Abstract
Kidney diseases including acute kidney injury and chronic kidney disease are among the largest health issues worldwide. Dialysis and kidney transplantation can replace a significant portion of renal function, however these treatments still have limitations. To overcome these shortcomings, a variety of innovative efforts have been introduced, including cell-based therapies. During the past decades, advances have been made in the stem cell and developmental biology, and tissue engineering. As part of such efforts, studies on renal cell therapy and artificial kidney developments have been conducted, and multiple therapeutic interventions have shown promise in the pre-clinical and clinical settings. More recently, therapeutic cell-secreting secretomes have emerged as a potential alternative to cell-based approaches. This approach involves the use of renotropic factors, such as growth factors and cytokines, that are produced by cells and these factors have shown effectiveness in facilitating kidney function recovery. This review focuses on the renotropic functions of bioactive compounds that provide protective and regenerative effects for kidney tissue repair, based on the available data in the literature.
Renal failure is a major health issues worldwide. Acute kidney injury (AKI) results in an abrupt loss of renal function with a corresponding spike in serum creatinine concentration and decrease in urine output. Although AKI is a reversible condition, it can progress to chronic kidney disease (CKD), which is characterized by a reduced glomerular filtration rate. End-stage renal disease (ESRD) is devastating condition, which requires either renal transplantation or dialysis. Although kidney dialysis replaces the renal filtration function by removing toxic substances from the blood and maintains survival of ESRD patients, it does not restore other kidney functions, such as erythropoietin production and vitamin D activation. Therefore, kidney transplantation is the only option to replace renal function in patients with ESRD. Unfortunately, donor shortage, surgical morbidity and complications associated with the life-long usage of immune suppressants remain a continued problem.
To address these unmet medical needs, several regenerative medicine approaches have been proposed as possible solutions. Regenerative medicine is a multidisciplinary field that combines various areas of science, including stem cell biology, developmental biology, material sciences, and tissue engineering. Various technologies developed in regenerative medicine have been applied for the restoration of kidney functions. Major research efforts in the regenerative medicine for kidney diseases include 1) identification of renal stem/progenitor cells in embryonic and adult kidneys, 2) cell therapies with hematopoietic, mesenchymal or fetal stem cells, and 3) reconstruction of artificial kidneys or renal components by using primary renal cells, embryonic stem cells, or induced pluripotent stem cells (iPS).1 While many therapeutic interventions appear to be effective in pre-clinical applications using animal models and a few clinical applications of AKI or CKD, challenges still exist in translating these promising outcomes in patients with kidney diseases. For example, despite the recent advances in cell-based therapies for the treatment of kidney diseases, safety remains a continued concern, as direct injection of the therapeutic cells can cause immune rejection, pulmonary embolism, and even teratoma formation in case of pluripotent cells.23
It has been demonstrated that cells produce trophic factors that control regulation and function. These cellular products or secretomes present in the culture medium have been shown to be as effective as cellular therapies.24 As such, the use of cellular secretomes for therapy is an appealing alternative to cell-based options.24 Secretomes have been used as a form of conditioned medium (CM), where high levels of growth factors and tissue repairing chemokines from therapeutic cells are released into culture medium.4 Several studies demonstrated favorable outcomes of CM therapy in kidney diseases using various types of cells including mesenchymal stem cells (MSC) and iPS.4 While the use of secretomes demonstrated a promising alternative to the cell-based therapy, many challenges need to be addressed before applying in the clinical setting. The most critical issue involving the use of secretomes is attributed to the unidentified characteristic of the secreting factors.2 Further studies are needed to better characterize and define secretomes, which allows for improved control and regulation for clinical translation.2
Based on the pre-clinical therapeutic outcomes as described above,4 the CM secreted from the therapeutic cells is presumed to contain renotropic factors responsible for the kidney repair. The renotropic factors include various bioactive molecules such as cytokines and growth factors that promote normal tubular cell differentiation, thus expected to replace lost and damaged tubular epithelial cells and function.156 This review covers the renotropic functions of bioactive compounds that have potential to impact renal regeneration and protection based on the available data in the literature.
Hepatocyte growth factor (HGF) is a ligand for the c-Met receptor tyrosine kinase, which is known to have anti-apoptotic, mitogenic, motogenic, and morphogenic effects on renal tubular cells, as well as angiogenic and angioprotective effects on endothelial cells.7 Sources of renal HGF are stromal cells such as mesangial cells, endothelial cells, and macrophages. In response to AKI, HGF secretion increases in distant organs such as lung and spleen as well as the injured kidney, and increase in HGF plays a role in renal regeneration. HGF is a pleiotropic factor that plays an imperative role in tubular repair and regeneration after AKI. It is also known that HGF is also a renoprotective factor that exhibits a potent antifibrotic ability.8 As chronic renal failure progresses, the expression of HGF decreases, but the expression of transforming growth factor-β (TGF-β) reciprocally increases.7 As is well known, TGF-β is a key factor in tissue fibrosis. Thus, decrease in HGF is associated with the aggravation of renal fibrosis and chronic renal failure.
HGF's morphogenic and motogenic effects were first described in the Madin-Darby canine kidney cell line,9 and were also shown in other epithelial cells such as a visceral glomerular cell line, proximal tubular cell lines, and a medullary collecting duct cell line.101112 A unilateral nephrectomy model has been used to study the renotropic systems in compensatory renal regeneration. HGF mRNA and protein increase were observed in the remaining kidney after unilateral nephrectomy, and this type of response was also shown in various models of acute renal injury caused by various nephrotoxins.131415 Animal model experiments involving the treatment of supplements of exogenous HGF have shown preventive and therapeutic effects on injured kidneys. Kawaida, et al.16 demonstrated that intravenous injection of recombinant human HGF into mice prevented the deterioration of renal function caused by administration of cisplatin or HgCl2. In addition, exogenous HGF promoted DNA synthesis of renal tubular cells following kidney injuries caused by HgCl2 administration and unilateral nephrectomy, and induced regeneration of the normal renal tissue structure in vivo. These results suggest that HGF prevents epithelial cell death, and promotes regeneration and remodeling of renal tissue against injury or fibrosis. Thus, HGF administration may be one treatment strategy to treat renal diseases.
Insulin-like growth factor-1 (IGF-1) is a single-chain proinsulin-like polypeptide, which consists of 70 amino acids. IGF-1 is a growth hormone (GH)-dependent growth factor, and it is thought that the growth-promoting and anabolic actions of GH are mediated by IGF-1.17 The circulating level of IGF-1 is controlled by GH. The collecting duct is a major source of IGF-1 production in the adult kidney, and glomerular mesangial cells in culture also produce IGF-1. Receptors for IGF-1 are present in the glomeruli and on the basolateral membrane of the renal proximal tubular cell.18 The GH/IGF-1 system is essential for normal kidney development and function. During embryogenesis, IGF-1 and -2 play important roles in normal metanephric development.19 During compensatory renal growth after unilateral nephrectomy, IGF-1 mRNA and protein expression was observed in the remaining kidney.20
IGF-1 is also involved in the repair process following AKI. In an animal model, IGF-1 expression is increased in regenerating proximal tubule cells after acute injury, and IGF-1 treatment accelerates recovery.21 Ding, et al.22 demonstrated that IGF-1 treatment reduces protein catabolism and nitrogen excretion in rats with AKI as compared to rats not receiving IGF-1. Moreover, protein synthesis was increased and protein degradation was decreased in excised epitrochlearis muscle from IGF-1-treated as compared to vehicle-treated rats. Miller, et al.23 also demonstrated a similar acceleration of recovery from ischemic AKI in rats receiving recombinant human IGF-1, and this was associated with increased rates of bromodeoxyuridine incorporation into proximal tubules. The beneficial effect of IGF-1 on post-ischemic renal injury could be explained by enhancement of glomerular filtration, renotropic property on renal tubules, and generalized anabolic action.18 However, clinical trials using IGF-1 in patients with AKI did not significantly improve kidney function or overall outcomes. Nevertheless, Bach, et al.21 suggested that IGF-1 may potentially enhance stem cell-mediated repair of kidney injury.
