Abstract
Purpose
The objective of this study was to describe the clinical phenotypes of children and adolescents with cystic fibrosis (CF); and to assess the role of pancreatic insufficiency and neonatal screening in diagnosis.
Methods
A cross-sectional study was conducted, which included 77 patients attending a reference center of CF between 2014 and 2016. Epidemiological data, anthropometric measurements, and the presence of pulmonary, pancreatic, gastrointestinal and hepatobiliary manifestations were evaluated based on clinical data and complementary examinations.
Results
Of the 77 patients, 51.9% were male, with a median age of 147 months (7.0–297.0 months), and the majority showed adequate nutritional status. The most common phenotype was pulmonary (92.2%), followed by pancreatic (87.0%), with pancreatic insufficiency in most cases. Gastrointestinal manifestation occurred in 46.8%, with constipation being the more common factor. Hepatobiliary disease occurred in 62.3% of patients. The group with pancreatic insufficiency was diagnosed earlier (5.0 months) when compared to the group with sufficiency (84.0 months) (p=0.01). The age of diagnosis was reduced following implementation of neonatal screening protocols for CF (6.0 months before vs. 3.0 months after, p=0.02).
Conclusion
The pulmonary phenotype was the most common, although extrapulmonary manifestations were frequent and clinically relevant, and should mandate early detection and treatment. Neonatal screening for CF led to earlier diagnosis in patients with pancreatic failure, and therefore, should be adopted universally.
Cystic fibrosis (CF) is an autosomal recessive genetic disorder that most commonly decreases life expectancy in Caucasians [1]. Lung disease is the main cause of morbidity and mortality in patients with CF, often involving the digestive tract [1]. The majority of affected individuals present gastrointestinal, pancreatic and/or hepatic manifestations throughout their lives, which negatively impacts the evolution of the disease, quality of life and survival rate [2].
In CF, genetic alteration interferes with the production of the CF transmembrane conductance regulator (CFTR), which regulates the secretion of chloride and fluids in the exocrine glands, bronchial gland, intestine, pancreatic duct, biliary and reproductive systems. CF patients produce thickened secretions, which occlude the light of the cavity of the structures involved, generating inflammation and compromising the function of the affected organs [3,4].
More than 2,000 mutations causing CF have been described, with the F508del mutation being the most commonly observed [3]. Various mutations result in defective and unstable CFTR proteins. These molecular and functional differences, associated with environmental and individual factors, result in varying phenotypes of the disease, hindering the diagnosis, with unfavorable consequences [1].
Extrapulmonary clinical manifestations related to the digestive tract reveal pancreatic, gastrointestinal and hepatobiliary dysfunction [4]. Independently of the manifestations, early diagnosis is critical for appropriate and prompt treatment to improve the quality of life in patients with CF [5].
The objectives of this study were as follows: (1) describe the clinical phenotypes of children and adolescents with CF in a reference center in Brazil; (2) assess the influence of clinical phenotype (pancreatic insufficiency) at the age of diagnosis; and, (3) evaluate the role of neonatal screening test in reducing the age of diagnosis.
The study was cross-sectional and analytical, using a series of cases, which included patients with CF who were treated by the pediatric reference center in Brasilia.
The diagnosis of CF was based on the existing international criteria at the time of the study [6]. Until 2011, patients were referred to diagnostic evaluation by presenting family history or clinical diagnosis of CF, or in specific cases, via positive neonatal screening, carried out in private laboratories. The diagnosis was confirmed using two positive sweat tests (dosage of chloride in sweat exceeding 60 mEq/L) or molecular genetic analysis of positive CFTR mutations (2 mutations). As of November 2011, the neonatal screening test of the the federal district's public health system, was also systematically included, based on testing for immunoreactive trypsinogen (IRT), with an active investigation of suspected cases, according to algorithms (IRT, IRT and sweat testing), and the diagnosis confirmed by the standard methodologies [6].
All patients up to the age of 18 years, with a diagnosis of CF, who were treated at the reference center between January 2014 and June 2016, were included in the study following informed consent.
