3. Tiong V, Rozita AM, Taib NA, Yip CH, Ng CH. Incidence of chemotherapy-induced ovarian failure in premenopausal women undergoing chemotherapy for breast cancer. World J Surg. 2014; 38:2288–2296. PMID:
24700093.

4. Howell S, Shalet S. Gonadal damage from chemotherapy and radiotherapy. Endocrinol Metab Clin North Am. 1998; 27:927–943. PMID:
9922915.

5. Critchley HO, Wallace WH. Impact of cancer treatment on uterine function. J Natl Cancer Inst Monogr. 2005; 2005:64–68.

6. Rodriguez-Wallberg KA, Oktay K. Options on fertility preservation in female cancer patients. Cancer Treat Rev. 2012; 38:354–361. PMID:
22078869.

7. Monte LM, Ellis RR. Fertility of women in the United States: 2012. Washington, D.C.: United States Census Bureau;2014. p. 20–575.
8. Rosen A, Rodriguez-Wallberg KA, Rosenzweig L. Psychosocial distress in young cancer survivors. Semin Oncol Nurs. 2009; 25:268–277. PMID:
19879433.

9. Zeltzer LK. Cancer in adolescents and young adults psychosocial aspects. Long-term survivors. Cancer. 1993; 71:3463–3468. PMID:
8490896.

10. Han HS, Ro J, Lee KS, Nam BH, Seo JA, Lee DH, et al. Analysis of chemotherapy-induced amenorrhea rates by three different anthracycline and taxane containing regimens for early breast cancer. Breast Cancer Res Treat. 2009; 115:335–342. PMID:
18506620.

11. Lee S, Song JY, Ku SY, Kim SH, Kim T. Fertility preservation in women with cancer. Clin Exp Reprod Med. 2012; 39:46–51. PMID:
22816069.

12. Meirow D. Reproduction post-chemotherapy in young cancer patients. Mol Cell Endocrinol. 2000; 169:123–131. PMID:
11155944.

13. Wallace WH, Anderson RA, Irvine DS. Fertility preservation for young patients with cancer: who is at risk and what can be offered? Lancet Oncol. 2005; 6:209–218. PMID:
15811616.

14. Meirow D, Nugent D. The effects of radiotherapy and chemotherapy on female reproduction. Hum Reprod Update. 2001; 7:535–543. PMID:
11727861.

15. Speiser B, Rubin P, Casarett G. Aspermia following lower truncal irradiation in Hodgkin’s disease. Cancer. 1973; 32:692–698. PMID:
4726968.

16. Sklar C. Maintenance of ovarian function and risk of premature menopause related to cancer treatment. J Natl Cancer Inst Monogr. 2005; 2005:25–27.

17. Wallace WH, Thomson AB, Saran F, Kelsey TW. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int J Radiat Oncol Biol Phys. 2005; 62:738–744. PMID:
15936554.

18. Wo JY, Viswanathan AN. Impact of radiotherapy on fertility, pregnancy, and neonatal outcomes in female cancer patients. Int J Radiat Oncol Biol Phys. 2009; 73:1304–1312. PMID:
19306747.

19. Green DM, Sklar CA, Boice JD Jr, Mulvihill JJ, Whitton JA, Stovall M, et al. Ovarian failure and reproductive outcomes after childhood cancer treatment: results from the Childhood Cancer Survivor Study. J Clin Oncol. 2009; 27:2374–2381. PMID:
19364956.

20. Chemaitilly W, Mertens AC, Mitby P, Whitton J, Stovall M, Yasui Y, et al. Acute ovarian failure in the childhood cancer survivor study. J Clin Endocrinol Metab. 2006; 91:1723–1728. PMID:
16492690.

21. Wallace WH, Thomson AB, Kelsey TW. The radiosensitivity of the human oocyte. Hum Reprod. 2003; 18:117–121. PMID:
12525451.

22. Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006; 24:2917–2931. PMID:
16651642.

23. Forman EJ, Anders CK, Behera MA. Pilot survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. J Reprod Med. 2009; 54:203–207. PMID:
19438160.
24. Armuand GM, Rodriguez-Wallberg KA, Wettergren L, Ahlgren J, Enblad G, Höglund M, et al. Sex differences in fertility-related information received by young adult cancer survivors. J Clin Oncol. 2012; 30:2147–2153. PMID:
22585695.

25. Lee S, Heytens E, Moy F, Ozkavukcu S, Oktay K. Determinants of access to fertility preservation in women with breast cancer. Fertil Steril. 2011; 95:1932–1936. PMID:
21371704.