Dysregulation of the IGF system has been implicated in various kidney diseases such as diabetic nephropathy, polycystic kidneys, proteinuric CKD, etc.21 There is growing interest in stem cell therapy for kidney diseases. Some studies suggest that administered stem cells do not integrate into the kidney parenchyma, but likely act as a paracrine source of renotropic factors that ameliorate damage.21 In one study, MSC were shown to provide a protective effect on proximal tubular cell proliferation. This effect was mediated by IGF-1.24 A limitation of systemic infusion of stem cells is their inability to home to injured tissues. Xinaris, et al.25 showed that preconditioning of MSC with IGF-1 before administration improved cell migration and restored normal renal function following AKI. Thus, it is suggested that IGFs may have a potential role in facilitating stem cell repair of kidney injury. However, further studies are necessary to determine the exact role of IGF-based therapies in kidney disease.
Epidermal growth factor (EGF) is a 53-amino-acid peptide, and was first purified from human urine. EGF belongs to an extensive class of molecules, referred to as growth factors, that mediates cell growth and differentiation, and also may stimulate acute cell responses.26 Their effects are mediated via autocrine, paracrine, or endocrine mechanisms. The distal tubule and medullary thick ascending limb of Henle's loop are the predominant sites of EGF production within the adult kidney. Glomeruli, proximal tubules, medullary interstitial cells, and collecting ducts all have EGF receptors. These receptors are present in the basolateral membranes of the tubular epithelial cells.18
Although the exact role of EGF in the kidney is unclear, its mitogenic effect on tubular cells has been suggested. EGF has been shown to be a mitogen for rabbit kidney cortical collecting tubules, cortical thick ascending limbs of Henle, and proximal tubule cells.26 The developing rat kidney produces TGF-β, which is a member of the EGF family of growth factors that acts through the EGF receptor. The growth and development of the metanephros in vitro is dependent on TGF-β.1827 The possible involvement of EGF in compensatory renal hypertrophy has been also studied by immunoassay and in situ hybridization.26 It has also been suggested that EGF may be important in maintaining the integrity of the epithelial surfaces of the urinary tract.28
Humes, et al.29 investigated whether exogenous EGF enhances the regenerative repair process to accelerate recovery of renal function after ischemic renal injury. They showed that exogenous EGF administration produced increases in renal thymidine incorporation compared with nontreated animals after ischemic injury, and this accelerated DNA replicative process was associated with a return to near normal serum creatinine levels in EGF-treated animals several days earlier than that observed in nontreated animals. Miller, et al.23 showed that EGF reduces mortality in rats with ischemic renal injury, in addition to accelerating the restoration of normal renal function and improving histology. Other studies also demonstrated that EGF accelerates renal repair in a model of gentamicin or HgCl2 nephrotoxicity.3031 These results suggest that exogenous EGF accelerates the repair process of the kidney after a severe toxic insult.
Heparin-binding EGF-like growth factor (HB-EGF) is a 20–22-kD glycoprotein originally purified from conditioned media of a macrophage-like cell line, U937, and a member of the EGF superfamily of growth factors that signal through EGF-receptor tyrosine phosphorylation.32 HB-EGF is expressed in macrophages, T lymphocytes, vascular smooth muscle cells, endothelial cells, keratinocytes, and intestinal epithelial cells.32 Homma, et al.33 reported that HB-EGF mRNA could be induced by acute renal injury in rat kidneys, and recombinant HB-EGF has a mitogenic impact on renal epithelial cells. Sakai, et al.32 suggested that HB-EGF is mainly produced in the distal tubules in response to acute injury and that endogenous HB-EGF may be an important growth factor involved in the repair, proliferation, and regeneration of renal epithelial cells in the early stages of recovery. Another study showed that HB-EGF is an autocrine/paracrine factor that mediates the proliferation of renal proximal tubular cells.34
Playing a pivotal role in angiogenesis, vascular endothelial growth factor (VEGF) promotes vascular proliferation and endothelial cell repair. Its role in vascular proliferation is essential for not only developmental phases but also the recovery phase after an ischemic insult. VEGF has been shown to be strongly expressed in proximal tubular epithelium and podocytes in both mouse and human kidneys.35 Basile, et al.36 demonstrated that VEGF mRNA expression was repressed by greater than 50% of control values up to 3 days postischemia, while VEGF protein was repressed for up to 7 days postischemia in an ischemic-reperfusion injury rat model. The loss of endogenous VEGF during a potentially critical window of the early recovery response suggested VEGF therapy could be a feasible renoprotective tool for ischemic renal injury. Leonard, et al.37 evaluated whether recombinant VEGF administration could attenuate the progression of CKD in an ischemic-reperfusion injury rat model. When VEGF was given during the initial 2 weeks post injury, interstitial scarring and albuminuria were significantly eliminated. However, this effect was not observed when VEGF administration was delayed until day 21. Chade and Kelsen38 published some experimental results using a renal artery stenosis pig model, and suggested that damage and early loss of renal microvascular architecture is an important determinant of the renal injury progression in renal artery stenosis and often initiates irreversible damage. In addition, intrarenal administration of VEGF preserved renal microvascular architecture and function of the stenotic kidney, and it preserved renal hemodynamics and function and decreased renal fibrosis. This finding underlines the importance of renal microvascular integrity for renal function.39 A recent study showed VEGF added to amniotic fluid stem cells induced a significantly higher nephroprotection than amniotic fluid stem cells alone in rats with renal ischemia-reperfusion injury.40
TGF-β superfamily includes four different isoforms (TGF-β1 to TGF-β4) which share many structural and functional aspects. TGF-β is known to activate different downstream substrates and regulatory proteins, induce transcription of various target genes that function in the differentiation, chemotaxis, proliferation, and activate many immune cells.41 Among the various biologic effects of TGF-β1, the most prominent feature is the regulation of extracellular matrix component synthesis by stimulation of extracellular matrix production, inhibition of enzymes that degrade matrix, and increase of the expression and adhesion phenotype of matrix receptors.42 TGF-β1 has been known to increase the synthesis of the components of extracellular matrix such collagen types I, II, III, IV, and V, proteoglycans, laminin, fibronectin, tenascin, and elastin.43
Histologic features of most chronic renal diseases, including diabetic nephropathy, focal segmental glomerulosclerosis, obstructive uropathy, and IgA nephritis, share thickened basement membrane, accumulation of mesangial matrix, and glomerular and interstitial sclerosis. It has been well demonstrated that TGF-β1 plays a pivotal role in certain models of renal disease as a mediator of renal fibrosis.43 Border, et al.42 demonstrated that addition of the neutralizing anti-TGF-β in vitro to glomerular cultures suppressed the synthesis of proteoglycans and fibronectin by 80%. Based on these results, they also showed in vivo administration of anti-TGF-β1 at the time of induction of the glomerular disease suppresses the increased production of extracellular matrix and significantly attenuates histological manifestations of the disease.44 Okuda, et al.45 demonstrated that the renal protective effect of a protein restricted diet was through the suppression of TGF-β1 expression in antithymocyte serum-induced nephritis model.
Platelet-derived growth factor (PDGF) was first isolated from platelets, where it is stored in the α-granules and released into the extracellular environment on platelet activation. However, it is also produced by other cell types, including smooth muscle cells, macrophages, and mesangial, epithelial, and endothelial cells of the kidney.43 PDGF is a well-characterized factor that promotes fibrosis in many diseases and organs, including the kidney, and it is one of the most potent mitogens for mesangial cells in culture.4346 Glomerular mesangial cells proliferate in response to glomerular damage, and this response is regarded as a risk factor for the progression of glomerular nephritis to irreversible glomerular scarring and a variety of glomerular diseases. There is also evidence to suggest an involvement of PDGF in the regulation of renal extracellular matrix turnover, the chemoattraction of mesangial cells and/or other cells to sites of injury, the regulation of glomerular hemodynamics, and lipoprotein uptake in the glomerulus.47 Therefore, understanding regulatory mechanisms that control proliferation of mesangial cells is important in developing effective treatments for glomerular disease. Bessho, et al.48 demonstrated that HGF suppressed PDGF-induced proliferation of activated mesangial cells both in vivo and in vitro. Meanwhile, the immunoreactivity of PDGF-B was demonstrated in the immature tubules of the developing human kidney, suggesting that PDGF-B would be involved in the tubulogenesis.49 In addition, Nakagawa, et al.50 reported that the PDGF-B/PDGFRs axis is involved in the proliferation of injured tubular cells and plays an important role in the regeneration of tubular cells from acute ischemic injury.