Data including epidemiological (sex, current age, age of diagnosis, country of birth, and origin), anthropometric (weight [kg], height [cm], for calculation of body mass index [BMI, kg/m2]), clinical measurements (clinical history and physical examination), complications during the disease, medications used and complementary examinations (laboratory, imaging and endoscopic) were evaluated. The nutritional evaluation was established based on the classification of Z score of the World Health Organization [7].
Pulmonary, pancreatic, gastrointestinal and hepatobiliary manifestations were defined by clinical data and complementary examinations described below.
Pulmonary involvement was based on clinical evaluation (persistent respiratory symptoms), functional (by spirometry) [8] and radiological (chest X-ray and/or chest computed tomography) investigations. This study also analyzed the data obtained from cultures of respiratory secretions (sputum, or oropharynx or smear routinely collected). Chronic colonization was defined when the same bacterium was isolated in more than 50% of the cultures within the previous 12 months [9].
Pancreatic involvement was based on the diagnosis of pancreatic insufficiency at the pre-screening clinic (malabsorptive syndrome or macroscopic presence of fat in the feces), associated with the 24-hour measurement of quantitative fecal fat (>7 g/100 g) [4], positive Sudan III stain or fecal elastase (<200 µg/g of feces).
Diabetes related to CF (CFRD) was evaluated in annual screening (beginning from the age of 10 years or in those pre-screened clinically), using the oral tolerance test for glucose of 0 and 120 minutes and glycated hemoglobin data. Patients with plasma glucose >200 µg/dL, within 120 minutes, received a diagnosis of CFRD [10].
Chronic pancreatitis was diagnosed based on clinical characteristics, evaluation of pancreatic function and identification of parenchymal changes in imaging exams [11].
Gastrointestinal manifestations were investigated via clinical evaluation associated with complementary examinations as needed. The criteria of the North American and European Societies of Gastroenterology, Hepatology and Pediatric nutrition were used for the diagnosis of gastric reflux disease (GERD) [12].
Hepatic and biliary involvement was defined via clinical evaluation (jaundice, pruritus, coliuria, fecal hypo/acolia, and hepatosplenomegaly), complemented by routine liver examinations: levels of liver enzymes (alanine aminotransferase, aspartate aminotransferase, gamma-glutamyltransferase, and alkaline phosphatase), total bilirubin and fractions, total protein and fractions, international standardized profile (ISP) and abdominal ultrasound. Hepatic elastography was used by a single examiner for the detection of hepatic fibrosis, using the FibroScan® (Echosens, Paris, France), with a cut-off limit >5.0 kPa for the presence of hepatic fibrosis [13]. Other complementary exams, such as upper endoscopy, were carried out in selected cases.
A total of 77 patients were included in the study: 40 (51.9%) were male, with an median of age of 147.0 months (7.0–297.0 months). The median age of diagnosis was 6.0 months (1.0–168.0 months).
The majority of patients, i.e., 56 (72.7%), were born and raised in the Federal District of Brazil. The remaining patients were residents of other Brazilian states: 7 (9.1%) were from Bahia, 3 (3.9%) of Goiás, 3 (3.9%) of Tocantins, 2 (2.6%) of Minas Gerais, 2 (2.6%) of Piauí (3%), 2 (2.6%) of Rio de Janeiro, 1 (1.3%) of Roraima and 1 (1.3%) of Paraíba.
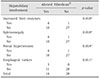
Regarding BMI and stature for age, patients were classified according to Table 1. Nearly 80% of the cases presented adequate nutritional status, and close to 90% presented height status that was adequate for their age.
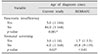
The pulmonary phenotype was the most frequent finding, affecting 71 patients (92.2%). Of the 77 cases, 50 (64.9%) performed spirometry maneuvers, with the following results: 25 (50.0%) presented normal spirometry, 15 (30.0%) mild obstructive ventilatory disorder (OVD), 5 (10.0%) moderate OVD, 3 (6.0%) severe OVD and 2 (4.0%) with mixed disturbances. The average forced expiratory volume in one second (FEV1) was 83% (±19) and the forced vital capacity (FVC) was 92% (±18) (Table 2).