26. Goodwin T, Elizabeth Oosterhuis B, Kiernan M, Hudson MM, Dahl GV. Attitudes and practices of pediatric oncology providers regarding fertility issues. Pediatr Blood Cancer. 2007; 48:80–85. PMID:
16572406.

27. Lee S, Ozkavukcu S, Heytens E, Moy F, Oktay K. Value of early referral to fertility preservation in young women with breast cancer. J Clin Oncol. 2010; 28:4683–4686. PMID:
20876425.

28. Lee S, Oktay K. Does higher starting dose of FSH stimulation with letrozole improve fertility preservation outcomes in women with breast cancer? Fertil Steril. 2012; 98:961–964.e1. PMID:
22771027.

29. Wang A, Santistevan A, Hunter Cohn K, Copperman A, Nulsen J, Miller BT, et al. Freeze-only versus fresh embryo transfer in a multicenter matched cohort study: contribution of progesterone and maternal age to success rates. Fertil Steril. 2017; 108:254–261.e4. PMID:
28579411.

30. Gosden R. Cryopreservation: a cold look at technology for fertility preservation. Fertil Steril. 2011; 96:264–268. PMID:
21718989.

31. Palermo G, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992; 340:17–18. PMID:
1351601.

32. Katayama KP, Stehlik J, Kuwayama M, Kato O, Stehlik E. High survival rate of vitrified human oocytes results in clinical pregnancy. Fertil Steril. 2003; 80:223–224. PMID:
12849831.

33. Pavone ME, Confino R, Steinberg M. Female fertility preservation: a clinical perspective. Minerva Ginecol. 2016; 68:458–465. PMID:
26847846.
34. Marnitz S, Köhler C, Schneider A, Seiler F, Hinkelbein W. Interindividual variability of lymph drainages in patients with cervical cancer. Implication on irradiation planning. Strahlenther Onkol. 2006; 182:80–85. PMID:
16447014.
35. Martin JR, Kodaman P, Oktay K, Taylor HS. Ovarian cryopreservation with transposition of a contralateral ovary: a combined approach for fertility preservation in women receiving pelvic radiation. Fertil Steril. 2007; 87:189.e5–189.e7.

36. Moore HC, Unger JM, Phillips KA, Boyle F, Hitre E, Porter D, et al. Goserelin for ovarian protection during breast-cancer adjuvant chemotherapy. N Engl J Med. 2015; 372:923–932. PMID:
25738668.

37. Oktay K, Rodriguez-Wallberg K, Munster P. Ovarian protection during adjuvant chemotherapy. N Engl J Med. 2015; 372:2268–2269.

38. Kano M, Sosulski AE, Zhang L, Saatcioglu HD, Wang D, Nagykery N, et al. AMH/MIS as a contraceptive that protects the ovarian reserve during chemotherapy. Proc Natl Acad Sci U S A. 2017; 114:E1688–E1697. PMID:
28137855.

39. Li F, Turan V, Lierman S, Cuvelier C, De Sutter P, Oktay K. Sphingosine-1-phosphate prevents chemotherapy-induced human primordial follicle death. Hum Reprod. 2014; 29:107–113. PMID:
24221908.

40. Plante M, Gregoire J, Renaud MC, Roy M. The vaginal radical trachelectomy: an update of a series of 125 cases and 106 pregnancies. Gynecol Oncol. 2011; 121:290–297. PMID:
21255824.

41. National Comprehensive Cancer Network, Inc.NCCN clinical practice guidelines in oncology (NCCN Guidelines®). Version 3. Ovarian cancer: including fallopian tube cancer and primary peritoneal cancer [Internet]. Fort Washington (PA): National Comprehensive Cancer Network, Inc.;c2017. cited 2017 Aug 30. Available from:
https://www.nccn.org/professionals/physician_gls/pdf/ovarian.pdf.
42. National Comprehensive Cancer Network, Inc.NCCN clinical practice guidelines in oncology (NCCN Guidelines®). Version 1. Adolescent and young adult (AYA) oncology [Internet]. Fort Washington (PA): National Comprehensive Cancer Network, Inc.;c2018. cited 2017 Aug 7. Available from:
https://www.nccn.org/professionals/physician_gls/pdf/aya.pdf.
43. National Comprehensive Cancer Network, Inc.NCCN clinical practice guidelines in oncology (NCCN Guidelines®). Version 3. Uterine neoplasms [Internet]. Fort Washington (PA): National Comprehensive Cancer Network, Inc.;c2017. cited 2017 Jul 18. Available from:
https://www.nccn.org/professionals/physician_gls/pdf/uterine.pdf.
44. Lee S, Kim SK, Hwang KJ, Kim T, Kim SH. Fertility preservation for patients with gynecologic malignancies: the Korean Society for Fertility Preservation clinical guidelines. Clin Exp Reprod Med. 2017; 44:175–180. PMID:
29376013.