The TGF-β superfamily includes more than twenty types of bone morphogenetic proteins (BMPs), of which BMP-7 (also called as osteogenic protein-1) is closely involved in kidney development and disease. BMPs are differentially expressed throughout development. BMP-7 is initially expressed in the ureteric bud. In the development period, BMP-7 is also found in the metanephric mesenchyme, early tubules, and in the podocytes of mature glomeruli. In the adult kidney, BMP-7 is expressed in glomerular podocytes, the thick ascending limb, the distal convoluted tubule, and the collecting duct.51 As previously mentioned, TGF-β1 is consistently upregulated in models of experimental and human renal fibrosis. On the contrary, BMP-7 expression was markedly reduced in experimental diseases associated with renal fibrosis. Several studies showed that the expression of BMP-7 mRNA and protein was markedly reduced in the medullar and glomeruli after AKI and unilateral ureteral obstruction.525354 De Petris, et al.55 demonstrated that culture of mouse podocytes under high glucose decreases synaptopodin, podocin and BMP-7 transcription and protein synthesis compared to normal glucose.
An antifibrotic effect of BMP-7 in renal cells has been shown. BMP-7 proved to be a potent inhibitor of TGF-β1 induced epithelial-to-mesenchymal transition of proximal tubular epithelial cells.56 BMP-7 also represses the basal and tumor necrosis factor-α (TNF-α)-stimulated expression of the pro-inflammatory cytokines interleukin (IL)-6 and IL-1β, the chemokines monocyte chemoattractant protein 1 (MCP-1) and IL-8, and the vasoconstrictor endothelin 2 (ET-2) in proximal tubular epithelial cells.57 In cultured mesangial cells, BMP-7 reduces TGF-β-induced extracellular matrix protein accumulation primarily by maintaining levels and activity of matrix metalloprotease-2.58 BMP-7 is a differentiation and survival factor for podocytes, it can also inhibit adverse effect on podocytes caused by high glucose.59
In one study, Vukicevic, et al.60 demonstrated that intravenous BMP-7 treatment reduced severity of renal injury after AKI in rats. BMP-7 treatment inhibited tubular epithelial disruption after unilateral ureteral obstruction, preventing tubular atrophy and diminishing the activation of tubulointerstitial inflammation and fibrosis and preserving renal function.53 Morrissey, et al.61 showed that intraperitoneal BMP-7 treatment is capable of blunting the progression of fibrotic disease and of decreasing interstitial volumes in a rat model of unilateral ureteral obstruction. Of note, a return of renal function is accelerated by BMP-7 treatment. In streptozotocin-induced diabetic rats, both glomerular and tubulointerstitial damage as well as albuminuria were significantly attenuated by BMP-7 therapy in a dose-dependent manner.62 BMP-7 treatment attenuated progression of renal disease even in the genetic mouse models of lupus nephritis and Alport syndrome.56 These results suggest that BMP-7 administration may be a potential treatment to restore or preserve renal function.
A recent discovery in stem cell research has shown multi-lineage plasticity of bone marrow cells and the contribution of hematopoietic stem cell for the regeneration of damaged organs including the kidney. This finding suggests the use of granulocyte-colony stimulating factor (G-CSF) as a therapeutic option to regenerate wounded organs.63 G-CSF mRNA and protein expression was shown in thick ascending limb cells of the kidney after renal AKI in mice, and increased peripheral serum concentration of G-CSF was also noted. This suggests a possible communication from the injured kidney to the bone marrow.64 Several studies have described the effect of exogenous G-CSF on kidney function in an AKI animal model.656667 Some studies reported that G-CSF treatment has a favorable effect on the course of AKI as compared with control group.6566 However, Tögel, et al.67 showed that boosting of peripheral stem cell numbers by G-CSF was associated with increased severity of renal failure and mortality in an AKI model. In addition to these contradictory results, there is still controversy regarding the mechanisms by which G-CSF exerts an alleviative effect on renal injury. The conflicting results of these studies with experimental AKI models suggested complex effects of G-CSF on the kidney. G-CSF can become a two-edged sword after kidney injury; it exerts both mitigating and detrimental effects at the same time.63 A careful observation of renal function is necessary when G-CSF is used in patients with renal injury.
Chemokines are small molecules involved in the regulation of inflammation and cell migration. Chemokines are known to possess the ability to induce directed chemotaxis in nearby responsive cells. C-X-C chemokine receptor type 4 (CXCR4) is a principal receptor for stromal derived factor-1 (SDF-1), and recently the role of CXCR4 has been highlighted in a variety of cancer and acquired immune deficiency syndrome.68 CXCR4 is one of the major receptors that regulate trafficking of hematopoietic and tissue stem cells and progenitor cells. It is also known to guide CXCR4-positive cells during embryogenesis, development and tissue regeneration. Furthermore, CXCR4 is involved in the regulation of angiogenesis through recruitment of endothelial progenitor cells. The recruitment of CXCR4-positive progenitor cells is mediated by hypoxic gradients via hypoxia-inducible factor 1 (HIF-1)-induced expression of SDF-1.69
SDF-1 and CXCR4 expression was observed in the developing kidney. CXCR4 expression was limited to focal expression by extravascular cells positive for the stem cell antigen CD34. SDF-1 expression observed in the ureteric buds, S-shaped bodies, and glomerular mesangium suggests a potential “gradient” of SDF-1 expression.70 Tögel, et al.71 evaluated the expression pattern and functions of the SDF-1/CXCR4 system in normal kidney and in the kidney after ischemia-reperfusion injury. SDF-1 and CXCR4 are expressed in normal kidney mostly by distal tubular cells in the cortex, whereas all kidney regions show robust expression of SDF-1 and CXCR4 after kidney injury induced by ischemia-reperfusion. Stokman, et al.72 demonstrated that renal SDF-1 protein increased significantly in the early phase of ischemia-reperfusion injury, and antisense treatment resulted in a reduction of corticomedullary SDF-1 expression, which was accompanied by severely increased tubular injury and decreased renal function. Ohnishi, et al.73 provided the evidence that incorporation of bone marrow-derived cells in endothelial and smooth muscle cells was evident in an early stage of ischemic kidney injury, and anti-CXCR4 antibody decreased the numbers of infiltrated bone marrow-derived cells. These data suggest that SDF-1/CXCR4 axis may play a protective and reparative role in AKI model. Therefore, renal SDF-1 is one of the important mediators of migration and homing of CXCR4-positive cells targeting the injured kidney.
Interleukins are a group of cytokines that were first seen to be expressed by white blood cells (leukocytes), and they have become well-known regulators of innate and adaptive immunity-related tissue inflammation. IL-22 is exclusively produced by different immune cell subsets, whereas IL-22 receptors are mainly expressed by epithelial cells in various tissues including the kidney. IL-22 primarily targets nonhematopoietic epithelial and stromal cells, where it can promote proliferation and play a role in tissue regeneration. Recently, IL-22 has gained attention due to its unique ability to maintain and restore epithelial integrity.7475
Kulkarni, et al.76 used an in vitro system to screen for the impact of interleukins on post-ischemic epithelial healing, and found that recombinant IL-22 had the strongest proregeneratory effect on tubular epithelial cells. They suggested that necrotic cell-derived Toll-like receptor 4 agonists activate intrarenal mononuclear cells to secrete IL-22, which accelerates tubular regeneration and recovery in AKI. Xu, et al.77 demonstrated that intraperitoneal administration of recombinant IL-22 ameliorates renal ischemia reperfusion injury in mice model, and preserves renal functions by activating signal transducer and activator of transcription 3 (STAT3) and AKT in the proximal tubular epithelial cells. Taken together, these results suggest that IL-22 might also have therapeutic potential for the treatment of acute ischemic kidney injury.