Chronic colonization was evident in 57 (74.0%) of the cases evaluated, with the following most frequent pathogens: Staphylococcus aureus 43 cases (55.8%) and Pseudomonas aeruginosa 27 cases (35.1%).
Only three patients (3.9%) presented with the pulmonary phenotype, without extrapulmonary manifestations.
Pancreatic involvement occurred in 67 cases (87.0%), the second most frequent phenotype. Most of the patients presented pancreatic insufficiency. About 14% presented CFRD and only one (1.3%) patient had pancreatitis (Table 2).
Gastrointestinal involvement was observed in 36 cases (46.8%), with constipation being the most common manifestation (33.8%). Table 2 describes the frequency of other gastrointestinal manifestations observed.
Hepatobiliary involvement occurred in 48 (62.3%) cases, with hepatomegaly in 22.1% of the total sample. The other hepatobiliary manifestations are described in Table 2. Among the patients with hepatobiliary involvement, 26 (54.2%) were treated with ursodeoxycholic acid (UDCA), and 19 (73.1%) of these presented reduced liver enzymes and improved echoradiographic aspects.
Of the 77 cases, 42 (54.5%) were subjected to hepatic elastography. Fibrosis (>5.0 kPa) was detected at 14 (33.3%), with a median of 6.85 kPa (2.5–14.4 kPa). The highest degree of fibrosis (14.4 kPa) was observed in a 14-year-old patient. The altered FibroScan® presented a statistically significant correlation with increased liver enzymes (p=0.018) and portal hypertension (p=0.018) (Table 3).
The diagnosis was made earlier in the group with pancreatic insufficiency, with a median of 5.0 months (1–144 months) when compared with the group with pancreatic sufficiency, with a median of 84.0 months (3–168 months) (p=0.01), as described in Table 4.
The median age of diagnosis prior to neonatal screening was 6.0 months (1–168 months), and subsequent to implementation of the test was 3.0 months (1–14 months) (p=0.02) (Table 4).
This is the first study evaluating the different clinical phenotypes of CF in Brazilian children, and the effect of implementation of neonatal screening for CF on the age of diagnosis.
In relation to the age of diagnosis, the median obtained (6.0 months) showed an improvement over the Brazilian Registry of Cystic Fibrosis (Registro Brasileiro de Fibrose Cística, REBRAFC) of 2014 (14.28 months) [14], possibly due to the absence of neonatal screening for CF in many states, which hindered early diagnosis. The current study evaluated a single center, which justified the difference in the age of diagnosis. Similar data correlating with the current median age of patients (147.0 months) were reported in the American annual record of patients in 2012 [15].
Most of the evaluated patients (83.1%) were classified as eutrophic (Table 1). This result was different from an Indian study, where 96.3% presented failure to thrive [16]. It also contrasted with REBRAFC of 2014, which revealed inadequate nutritional status among many of the identified patients [14]. The reference center of this study included an interdisciplinary team, nutritional and therapeutic support, which contributed to the improvement of nutritional status. Normal nutritional status is associated with better lung function and longer survival.
The pulmonary phenotype was the most frequent (92.2%), similar to that described by Rizzo et al. (92.0%) [17]. Half of the patients capable of performing spirometric maneuvers showed normal spirometry, higher than the reported data in the REBRAFC, where 40% of the patients underwent normal spirometry [14]. The averages of FEV1 and FVC were also better than those described in the REBRAFC [14]. It has been reported that BMI values above the 50 percentile are associated with better pulmonary function [18], which explain the favorable pulmonary indices in this study.
The colonization of S. aureus in more than half of the patients in this study is consistent with the literature. According to Goss and Muhlebach [19], S. aureus is one of the earliest and most frequent pathogens isolated from the respiratory tract of patients with CF. The case study involving P. aeruginosa showed a lower frequency than that of REBRAFC [14].
The importance of recognizing the non-respiratory complications of CF is well known [20]. Only 3.9% of the evaluated patients presented no extrapulmonary manifestations involving pancreatic, gastrointestinal and hepatobiliary dysfunction.