45. Seli E, Tangir J. Fertility preservation options for female patients with malignancies. Curr Opin Obstet Gynecol. 2005; 17:299–308. PMID:
15870565.

46. Mazur P. Equilibrium, quasi-equilibrium, and nonequilibrium freezing of mammalian embryos. Cell Biophys. 1990; 17:53–92. PMID:
1704816.

47. Klocke S, Bündgen N, Köster F, Eichenlaub-Ritter U, Griesinger G. Slow-freezing versus vitrification for human ovarian tissue cryopreservation. Arch Gynecol Obstet. 2015; 291:419–426. PMID:
25115279.

48. Gandolfi F, Paffoni A, Papasso Brambilla E, Bonetti S, Brevini TA, Ragni G. Efficiency of equilibrium cooling and vitrification procedures for the cryopreservation of ovarian tissue: comparative analysis between human and animal models. Fertil Steril. 2006; 85(Suppl 1):1150–1156. PMID:
16616087.

49. Vajta G, Nagy ZP. Are programmable freezers still needed in the embryo laboratory? Review on vitrification. Reprod Biomed Online. 2006; 12:779–796. PMID:
16792858.

50. Demeestere I, Simon P, Emiliani S, Delbaere A, Englert Y. Orthotopic and heterotopic ovarian tissue transplantation. Hum Reprod Update. 2009; 15:649–665. PMID:
19474206.

51. Bedaiwy MA, Falcone T. Ovarian tissue banking for cancer patients: reduction of post-transplantation ischaemic injury: intact ovary freezing and transplantation. Hum Reprod. 2004; 19:1242–1244. PMID:
15117897.

52. Martinez-Madrid B, Dolmans MM, Van Langendonckt A, Defrère S, Donnez J. Freeze-thawing intact human ovary with its vascular pedicle with a passive cooling device. Fertil Steril. 2004; 82:1390–1394. PMID:
15533365.

53. Revel A, Elami A, Bor A, Yavin S, Natan Y, Arav A. Whole sheep ovary cryopreservation and transplantation. Fertil Steril. 2004; 82:1714–1715. PMID:
15589891.

54. Migishima F, Suzuki-Migishima R, Song SY, Kuramochi T, Azuma S, Nishijima M, et al. Successful cryopreservation of mouse ovaries by vitrification. Biol Reprod. 2003; 68:881–887. PMID:
12604638.
55. Yin H, Wang X, Kim SS, Chen H, Tan SL, Gosden RG. Transplantation of intact rat gonads using vascular anastomosis: effects of cryopreservation, ischaemia and genotype. Hum Reprod. 2003; 18:1165–1172. PMID:
12773441.

56. Kim SY, Lee JR. Fertility preservation option in young women with ovarian cancer. Future Oncol. 2016; 12:1695–1698. PMID:
27193251.

57. Kim SY, Kim SK, Lee JR, Woodruff TK. Toward precision medicine for preserving fertility in cancer patients: existing and emerging fertility preservation options for women. J Gynecol Oncol. 2016; 27:e22. PMID:
26768785.

58. Xu M, Kreeger PK, Shea LD, Woodruff TK. Tissue-engineered follicles produce live, fertile offspring. Tissue Eng. 2006; 12:2739–2746. PMID:
17518643.

59. Xu M, Barrett SL, West-Farrell E, Kondapalli LA, Kiesewetter SE, Shea LD, et al.
In vitro grown human ovarian follicles from cancer patients support oocyte growth. Hum Reprod. 2009; 24:2531–2540. PMID:
19597190.
60. Oktay K, Karlikaya G. Ovarian function after transplantation of frozen, banked autologous ovarian tissue. N Engl J Med. 2000; 342:1919.

61. Oktay K, Oktem O. Ovarian cryopreservation and transplantation for fertility preservation for medical indications: report of an ongoing experience. Fertil Steril. 2010; 93:762–768. PMID:
19013568.

62. Donnez J, Dolmans MM, Demylle D, Jadoul P, Pirard C, Squifflet J, et al. Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet. 2004; 364:1405–1410. PMID:
15488215.