Angiotensin is a peptide hormone that causes vasoconstriction, thus resulting in increased blood pressure. The intrarenal renin-angiotensin system is known to have a major impact on tubular cell proliferation, apoptosis and regeneration following kidney injury.78 Tissue repair involves inflammatory cells and myofibroblasts. Inflammatory cells include members of the monocyte/macrophage lineage and are integral to the initiation of the repair process, while myofibroblasts are phenotypically transformed interstitial fibroblasts that are responsible for collagen turnover and fibrous tissue formation. In the microenvironment, de novo generation of angiotensin II is involved.79 In an autocrine/paracrine manner, this peptide regulates expression of TGF-β1 via angiotensin (AT1) receptor-ligand binding. Angiotensin-converting enzyme (ACE) inhibition or AT1 receptor antagonism prevent many of these molecular and cellular responses that lead to fibrosis.
Drugs that reduce glomerular hypertension and protein trafficking prevents renal function decline and facilitate kidney repair. The objective of the current treatment is inhibition of the renin-angiotensin system by ACE inhibitors (ACEi) and angiotensin II type I receptor blockers (ARBs). Nondiabetic and diabetic nephropathic animal models have clearly shown that treatment with ACEi, ARBs, or their combination prevents progressive renal damage, and also promotes the regression of glomerulosclerosis and vascular lesions.8081
Erythropoietin is a hormone produced largely in the kidney, and it regulates red blood cell production in the hematopoietic system. Erythropoietin is known to be involved in wound healing responses, angiogenesis, and the body's innate response to injury in the brain and heart. In particular, renoprotective effects of erythropoietin during AKI and nephrotoxic agent-induced injury have been also suggested.82 In an ischemic-reperfusion injury animal model, erythropoietin treatment was shown to reduce the extent of renal dysfunction; this renoprotective effect was associated mainly with a reduction in apoptotic cell death.838485 Similar results were also shown in nephrotoxic agent-induced kidney injury model. Bagins, et al.86 demonstrated that erythropoietin significantly enhanced the recovery from AKI induced by cisplatin via stimulation of tubular cell regeneration. Lee, et al.87 showed that erythropoietin effectively attenuated renal interstitial inflammation and fibrosis in chronic cyclosporine nephropathy. Recently, a pilot clinical study suggested a beneficial effect of erythropoietin on the prevention of AKI. Prophylactic administration of erythropoietin prevents AKI and improves postoperative renal function in patients who underwent coronary artery bypass grafting; however, another study failed to reproduce this positive effect.8889
Melatonin is a circadian-regulating hormone mainly secreted by the pineal gland. Recent studies have shown that melatonin has a variety of biological functions, including anti-oxidative stress, anti-inflammatory, anti-apoptosis, and anti-tumor properties.90 It has been reported that intraperitoneal injection of melatonin can reduce kidney damage induced by AKI and unilateral ureteral obstruction mainly through the antioxidant and anti-apoptotic effects.9192
Activin A, a member of the TGF-β superfamily, inhibits branching tubulogenesis of the kidney in organ culture system as well as in an in vitro tubulogenesis model. Follistatin is an antagonist of activin A, also known as activin-binding protein. It can block the effect of activin A on kidney development, plays an important role in branching tubulogenesis, and also promotes tubular regeneration after AKI by blocking the action of endogenous activin A.93 HGF is also known to inhibit the production of activin A, resulting in branching tubulogenesis.93 Fang, et al.94 showed the evidence that activin B is also involved in ischemic reperfusion injury rat model, and proposed that activin B initiates and activin A potentiates renal injury after ischemic reperfusion injury. In a murine study, exogenous administration of follistatin prevented the histologic changes after ischemic kidney injury, reduced apoptosis in tubular cells, and accelerated tubular cell proliferation. Laboratory results on renal function were favorable in follistatin-treated rats.95 In a rat model of unilateral ureteral obstruction, activin A produced by interstitial fibroblasts acts as a potent profibrotic factor during renal fibrosis, administration of recombinant follistatin reduced the fibrotic area in the unilateral ureteral obstruction kidneys.96
Galectins constitute a large family of β-galactoside binding lectins, and galectin-3 is known to promote cell migration by modulating cell-cell adhesion and cell-matrix adhesion which are critical aspects for embryogenesis, inflammation as well as for cancer dissemination.97 It is strongly expressed in the ureteric bud and its derivatives, and its upregulation is critical in controlling the ureteric bud branching, thus it promotes nephrogenesis during development.98 Galectin-3 has also been reported to play a role in ameliorating ischemic and nephrotoxic AKI. There was significant negative correlation between galectin-3 mRNA expression and serum creatinine at 48 hours after an ischemic-reperfusion injury. In later stages of regeneration, galectin-3 expressions were found in macrophages, suggesting that galectin-3 may play an important role in acute tubular injury and the following regeneration stage.99 On the one hand, galectin-3 is associated with fibrosis in a variety of organs such as liver, skin, lung, gut, myocardium, vascular, pancreas, and it also plays a pivotal role in interstitial fibrosis and progression of CKD. Elevated plasma galectin-3 levels are also associated with increased risks of rapid renal function decline, incidence of CKD, and progressive renal impairment.9798 Galectin-3 has been proposed as a potential therapeutic target for the treatment of CKD, and currently clinical trials using a galectin-3 inhibitor are under investigation.98100
While vitamin E has various biological functions including enzymatic activity, gene regulation, and inhibition of platelet aggregation, the most important role of vitamin E is considered to be its antioxidant effect. Reactive oxygen species have been known to play an important role in the development of AKI.101 Vitamin E is able to bind to various reactive oxidant species such as superoxide free radicals, and it is possible to prevent damage caused by reactive oxygen species. The protective effect of vitamin E against AKI was first reported more than 2 decades ago, thereafter therapeutic action of vitamin E has been demonstrated in dozens of studies using a variety of AKI model induced by ischemia-reperfusion, nephrotoxic drugs, and contrast agents, etc.101 A meta-analysis suggested that vitamin E plus hydration significantly reduced the risk of contrast-induced AKI in patients with renal impairment compared with hydration alone.102 However, several researchers maintained that a single vitamin E administration did not have a beneficial effect on the prevention and severity of AKI, as the oxidative stress in the kidney tissue could not be absolutely related to renal dysfunction in some AKI models.103 According to a recently published network meta-analysis, vitamins and analogues have a preventive effect on contrast-induced AKI compared to hydration, but high-dose statins plus hydration with or without N-acetylcysteine is shown to be the most effective way to prevent the development of AKI.104 Thus, the combination of vitamin E and other therapy factors such as other vitamins, amino acids, drugs, and cells could be novel optimized methods, it should be elucidated through the experimental and clinical investigation in the future.
Herein, we summarized the role of various bioactive compounds that are associated with kidney regeneration (Table 1). Although many renotropic factors or signaling pathways have been identified, the mechanisms of these factors are not fully understood. It is still unclear how these compounds interact with injured kidney tissues for repair. To obtain better understanding about the renotropic systems, determination of more precise mechanisms of how renal cells recognize and respond to renal injury is required. It would be valuable if these bioactive compounds promote renal regeneration via the activation of intrinsic renal stem cells. For example, recent studies have demonstrated evidences of the activation and infiltration of host stem or progenitor cells through delivery of bioactive factors and the concept of tissue regeneration, namely in situ tissue regeneration, may be used for efficient kidney regeneration.105 The in situ tissue regeneration utilizes the body's natural healing capacity to repair damaged tissue or organs, and requires the safe and targeted in vivo delivery of the bioactive factors for enhanced therapeutic outcomes. Precise and well-controlled release of the growth factor or cytokines through various types of delivery vehicles such as hydrogel will be a crucial factor for efficient kidney repair.106 In conclusion, the therapeutic option using renotropic factors holds significant promise for treatment of kidney diseases. The understanding and utilization of bioactive compounds can play an important role in the success of these treatments and should be carefully considered in future therapies.
References
1. Maeshima A, Nakasatomi M, Nojima Y. Regenerative medicine for the kidney: renotropic factors, renal stem/progenitor cells, and stem cell therapy. Biomed Res Int. 2014; 2014:595493. PMID: 24895592.

