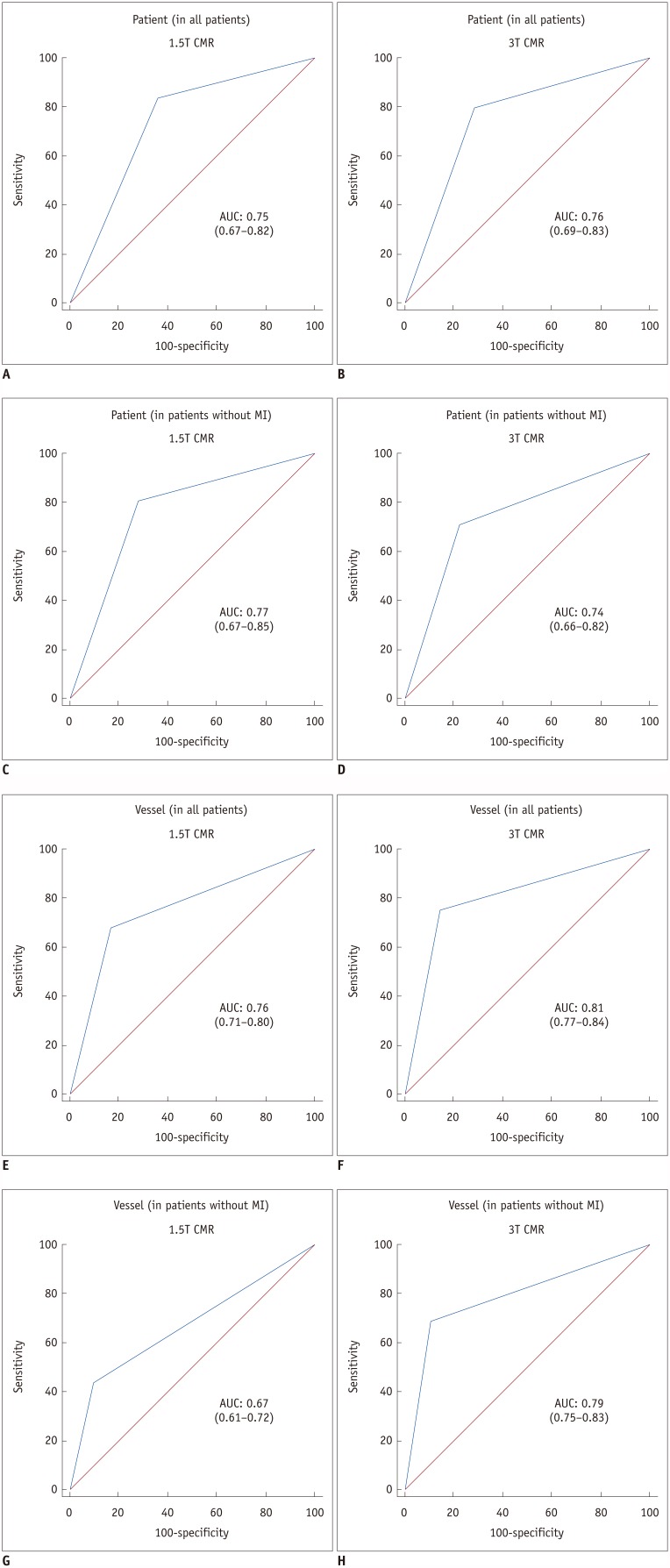
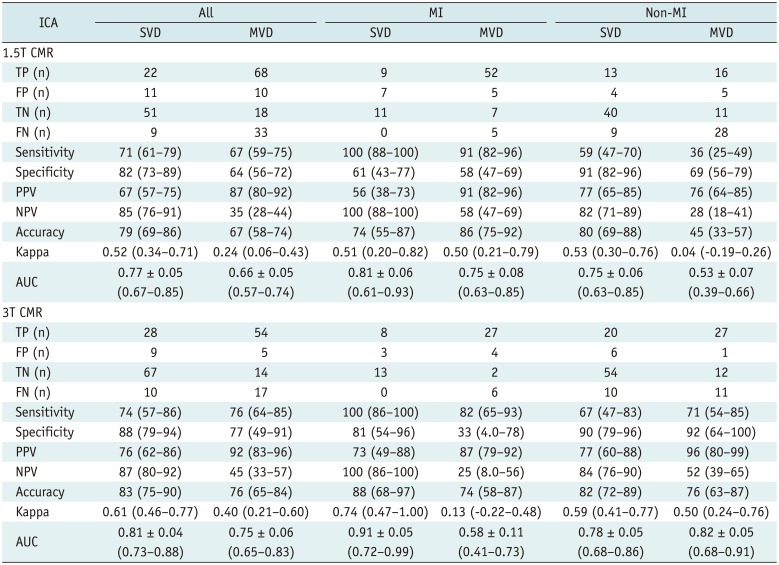
Table 2
Baseline Characteristics of Study Patients
CAD Characteristics
Diagnostic Performance of CMR