63. Silber SJ, Lenahan KM, Levine DJ, Pineda JA, Gorman KS, Friez MJ, et al. Ovarian transplantation between monozygotic twins discordant for premature ovarian failure. N Engl J Med. 2005; 353:58–63. PMID:
15941849.

64. Meirow D, Levron J, Eldar-Geva T, Hardan I, Fridman E, Zalel Y, et al. Pregnancy after transplantation of cryopreserved ovarian tissue in a patient with ovarian failure after chemotherapy. N Engl J Med. 2005; 353:318–321. PMID:
15983020.

65. Demeestere I, Simon P, Emiliani S, Delbaere A, Englert Y. Fertility preservation: successful transplantation of cryopreserved ovarian tissue in a young patient previously treated for Hodgkin’s disease. Oncologist. 2007; 12:1437–1442. PMID:
18165621.

66. Andersen CY, Rosendahl M, Byskov AG, Loft A, Ottosen C, Dueholm M, et al. Two successful pregnancies following autotransplantation of frozen/thawed ovarian tissue. Hum Reprod. 2008; 23:2266–2272. PMID:
18603535.

67. Oktay K, Taylan E, Sugishita Y, Goldberg GM. Robot-assisted laparoscopic transplantation of frozen-thawed ovarian tissue. J Minim Invasive Gynecol. 2017; 24:897–898. PMID:
28274872.

68. Oktay K, Newton H, Mullan J, Gosden RG. Development of human primordial follicles to antral stages in SCID/hpg mice stimulated with follicle stimulating hormone. Hum Reprod. 1998; 13:1133–1138. PMID:
9647533.

69. Oktay K, Newton H, Gosden RG. Transplantation of cryopreserved human ovarian tissue results in follicle growth initiation in SCID mice. Fertil Steril. 2000; 73:599–603. PMID:
10689020.

70. Gook DA, McCully BA, Edgar DH, McBain JC. Development of antral follicles in human cryopreserved ovarian tissue following xenografting. Hum Reprod. 2001; 16:417–422. PMID:
11228205.

71. Luyckx V, Scalercio S, Jadoul P, Amorim CA, Soares M, Donnez J, et al. Evaluation of cryopreserved ovarian tissue from prepubertal patients after long-term xenografting and exogenous stimulation. Fertil Steril. 2013; 100:1350–1357.e3. PMID:
23953325.

72. Lucifero D, Mertineit C, Clarke HJ, Bestor TH, Trasler JM. Methylation dynamics of imprinted genes in mouse germ cells. Genomics. 2002; 79:530–538. PMID:
11944985.

73. Kim SS, Kang HG, Kim NH, Lee HC, Lee HH. Assessment of the integrity of human oocytes retrieved from cryopreserved ovarian tissue after xenotransplantation. Hum Reprod. 2005; 20:2502–2508. PMID:
15946997.
74. Donnez J, Dolmans MM, Pellicer A, Diaz-Garcia C, Sanchez Serrano M, Schmidt KT, et al. Restoration of ovarian activity and pregnancy after transplantation of cryopreserved ovarian tissue: a review of 60 cases of reimplantation. Fertil Steril. 2013; 99:1503–1513. PMID:
23635349.

75. Silber SJ, DeRosa M, Pineda J, Lenahan K, Grenia D, Gorman K, et al. A series of monozygotic twins discordant for ovarian failure: ovary transplantation (cortical versus microvascular) and cryopreservation. Hum Reprod. 2008; 23:1531–1537. PMID:
18285322.

76. Silber SJ, Gosden RG. Ovarian transplantation in a series of monozygotic twins discordant for ovarian failure. N Engl J Med. 2007; 356:1382–1384. PMID:
17392316.

77. Silber SJ, Grudzinskas G, Gosden RG. Successful pregnancy after microsurgical transplantation of an intact ovary. N Engl J Med. 2008; 359:2617–2618. PMID:
19073987.

78. Donnez J, Squifflet J, Pirard C, Jadoul P, Dolmans MM. Restoration of ovarian function after allografting of ovarian cortex between genetically non-identical sisters. Hum Reprod. 2010; 25:2489–2495. PMID:
20663793.

79. Kim SS. Assessment of long term endocrine function after transplantation of frozen-thawed human ovarian tissue to the heterotopic site: 10 year longitudinal follow-up study. J Assist Reprod Genet. 2012; 29:489–493. PMID:
22492223.
80. Jensen AK, Kristensen SG, Macklon KT, Jeppesen JV, Fedder J, Ernst E, et al. Outcomes of transplantations of cryopreserved ovarian tissue to 41 women in Denmark. Hum Reprod. 2015; 30:2838–2845. PMID:
26443605.