2. Tran C, Damaser MS. Stem cells as drug delivery methods: application of stem cell secretome for regeneration. Adv Drug Deliv Rev. 2015; 82-83:1–11. PMID: 25451858.

3. Herberts CA, Kwa MS, Hermsen HP. Risk factors in the development of stem cell therapy. J Transl Med. 2011; 9:29. PMID: 21418664.

4. Pawitan JA. Prospect of stem cell conditioned medium in regenerative medicine. Biomed Res Int. 2014; 2014:965849. PMID: 25530971.

5. Little MH, Kairath P. Does renal repair recapitulate kidney development? J Am Soc Nephrol. 2017; 28:34–46. PMID: 27798243.

7. Matsumoto K, Nakamura T. Hepatocyte growth factor: renotropic role and potential therapeutics for renal diseases. Kidney Int. 2001; 59:2023–2038. PMID: 11380804.

8. Liu Y. Hepatocyte growth factor in kidney fibrosis: therapeutic potential and mechanisms of action. Am J Physiol Renal Physiol. 2004; 287:F7–F16. PMID: 15180923.

9. Li Y, Joseph A, Bhargava MM, Rosen EM, Nakamura T, Goldberg I. Effect of scatter factor and hepatocyte growth factor on motility and morphology of MDCK cells. In Vitro Cell Dev Biol. 1992; 28A:364–368. PMID: 1534555.

10. Montesano R, Matsumoto K, Nakamura T, Orci L. Identification of a fibroblast-derived epithelial morphogen as hepatocyte growth factor. Cell. 1991; 67:901–908. PMID: 1835669.

11. Santos OF, Moura LA, Rosen EM, Nigam SK. Modulation of HGF-induced tubulogenesis and branching by multiple phosphorylation mechanisms. Dev Biol. 1993; 159:535–548. PMID: 8405677.

12. Santos OF, Nigam SK. HGF-induced tubulogenesis and branching of epithelial cells is modulated by extracellular matrix and TGF-beta. Dev Biol. 1993; 160:293–302. PMID: 8253265.
13. Ishibashi K, Sasaki S, Sakamoto H, Hoshino Y, Nakamura T, Marumo F. Expressions of receptor gene for hepatocyte growth factor in kidney after unilateral nephrectomy and renal injury. Biochem Biophys Res Commun. 1992; 187:1454–1459. PMID: 1329737.

14. Liu Y, Sun AM, Dworkin LD. Hepatocyte growth factor protects renal epithelial cells from apoptotic cell death. Biochem Biophys Res Commun. 1998; 246:821–826. PMID: 9618296.

15. Yo Y, Morishita R, Nakamura S, Tomita N, Yamamoto K, Moriguchi A, et al. Potential role of hepatocyte growth factor in the maintenance of renal structure: anti-apoptotic action of HGF on epithelial cells. Kidney Int. 1998; 54:1128–1138. PMID: 9767528.

16. Kawaida K, Matsumoto K, Shimazu H, Nakamura T. Hepatocyte growth factor prevents acute renal failure and accelerates renal regeneration in mice. Proc Natl Acad Sci U S A. 1994; 91:4357–4361. PMID: 8183913.

17. Rotwein P. Structure, evolution, expression and regulation of insulin-like growth factors I and II. Growth Factors. 1991; 5:3–18. PMID: 1772660.

18. Hammerman MR, Miller SB. Therapeutic use of growth factors in renal failure. J Am Soc Nephrol. 1994; 5:1–11. PMID: 7948775.

19. Abolbashari M, Agcaoili SM, Lee MK, Ko IK, Aboushwareb T, Jackson JD, et al. Repopulation of porcine kidney scaffold using porcine primary renal cells. Acta Biomater. 2016; 29:52–61. PMID: 26596567.

20. Feld S, Hirschberg R. Growth hormone, the insulin-like growth factor system, and the kidney. Endocr Rev. 1996; 17:423–480. PMID: 8897021.

21. Bach LA, Hale LJ. Insulin-like growth factors and kidney disease. Am J Kidney Dis. 2015; 65:327–336. PMID: 25151409.

22. Ding H, Kopple JD, Cohen A, Hirschberg R. Recombinant human insulin-like growth factor-I accelerates recovery and reduces catabolism in rats with ischemic acute renal failure. J Clin Invest. 1993; 91:2281–2287. PMID: 8486787.

23. Miller SB, Martin DR, Kissane J, Hammerman MR. Insulin-like growth factor I accelerates recovery from ischemic acute tubular necrosis in the rat. Proc Natl Acad Sci U S A. 1992; 89:11876–11880. PMID: 1465411.

24. Imberti B, Morigi M, Tomasoni S, Rota C, Corna D, Longaretti L, et al. Insulin-like growth factor-1 sustains stem cell mediated renal repair. J Am Soc Nephrol. 2007; 18:2921–2928. PMID: 17942965.
25. Xinaris C, Morigi M, Benedetti V, Imberti B, Fabricio AS, Squarcina E, et al. A novel strategy to enhance mesenchymal stem cell migration capacity and promote tissue repair in an injury specific fashion. Cell Transplant. 2013; 22:423–436. PMID: 22889699.

26. Fisher DA, Salido EC, Barajas L. Epidermal growth factor and the kidney. Annu Rev Physiol. 1989; 51:67–80. PMID: 2653200.

27. Rogers SA, Ryan G, Hammerman MR. Metanephric transforming growth factor-alpha is required for renal organogenesis in vitro. Am J Physiol. 1992; 262(4 Pt 2):F533–F539. PMID: 1566867.

28. Rall LB, Scott J, Bell GI, Crawford RJ, Penschow JD, Niall HD, et al. Mouse prepro-epidermal growth factor synthesis by the kidney and other tissues. Nature. 1985; 313:228–231. PMID: 3871506.

29. Humes HD, Cieslinski DA, Coimbra TM, Messana JM, Galvao C. Epidermal growth factor enhances renal tubule cell regeneration and repair and accelerates the recovery of renal function in postischemic acute renal failure. J Clin Invest. 1989; 84:1757–1761. PMID: 2592559.

30. Morin NJ, Laurent G, Nonclercq D, Toubeau G, Heuson-Stiennon JA, Bergeron MG, et al. Epidermal growth factor accelerates renal tissue repair in a model of gentamicin nephrotoxicity in rats. Am J Physiol. 1992; 263(5 Pt 2):F806–F811. PMID: 1443171.

31. Coimbra TM, Cieslinski DA, Humes HD. Epidermal growth factor accelerates renal repair in mercuric chloride nephrotoxicity. Am J Physiol. 1990; 259(3 Pt 2):F438–F443. PMID: 2396670.

32. Sakai M, Zhang M, Homma T, Garrick B, Abraham JA, McKanna JA, et al. Production of heparin binding epidermal growth factor-like growth factor in the early phase of regeneration after acute renal injury. Isolation and localization of bioactive molecules. J Clin Invest. 1997; 99:2128–2138. PMID: 9151785.

33. Homma T, Sakai M, Cheng HF, Yasuda T, Coffey RJ Jr, Harris RC. Induction of heparin-binding epidermal growth factor-like growth factor mRNA in rat kidney after acute injury. J Clin Invest. 1995; 96:1018–1025. PMID: 7635938.

34. Zhuang S, Kinsey GR, Rasbach K, Schnellmann RG. Heparin-binding epidermal growth factor and Src family kinases in proliferation of renal epithelial cells. Am J Physiol Renal Physiol. 2008; 294:F459–F468. PMID: 18171996.

35. El Sabbahy M, Vaidya VS. Ischemic kidney injury and mechanisms of tissue repair. Wiley Interdiscip Rev Syst Biol Med. 2011; 3:606–618. PMID: 21197658.
36. Basile DP, Fredrich K, Chelladurai B, Leonard EC, Parrish AR. Renal ischemia reperfusion inhibits VEGF expression and induces ADAMTS-1, a novel VEGF inhibitor. Am J Physiol Renal Physiol. 2008; 294:F928–F936. PMID: 18272597.