Perfusion Imaging on Per-Patient and Per-Vascular Territory Bases
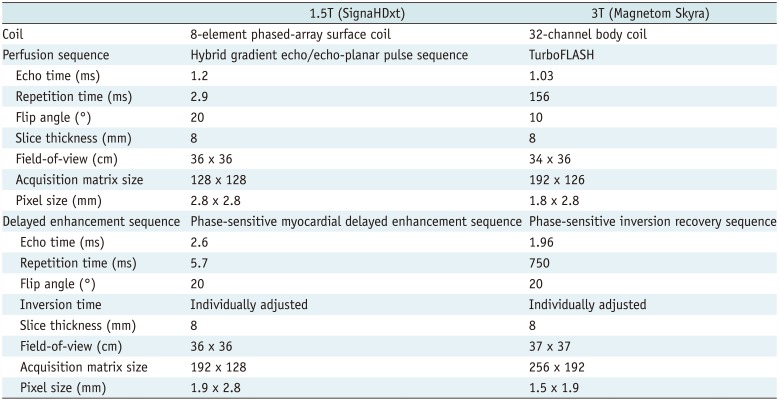
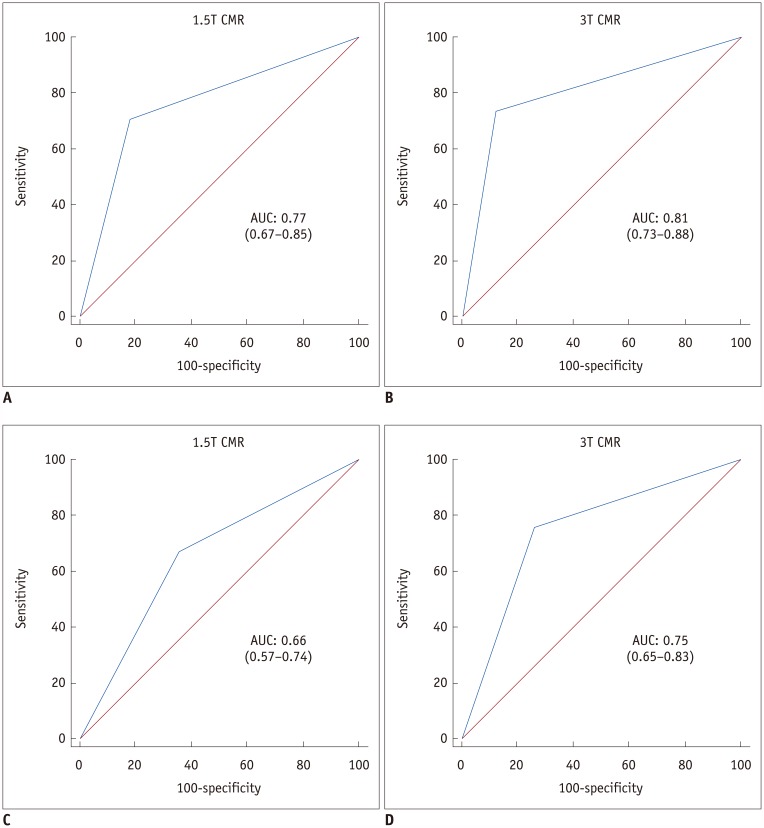
 | Fig. 1AUC for 1.5T and 3T CMR perfusion.