81. Kim SS, Lee WS, Chung MK, Lee HC, Lee HH, Hill D. Long-term ovarian function and fertility after heterotopic autotransplantation of cryobanked human ovarian tissue: 8-year experience in cancer patients. Fertil Steril. 2009; 91:2349–2354. PMID:
18675964.

82. Wallace WH, Kelsey TW, Anderson RA. Ovarian cryopreservation: experimental or established and a cure for the menopause? Reprod Biomed Online. 2012; 25:93–95. PMID:
22858254.

83. Van Eyck AS, Jordan BF, Gallez B, Heilier JF, Van Langendonckt A, Donnez J. Electron paramagnetic resonance as a tool to evaluate human ovarian tissue reoxygenation after xenografting. Fertil Steril. 2009; 92:374–381. PMID:
18692811.

84. Van Eyck AS, Bouzin C, Feron O, Romeu L, Van Langendonckt A, Donnez J, et al. Both host and graft vessels contribute to revascularization of xenografted human ovarian tissue in a murine model. Fertil Steril. 2010; 93:1676–1685. PMID:
19539913.

85. Meirow D. Fertility preservation in cancer patients using stored ovarian tissue: clinical aspects. Curr Opin Endocrinol Diabetes Obes. 2008; 15:536–547. PMID:
18971683.

86. Baird DT, Webb R, Campbell BK, Harkness LM, Gosden RG. Long-term ovarian function in sheep after ovariectomy and transplantation of autografts stored at -196 C. Endocrinology. 1999; 140:462–471. PMID:
9886858.
87. Faddy MJ, Gosden RG. Ovary and ovulation: a model conforming the decline in follicle numbers to the age of menopause in women. Hum Reprod. 1996; 11:1484–1486. PMID:
8671489.

88. Wallace WH, Kelsey TW. Human ovarian reserve from conception to the menopause. PLoS One. 2010; 5:e8772. PMID:
20111701.

89. des Rieux A, Ucakar B, Mupendwa BP, Colau D, Feron O, Carmeliet P, et al. 3D systems delivering VEGF to promote angiogenesis for tissue engineering. J Control Release. 2011; 150:272–278. PMID:
21130820.

90. Dath C, Dethy A, Van Langendonckt A, Van Eyck AS, Amorim CA, Luyckx V, et al. Endothelial cells are essential for ovarian stromal tissue restructuring after xenotransplantation of isolated ovarian stromal cells. Hum Reprod. 2011; 26:1431–1439. PMID:
21421662.

91. Friedman O, Orvieto R, Fisch B, Felz C, Freud E, Ben-Haroush A, et al. Possible improvements in human ovarian grafting by various host and graft treatments. Hum Reprod. 2012; 27:474–482. PMID:
22114111.

92. Kristensen SG, Giorgione V, Humaidan P, Alsbjerg B, Bjørn AB, Ernst E, et al. Fertility preservation and refreezing of transplanted ovarian tissue-a potential new way of managing patients with low risk of malignant cell recurrence. Fertil Steril. 2017; 107:1206–1213. PMID:
28433369.

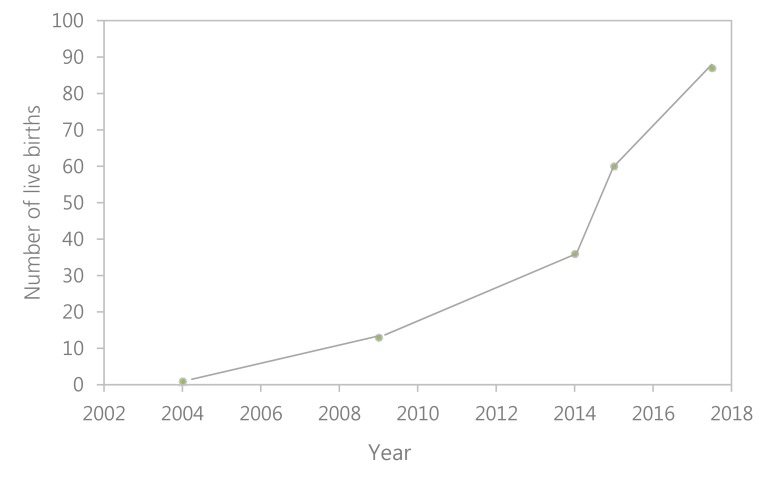
93. Jensen AK, Macklon KT, Fedder J, Ernst E, Humaidan P, Andersen CY. 86 successful births and 9 ongoing pregnancies worldwide in women transplanted with frozen-thawed ovarian tissue: focus on birth and perinatal outcome in 40 of these children. J Assist Reprod Genet. 2017; 34:325–336. PMID:
28028773.