37. Leonard EC, Friedrich JL, Basile DP. VEGF-121 preserves renal microvessel structure and ameliorates secondary renal disease following acute kidney injury. Am J Physiol Renal Physiol. 2008; 295:F1648–F1657. PMID: 18799550.

38. Chade AR, Kelsen S. Renal microvascular disease determines the responses to revascularization in experimental renovascular disease. Circ Cardiovasc Interv. 2010; 3:376–383. PMID: 20587789.

39. Iliescu R, Fernandez SR, Kelsen S, Maric C, Chade AR. Role of renal microcirculation in experimental renovascular disease. Nephrol Dial Transplant. 2010; 25:1079–1087. PMID: 19934087.

40. Mori da Cunha MG, Zia S, Beckmann DV, Carlon MS, Arcolino FO, Albersen M, et al. Vascular endothelial growth factor up-regulation in human amniotic fluid stem cell enhances nephroprotection after ischemia-reperfusion injury in the rat. Crit Care Med. 2017; 45:e86–e96. PMID: 27548820.

41. Massagué J. TGFβ signalling in context. Nat Rev Mol Cell Biol. 2012; 13:616–630. PMID: 22992590.

42. Border WA, Noble NA, Yamamoto T, Tomooka S, Kagami S. Antagonists of transforming growth factor-beta: a novel approach to treatment of glomerulonephritis and prevention of glomerulosclerosis. Kidney Int. 1992; 41:566–570. PMID: 1573830.
43. O'Shea M, Miller SB, Finkel K, Hammerman MR. Roles of growth hormone and growth factors in the pathogenesis and treatment of kidney disease. Curr Opin Nephrol Hypertens. 1993; 2:67–72. PMID: 7922170.
44. Border WA, Okuda S, Languino LR, Sporn MB, Ruoslahti E. Suppression of experimental glomerulonephritis by antiserum against transforming growth factor beta 1. Nature. 1990; 346:371–374. PMID: 2374609.
45. Okuda S, Nakamura T, Yamamoto T, Ruoslahti E, Border WA. Dietary protein restriction rapidly reduces transforming growth factor beta 1 expression in experimental glomerulonephritis. Proc Natl Acad Sci U S A. 1991; 88:9765–9769. PMID: 1946401.

46. Furuichi K, Kaneko S, Wada T. Chemokine/chemokine receptor-mediated inflammation regulates pathologic changes from acute kidney injury to chronic kidney disease. Clin Exp Nephrol. 2009; 13:9–14. PMID: 19085040.

47. Floege J, Johnson RJ. Multiple roles for platelet-derived growth factor in renal disease. Miner Electrolyte Metab. 1995; 21:271–282. PMID: 7565476.
48. Bessho K, Mizuno S, Matsumoto K, Nakamura T. Counteractive effects of HGF on PDGF-induced mesangial cell proliferation in a rat model of glomerulonephritis. Am J Physiol Renal Physiol. 2003; 284:F1171–F1180. PMID: 12595276.
49. Alpers CE, Seifert RA, Hudkins KL, Johnson RJ, Bowen-Pope DF. Developmental patterns of PDGF B-chain, PDGF-receptor, and alpha-actin expression in human glomerulogenesis. Kidney Int. 1992; 42:390–399. PMID: 1405322.
50. Nakagawa T, Sasahara M, Haneda M, Kataoka H, Nakagawa H, Yagi M, et al. Role of PDGF B-chain and PDGF receptors in rat tubular regeneration after acute injury. Am J Pathol. 1999; 155:1689–1699. PMID: 10550325.

51. Nguyen TQ, Goldschmeding R. Bone morphogenetic protein-7 and connective tissue growth factor: novel targets for treatment of renal fibrosis? Pharm Res. 2008; 25:2416–2426. PMID: 18266088.

52. Simon M, Maresh JG, Harris SE, Hernandez JD, Arar M, Olson MS, et al. Expression of bone morphogenetic protein-7 mRNA in normal and ischemic adult rat kidney. Am J Physiol. 1999; 276(3 Pt 2):F382–F389. PMID: 10070161.
53. Hruska KA, Guo G, Wozniak M, Martin D, Miller S, Liapis H, et al. Osteogenic protein-1 prevents renal fibrogenesis associated with ureteral obstruction. Am J Physiol Renal Physiol. 2000; 279:F130–F143. PMID: 10894795.

54. Almanzar MM, Frazier KS, Dube PH, Piqueras AI, Jones WK, Charette MF, et al. Osteogenic protein-1 mRNA expression is selectively modulated after acute ischemic renal injury. J Am Soc Nephrol. 1998; 9:1456–1463. PMID: 9697668.

55. De Petris L, Hruska KA, Chiechio S, Liapis H. Bone morphogenetic protein-7 delays podocyte injury due to high glucose. Nephrol Dial Transplant. 2007; 22:3442–3450. PMID: 17686813.

56. Zeisberg M, Hanai J, Sugimoto H, Mammoto T, Charytan D, Strutz F, et al. BMP-7 counteracts TGF-beta1-induced epithelial-to-mesenchymal transition and reverses chronic renal injury. Nat Med. 2003; 9:964–968. PMID: 12808448.
57. Gould SE, Day M, Jones SS, Dorai H. BMP-7 regulates chemokine, cytokine, and hemodynamic gene expression in proximal tubule cells. Kidney Int. 2002; 61:51–60. PMID: 11786084.
58. Wang S, Hirschberg R. BMP7 antagonizes TGF-beta-dependent fibrogenesis in mesangial cells. Am J Physiol Renal Physiol. 2003; 284:F1006–F1013. PMID: 12676736.
59. Mitu GM, Wang S, Hirschberg R. BMP7 is a podocyte survival factor and rescues podocytes from diabetic injury. Am J Physiol Renal Physiol. 2007; 293:F1641–F1648. PMID: 17804487.

60. Vukicevic S, Basic V, Rogic D, Basic N, Shih MS, Shepard A, et al. Osteogenic protein-1 (bone morphogenetic protein-7) reduces severity of injury after ischemic acute renal failure in rat. J Clin Invest. 1998; 102:202–214. PMID: 9649574.

61. Morrissey J, Hruska K, Guo G, Wang S, Chen Q, Klahr S. Bone morphogenetic protein-7 improves renal fibrosis and accelerates the return of renal function. J Am Soc Nephrol. 2002; 13(Suppl 1):S14–S21. PMID: 11792757.

62. Wang S, Chen Q, Simon TC, Strebeck F, Chaudhary L, Morrissey J, et al. Bone morphogenic protein-7 (BMP-7), a novel therapy for diabetic nephropathy. Kidney Int. 2003; 63:2037–2049. PMID: 12753291.
63. Nishida M, Hamaoka K. How does G-CSF act on the kidney during acute tubular injury? Nephron Exp Nephrol. 2006; 104:e123–e128. PMID: 16902315.

64. Zhang Y, Woodward VK, Shelton JM, Richardson JA, Zhou XJ, Link D, et al. Ischemia-reperfusion induces G-CSF gene expression by renal medullary thick ascending limb cells in vivo and in vitro. Am J Physiol Renal Physiol. 2004; 286:F1193–F1201. PMID: 14734360.

65. Nishida M, Fujimoto S, Toiyama K, Sato H, Hamaoka K. Effect of hematopoietic cytokines on renal function in cisplatin-induced ARF in mice. Biochem Biophys Res Commun. 2004; 324:341–347. PMID: 15465024.

66. Stokman G, Leemans JC, Claessen N, Weening JJ, Florquin S. Hematopoietic stem cell mobilization therapy accelerates recovery of renal function independent of stem cell contribution. J Am Soc Nephrol. 2005; 16:1684–1692. PMID: 15829714.

67. Tögel F, Isaac J, Westenfelder C. Hematopoietic stem cell mobilization-associated granulocytosis severely worsens acute renal failure. J Am Soc Nephrol. 2004; 15:1261–1267. PMID: 15100366.
68. Togel FE, Westenfelder C. Role of SDF-1 as a regulatory chemokine in renal regeneration after acute kidney injury. Kidney Int Suppl. 2011; 1:87–89.