A-D. Patient-based diagnostic performance of 1.5T (A, C) and 3T (B, D) CMR perfusion. E-H. Vessel-based diagnostic performance of 1.5T (E, G) and 3T (F, H) CMR perfusion. AUC of 3T CMR perfusion (H) is significantly greater than AUC of 1.5T CMR perfusion (G) (0.79 vs. 0.67, p = 0.006) on per vessel territory in patients without old MI. AUC = area under receiver operating characteristic curve, CMR = cardiovascular magnetic resonance, MI = myocardial infarction
|
Table 4
Patient- and Vessel-Based Diagnostic Performance of 1.5T and 3T CMR Perfusion Imaging for Detecting Significant Coronary Stenoses Compared with ICA
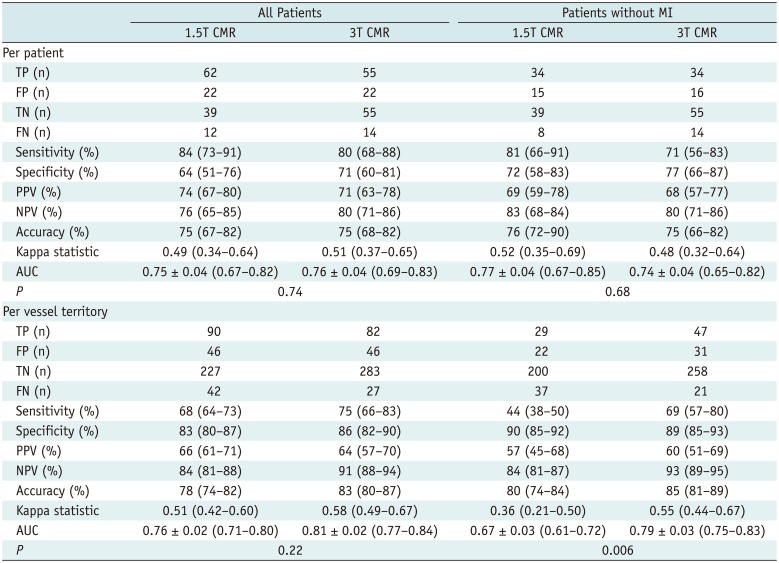
Values for sensitivity, specificity, PPV, NPV, accuracy, kappa statistic, and AUC presented with 95% CIs. AUC expressed as mean ± standard error. AUC = area under receiver operating characteristic curve, CIs = confidence intervals, FN = false negative, FP = false positive, NPV = negative predictive value, PPV = positive predictive value, TN = true negative, TP = true positive
Subgroup Analysis of Vessel-Based Diagnostic Performance of CMR Perfusion Imaging
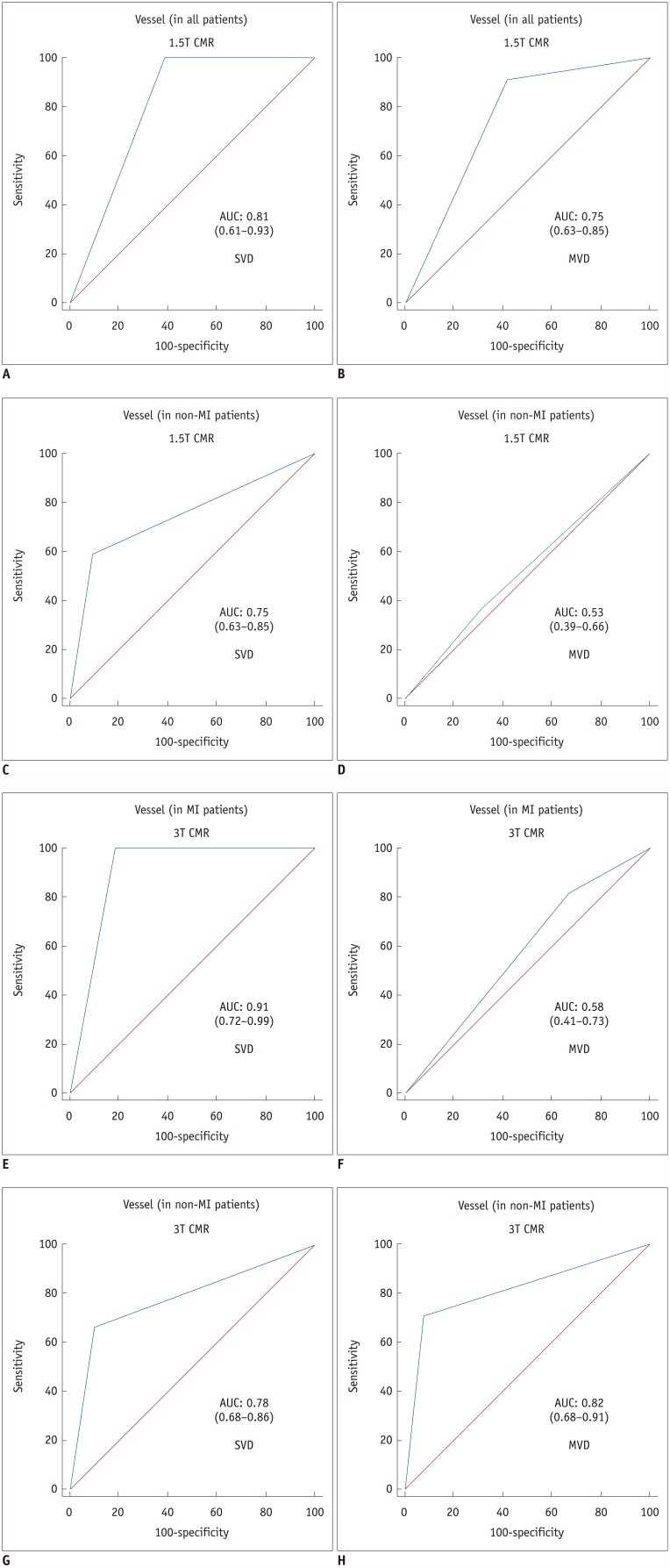