94. Donnez J, Dolmans MM, Diaz C, Pellicer A. Ovarian cortex transplantation: time to move on from experimental studies to open clinical application. Fertil Steril. 2015; 104:1097–1098. PMID:
26342246.
95. Anderson CY. Success and challenges in fertility preservation after ovarian tissue grafting. Lancet. 2015; 385:1947–1948.
96. Stoop D, Cobo A, Silber S, Diaz-Garcia C, Ernst E, Macklon KT, et al. Fertility preservation for age-related fertility decline. Lancet. 2014; 384:1311–1319. PMID:
25283572.

97. Anderson RA, Mitchell RT, Kelsey TW, Spears N, Telfer EE, Wallace WH. Cancer treatment and gonadal function: experimental and established strategies for fertility preservation in children and young adults. Lancet Diabetes Endocrinol. 2015; 3:556–567. PMID:
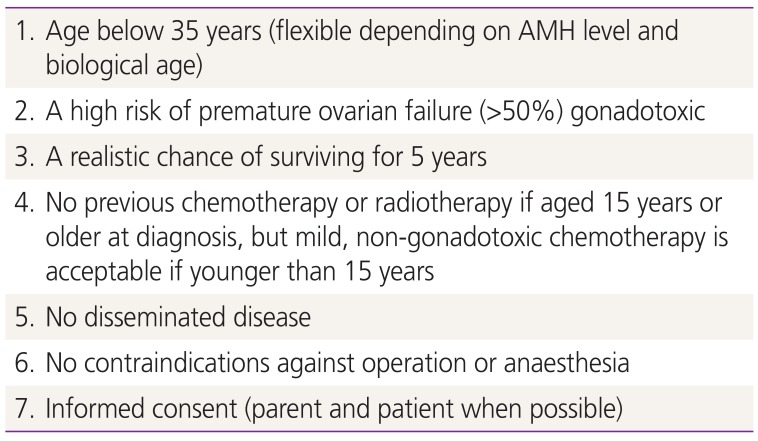
25873571.

98. Wallace WH, Smith AG, Kelsey TW, Edgar AE, Anderson RA. Fertility preservation for girls and young women with cancer: population-based validation of criteria for ovarian tissue cryopreservation. Lancet Oncol. 2014; 15:1129–1136. PMID:
25130994.

99. Donfack NJ, Alves KA, Araújo VR, Cordova A, Figueiredo JR, Smitz J, et al. Expectations and limitations of ovarian tissue transplantation. Zygote. 2017; 25:391–403. PMID:
28766468.

100. Oktay K, Economos K, Kan M, Rucinski J, Veeck L, Rosenwaks Z. Endocrine function and oocyte retrieval after autologous transplantation of ovarian cortical strips to the forearm. JAMA. 2001; 286:1490–1493. PMID:
11572742.

101. Rodriguez-Wallberg KA, Oktay K. Recent advances in oocyte and ovarian tissue cryopreservation and transplantation. Best Pract Res Clin Obstet Gynaecol. 2012; 26:391–405. PMID:
22301053.

102. Stern CJ, Gook D, Hale LG, Agresta F, Oldham J, Rozen G, et al. Delivery of twins following heterotopic grafting of frozen-thawed ovarian tissue. Hum Reprod. 2014; 29:1828–1829.

103. Donnez J, Jadoul P, Squifflet J, Van Langendonckt A, Donnez O, Van Eyck AS, et al. Ovarian tissue cryopreservation and transplantation in cancer patients. Best Pract Res Clin Obstet Gynaecol. 2010; 24:87–100. PMID:
19850531.

104. Lee S, Song JY, Kim T, Kim SH. Ovarian tissue cryopreservation and transplantation in a young patient with cervical cancer: the first successful case in Korea. Eur J Gynaecol Oncol. [Epub].
105. Farber LA, Ames JW, Rush S, Gal D. Laparoscopic ovarian transposition to preserve ovarian function before pelvic radiation and chemotherapy in a young patient with rectal cancer. MedGenMed. 2005; 7:66.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download