69. Ceradini DJ, Kulkarni AR, Callaghan MJ, Tepper OM, Bastidas N, Kleinman ME, et al. Progenitor cell trafficking is regulated by hypoxic gradients through HIF-1 induction of SDF-1. Nat Med. 2004; 10:858–864. PMID: 15235597.

70. Gröne HJ, Cohen CD, Gröne E, Schmidt C, Kretzler M, Schlöndorff D, et al. Spatial and temporally restricted expression of chemokines and chemokine receptors in the developing human kidney. J Am Soc Nephrol. 2002; 13:957–967. PMID: 11912255.

71. Tögel F, Isaac J, Hu Z, Weiss K, Westenfelder C. Renal SDF-1 signals mobilization and homing of CXCR4-positive cells to the kidney after ischemic injury. Kidney Int. 2005; 67:1772–1784. PMID: 15840024.

72. Stokman G, Stroo I, Claessen N, Teske GJ, Florquin S, Leemans JC. SDF-1 provides morphological and functional protection against renal ischaemia/reperfusion injury. Nephrol Dial Transplant. 2010; 25:3852–3859. PMID: 20519232.

73. Ohnishi H, Mizuno S, Mizuno-Horikawa Y, Kato T. Stromal cell-derived factor-1 (SDF1)-dependent recruitment of bone marrow-derived renal endothelium-like cells in a mouse model of acute kidney injury. J Vet Med Sci. 2015; 77:313–319. PMID: 25833353.

74. Dudakov JA, Hanash AM, van den Brink MR. Interleukin-22: immunobiology and pathology. Annu Rev Immunol. 2015; 33:747–785. PMID: 25706098.

75. Weidenbusch M, Rodler S, Anders HJ. Interleukin-22 in kidney injury and regeneration. Am J Physiol Renal Physiol. 2015; 308:F1041–F1046. PMID: 25740595.

76. Kulkarni OP, Hartter I, Mulay SR, Hagemann J, Darisipudi MN, Kumar Vr S, et al. Toll-like receptor 4-induced IL-22 accelerates kidney regeneration. J Am Soc Nephrol. 2014; 25:978–989. PMID: 24459235.

77. Xu MJ, Feng D, Wang H, Guan Y, Yan X, Gao B. IL-22 ameliorates renal ischemia-reperfusion injury by targeting proximal tubule epithelium. J Am Soc Nephrol. 2014; 25:967–977. PMID: 24459233.

78. Zhang SL, Guo J, Moini B, Ingelfinger JR. Angiotensin II stimulates Pax-2 in rat kidney proximal tubular cells: impact on proliferation and apoptosis. Kidney Int. 2004; 66:2181–2192. PMID: 15569307.

79. Weber KT. Fibrosis, a common pathway to organ failure: angiotensin II and tissue repair. Semin Nephrol. 1997; 17:467–491. PMID: 9316215.
80. Gagliardini E, Benigni A. Drugs to foster kidney regeneration in experimental animals and humans. Nephron Exp Nephrol. 2014; 126:91. PMID: 24854648.

81. Benigni A, Morigi M, Remuzzi G. Kidney regeneration. Lancet. 2010; 375:1310–1317. PMID: 20382327.

82. Arcasoy MO. The non-haematopoietic biological effects of erythropoietin. Br J Haematol. 2008; 141:14–31. PMID: 18324962.

83. Sharples EJ, Patel N, Brown P, Stewart K, Mota-Philipe H, Sheaff M, et al. Erythropoietin protects the kidney against the injury and dysfunction caused by ischemia-reperfusion. J Am Soc Nephrol. 2004; 15:2115–2124. PMID: 15284297.

84. Spandou E, Tsouchnikas I, Karkavelas G, Dounousi E, Simeonidou C, Guiba-Tziampiri O, et al. Erythropoietin attenuates renal injury in experimental acute renal failure ischaemic/reperfusion model. Nephrol Dial Transplant. 2006; 21:330–336. PMID: 16221709.

85. Yang CW, Li C, Jung JY, Shin SJ, Choi BS, Lim SW, et al. Preconditioning with erythropoietin protects against subsequent ischemia-reperfusion injury in rat kidney. FASEB J. 2003; 17:1754–1755. PMID: 12958199.

86. Bagnis C, Beaufils H, Jacquiaud C, Adabra Y, Jouanneau C, Le Nahour G, et al. Erythropoietin enhances recovery after cisplatin-induced acute renal failure in the rat. Nephrol Dial Transplant. 2001; 16:932–938. PMID: 11328897.

87. Lee SH, Li C, Lim SW, Ahn KO, Choi BS, Kim YS, et al. Attenuation of interstitial inflammation and fibrosis by recombinant human erythropoietin in chronic cyclosporine nephropathy. Am J Nephrol. 2005; 25:64–76. PMID: 15746540.

88. Dardashti A, Ederoth P, Algotsson L, Brondén B, Grins E, Larsson M, et al. Erythropoietin and protection of renal function in cardiac surgery (the EPRICS Trial). Anesthesiology. 2014; 121:582–590. PMID: 25225746.

89. Song YR, Lee T, You SJ, Chin HJ, Chae DW, Lim C, et al. Prevention of acute kidney injury by erythropoietin in patients undergoing coronary artery bypass grafting: a pilot study. Am J Nephrol. 2009; 30:253–260. PMID: 19494484.

90. Zhu F, Chong Lee Shin OL, Xu H, Zhao Z, Pei G, Hu Z, et al. Melatonin promoted renal regeneration in folic acid-induced acute kidney injury via inhibiting nucleocytoplasmic translocation of HMGB1 in tubular epithelial cells. Am J Transl Res. 2017; 9:1694–1707. PMID: 28469775.
91. Chang YC, Hsu SY, Yang CC, Sung PH, Chen YL, Huang TH, et al. Enhanced protection against renal ischemia-reperfusion injury with combined melatonin and exendin-4 in a rodent model. Exp Biol Med (Maywood). 2016; 241:1588–1602. PMID: 27037275.

92. Yildirim ME, Badem H, Cakmak M, Yilmaz H, Kosem B, Karatas OF, et al. Melatonin protects kidney against apoptosis induced by acute unilateral ureteral obstruction in rats. Cent European J Urol. 2016; 69:225–230.
93. Maeshima A, Nojima Y, Kojima I. The role of the activin-follistatin system in the developmental and regeneration processes of the kidney. Cytokine Growth Factor Rev. 2001; 12:289–298. PMID: 11544099.

94. Fang DY, Lu B, Hayward S, de Kretser DM, Cowan PJ, Dwyer KM. The role of activin A and B and the benefit of follistatin treatment in renal ischemia-reperfusion injury in mice. Transplant Direct. 2016; 2:e87. PMID: 27830181.

95. Maeshima A, Zhang YQ, Nojima Y, Naruse T, Kojima I. Involvement of the activin-follistatin system in tubular regeneration after renal ischemia in rats. J Am Soc Nephrol. 2001; 12:1685–1695. PMID: 11461941.

96. Maeshima A, Mishima K, Yamashita S, Nakasatomi M, Miya M, Sakurai N, et al. Follistatin, an activin antagonist, ameliorates renal interstitial fibrosis in a rat model of unilateral ureteral obstruction. Biomed Res Int. 2014; 2014:376191. PMID: 24883308.

97. Saccon F, Gatto M, Ghirardello A, Iaccarino L, Punzi L, Doria A. Role of galectin-3 in autoimmune and non-autoimmune nephropathies. Autoimmun Rev. 2017; 16:34–47. PMID: 27666815.

98. Chen SC, Kuo PL. The role of galectin-3 in the kidneys. Int J Mol Sci. 2016; 17:565. PMID: 27089335.

99. Nishiyama J, Kobayashi S, Ishida A, Nakabayashi I, Tajima O, Miura S, et al. Up-regulation of galectin-3 in acute renal failure of the rat. Am J Pathol. 2000; 157:815–823. PMID: 10980121.