 | Fig. 2AUC for 1.5T and 3T CMR perfusion according to CAD extent.AUC values of both 1.5T (A, C) and 3T (B, D) CMR perfusion imaging for detecting significant CAD are greater in patients with SVD (A, B) than in those with MVD (C, D). CAD = coronary artery disease, MVD = multi-vessel disease, SVD = single-vessel disease
|
 | Fig. 3AUC for 1.5T and 3T CMR perfusion according to combined CAD extent and presence or absence of old MI.1.5T CMR perfusion (C, D) had significantly greater AUC values in SVD (C) than in MVD (D) in patients without old MI (p = 0.01) and 3T CMR had significantly larger AUC values in SVD (E) than in MVD (F) in patients with old MI (p = 0.007). AUC values for 3T CMR were greater than those for 1.5T CMR, except in patients with old MI and MVD (p = 0.20) (B, F), but were only significantly greater in patients without old MI and with MVD (p = 0.001) (D, H).
|
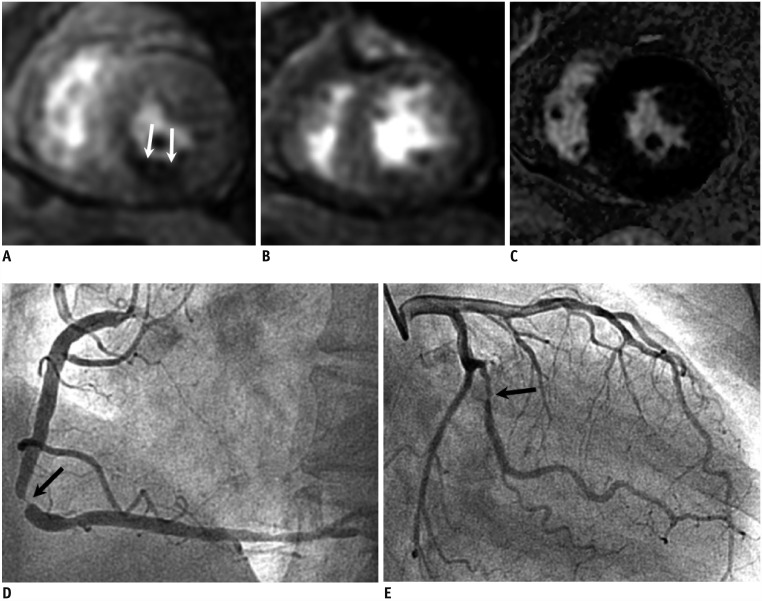 | Fig. 41.5T CMR perfusion with false negative result in MVD without MI.67-year-old female with chest pain; 1.5T CMR stress perfusion (A), rest perfusion (B), and delayed enhancement (C) images show reversible subendocardial perfusion defect at mid-inferior left ventricular wall (arrows). ICA shows severe stenosis at middle segment of right coronary artery (arrow) (D). There was also significant stenosis at large obtuse marginal branch (arrow) (E), but it was not associated with defects in CMR perfusion images. ICA = invasive coronary angiography