100. Desmedt V, Desmedt S, Delanghe JR, Speeckaert R, Speeckaert MM. Galectin-3 in renal pathology: more than just an innocent bystander. Am J Nephrol. 2016; 43:305–317. PMID: 27166158.

101. Liu P, Feng Y, Wang Y, Zhou Y, Zhao L. Protective effect of vitamin E against acute kidney injury. Biomed Mater Eng. 2015; 26(Suppl 1):S2133–S2144. PMID: 26405992.

102. Cho MH, Kim SN, Park HW, Chung S, Kim KS. Could vitamin E prevent contrast-induced acute kidney injury? A systematic review and meta-analysis. J Korean Med Sci. 2017; 32:1468–1473. PMID: 28776342.

103. Kim HB, Shanu A, Wood S, Parry SN, Collet M, McMahon A, et al. Phenolic antioxidants tert-butyl-bisphenol and vitamin E decrease oxidative stress and enhance vascular function in an animal model of rhabdomyolysis yet do not improve acute renal dysfunction. Free Radic Res. 2011; 45:1000–1012. PMID: 21726176.

104. Su X, Xie X, Liu L, Lv J, Song F, Perkovic V, et al. Comparative effectiveness of 12 treatment strategies for preventing contrast-induced acute kidney injury: a systematic review and Bayesian network meta-analysis. Am J Kidney Dis. 2017; 69:69–77. PMID: 27707552.

105. Ko IK, Ju YM, Chen T, Atala A, Yoo JJ, Lee SJ. Combined systemic and local delivery of stem cell inducing/recruiting factors for in situ tissue regeneration. FASEB J. 2012; 26:158–168. PMID: 21965595.
106. Ko IK, Lee SJ, Atala A, Yoo JJ. In situ tissue regeneration through host stem cell recruitment. Exp Mol Med. 2013; 45:e57. PMID: 24232256.

Table 1
Major Findings of Experimental Studies on Bioactive Compounds Related to Kidney Diseases
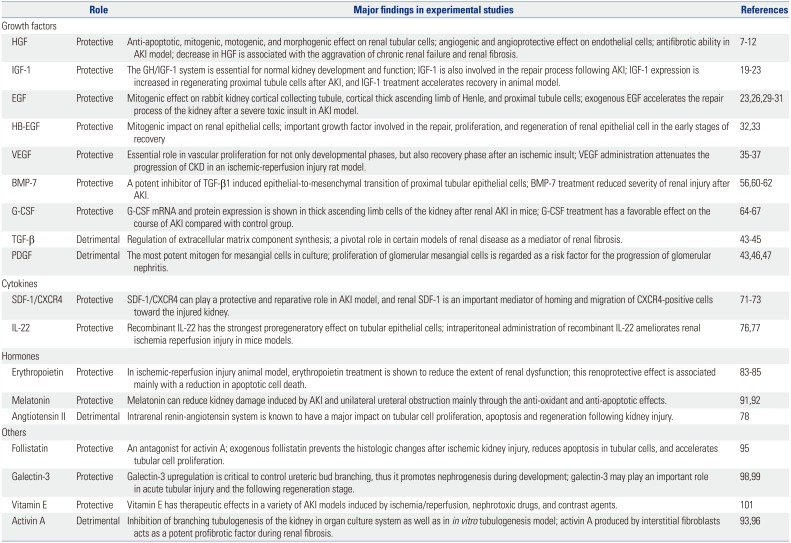
| Role | Major findings in experimental studies | References | |
|---|---|---|---|
| Growth factors | |||
| HGF | Protective | Anti-apoptotic, mitogenic, motogenic, and morphogenic effect on renal tubular cells; angiogenic and angioprotective effect on endothelial cells; antifibrotic ability in AKI model; decrease in HGF is associated with the aggravation of chronic renal failure and renal fibrosis. | 789101112 |
| IGF-1 | Protective | The GH/IGF-1 system is essential for normal kidney development and function; IGF-1 is also involved in the repair process following AKI; IGF-1 expression is increased in regenerating proximal tubule cells after AKI, and IGF-1 treatment accelerates recovery in animal model. | 1920212223 |
| EGF | Protective | Mitogenic effect on rabbit kidney cortical collecting tubule, cortical thick ascending limb of Henle, and proximal tubule cells; exogenous EGF accelerates the repair process of the kidney after a severe toxic insult in AKI model. | 2326293031 |
| HB-EGF | Protective | Mitogenic impact on renal epithelial cells; important growth factor involved in the repair, proliferation, and regeneration of renal epithelial cell in the early stages of recovery | 3233 |
| VEGF | Protective | Essential role in vascular proliferation for not only developmental phases, but also recovery phase after an ischemic insult; VEGF administration attenuates the progression of CKD in an ischemic-reperfusion injury rat model. | 353637 |
| BMP-7 | Protective | A potent inhibitor of TGF-β1 induced epithelial-to-mesenchymal transition of proximal tubular epithelial cells; BMP-7 treatment reduced severity of renal injury after AKI. | 56606162 |
| G-CSF | Protective | G-CSF mRNA and protein expression is shown in thick ascending limb cells of the kidney after renal AKI in mice; G-CSF treatment has a favorable effect on the course of AKI compared with control group. | 64656667 |
| TGF-β | Detrimental | Regulation of extracellular matrix component synthesis; a pivotal role in certain models of renal disease as a mediator of renal fibrosis. | 434445 |
| PDGF | Detrimental | The most potent mitogen for mesangial cells in culture; proliferation of glomerular mesangial cells is regarded as a risk factor for the progression of glomerular nephritis. | 434647 |
| Cytokines | |||
| SDF-1/CXCR4 | Protective | SDF-1/CXCR4 can play a protective and reparative role in AKI model, and renal SDF-1 is an important mediator of homing and migration of CXCR4-positive cells toward the injured kidney. | 717273 |
| IL-22 | Protective | Recombinant IL-22 has the strongest proregeneratory effect on tubular epithelial cells; intraperitoneal administration of recombinant IL-22 ameliorates renal ischemia reperfusion injury in mice models. | 7677 |
| Hormones | |||
| Erythropoietin | Protective | In ischemic-reperfusion injury animal model, erythropoietin treatment is shown to reduce the extent of renal dysfunction; this renoprotective effect is associated mainly with a reduction in apoptotic cell death. | 838485 |
| Melatonin | Protective | Melatonin can reduce kidney damage induced by AKI and unilateral ureteral obstruction mainly through the anti-oxidant and anti-apoptotic effects. | 9192 |
| Angtiotensin II | Detrimental | Intrarenal renin-angiotensin system is known to have a major impact on tubular cell proliferation, apoptosis and regeneration following kidney injury. | 78 |
| Others | |||
| Follistatin | Protective | An antagonist for activin A; exogenous follistatin prevents the histologic changes after ischemic kidney injury, reduces apoptosis in tubular cells, and accelerates tubular cell proliferation. | 95 |
| Galectin-3 | Protective | Galectin-3 upregulation is critical to control ureteric bud branching, thus it promotes nephrogenesis during development; galectin-3 may play an important role in acute tubular injury and the following regeneration stage. | 9899 |
| Vitamin E | Protective | Vitamin E has therapeutic effects in a variety of AKI models induced by ischemia/reperfusion, nephrotoxic drugs, and contrast agents. | 101 |
| Activin A | Detrimental | Inhibition of branching tubulogenesis of the kidney in organ culture system as well as in in vitro tubulogenesis model; activin A produced by interstitial fibroblasts acts as a potent profibrotic factor during renal fibrosis. | 9396 |
AKI, acute kidney injury; HGF, hepatocyte growth factor; IGF-1, insulin-like growth factor-1; GH, growth hormone; EGF, epidermal growth factor; HB-EGF, heparin-binding EGF-like growth factor; VEGF, vascular endothelial growth factor; CKD, chronic kidney disease; BMP-7, bone morphogenetic protein-7; G-CSF, granulocyte-colony stimulating factor; TGF-β, transforming growth factor-β; PDGF, platelet-derived growth factor; SDF-1, stromal derived factor-1; CXCR4, C-X-C chemokine receptor type 4.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download