|
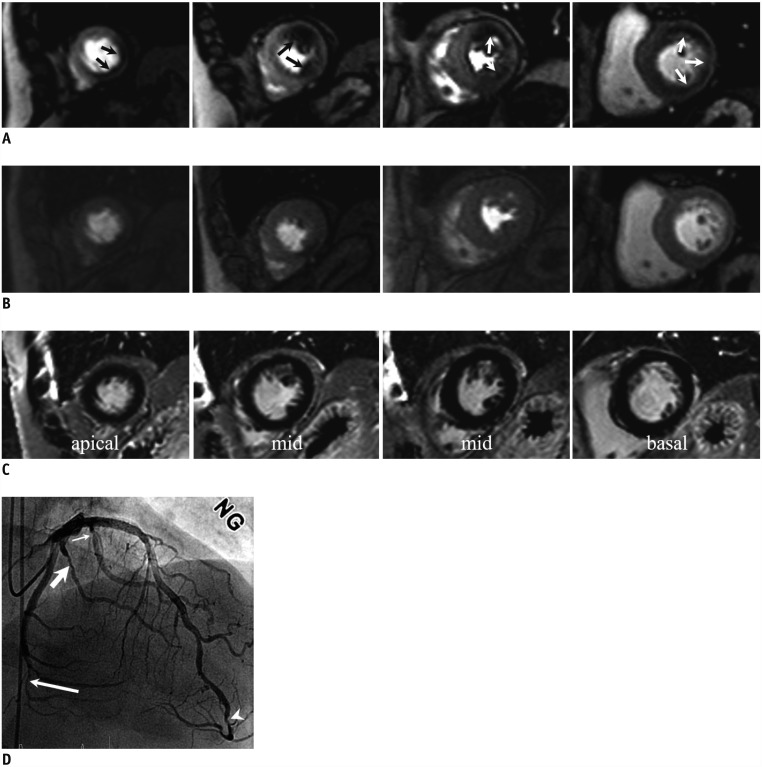 | Fig. 53T CMR perfusion with true positive result in MVD without MI.76-year-old male patient with hypertension and diabetes mellitus who had had 2 previous percutaneous coronary interventions; he had resting pain at epigastric area 2 or 3 times a month.
3T CMR stress perfusion (A), rest perfusion (B), and delayed (C) images show reversible perfusion defects at apical to mid-septal, inferior, and lateral and basal anterior, inferolateral, and inferior left ventricular wall (arrows) (A), corresponding to 3 vessel territories. ICA (D) shows multiple significant stenoses at distal LAD (arrowhead) and first (thin arrow), second (thick arrow), and fifth (long arrow) obtuse marginal branches, consistent with 2-vessel disease. However, given left coronary hyperdominance, 3T CMR and ICA coincide. LAD = left anterior descending coronary artery
|
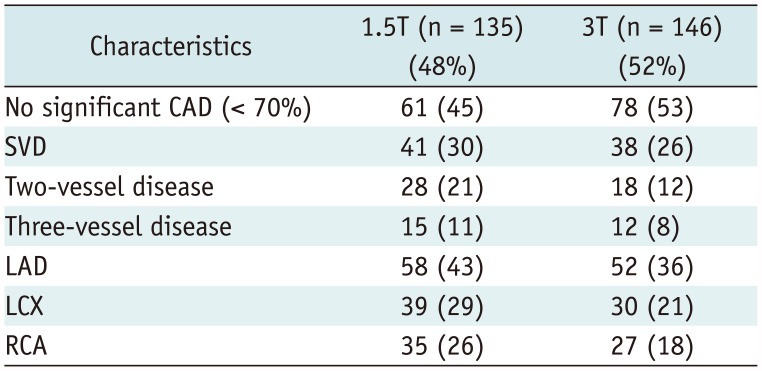
Table 5
Vessel-Based Diagnostic Performance of 1.5T and 3T CMR Perfusion for Detecting Significant Coronary Stenoses Compared with ICA according to CAD Extent and Presence or Absence of old MI




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download