The pancreatic phenotype was the second most frequent, with pancreatic insufficiency diagnosed in most of the cases (Table 2). It is known that 90% of CF carriers are pancreatically insufficient, with malabsorptive syndrome being the classical clinical presentation, also with steatorrhoea and growth insufficiency, mainly due to poor absorption of nutrients [21].
The prevalence of CFRD observed resembles the known condition in Brazil (13.3%) [18]. However, it is higher than that reported by international registration (2.9%) [16], probably justified by ethnic and/or geographical differences.
Only one patient, who had pancreatic insufficiency, showed signs of chronic pancreatitis in an abdominal ultrasound. It is known that the imaging of patients with CF reveals fatty substitution, calcification and atrophy of the pancreas consistent with chronic lesion [1], which may justify the findings in the described patient.
Gastrointestinal involvement was present in almost half of the cases, reflecting the trend reported in the Brazilian literature [17]. Constipation was the most frequent gastrointestinal manifestation (33.8%), similar to that described by Gelfond and Borowitz (32.0%) [2]. It resulted in increased viscosity of intestinal content as well as distal intestinal obstruction syndrome (DIOS) [2]. In this study, 11.7% of the patients presented DIOS, with incidence similar to that observed in world centers [22]. This is a unique condition of CF and is characterized by complete or incomplete fecal obstruction in the ileocecal region [2].
The prevalence of identified GERD (9.1%) was higher than in REBRAFC (5.6%) [14], but lower than that reported by foreign studies [23]. The prevalence variation is justified by the difference in the methods used to define GERD.
It is known that the occurrence of GERD in these patients is 6 to 8 times greater than in healthy children. Several factors contribute to the increase: prolonged gastric emptying, medicines, and increased abdominal pressure by coughing and respiratory physiotherapy [24].
The prevalence of meconium ileus (9.1%) was close to that described in literature [25]. This condition is considered a neonatal emergency, often associated with serious mutations [25].
The occurrence of rectal prolapse was observed in 2.6% of the cases (Table 2). The literature estimates that less than 5% of CF patients will have rectal prolapse [26]. Rectal prolapse is probably attributed to the earlier diagnosis of the disease by screening newborns, prevention of constipation and better formulations of pancreatic enzyme replacement therapy [4]. Although CF is not the cause of rectal prolapse in most cases, it should be included in the differential diagnosis [4].
The prevalence of peptic ulcerative disease (PUD) was 2.6%, and negative for Helicobacter pylori in all cases. It has already been described that despite the reduction of bicarbonate secretion in patients with CF, habitual prevalence or even decreased PUD and infections by H. pylori are observed [27]. This “CF paradox” may be due to the bicarbonate retained in the cytoplasm of the enterocyte, which prevents injury and ulcer formation, or due to frequent use of antibiotics [27].
Only one (1) patient presented fibrosing colonopathy, reinforcing reduced incidence of this condition after standardization of the pancreatic enzyme replacement therapy described in the literature [4].
The frequency of hepatic involvement observed in this study (62.3%) was greater than that described by Salvatore et al. (5.7% in children) [28]. In a Brazilian study, hepatobiliary disease was diagnosed in 16.4% of the patients, and it occurred as an initial manifestation of CF in 55.6% of these cases [29]. This variation in prevalence may be justified by the difference in the methods used for the diagnosis of liver disease associated with CF. In this study, it was not possible to perform the genetic study, therefore, it is not possible to evaluate if the observed prevalence was related to the genotype.
It is known that most CF patients will at some point present evidence of liver changes [30]. Currently, liver disease in CF is considered the third leading cause of death [31].
The prevalence of observed hepatomegaly (22.1%) is close to that reported in the literature (6–30%) [31]. However, the observed rate of neonatal cholestasis (11.7%) was different from the literature, where less than 2% of children with CF suffered from this condition [32]. An increase in liver enzymes (10.4%) within patients was observed. According to Flass and Narkewicz [33], the transient elevation of transaminases is often observed, often from idiopathic cause or due to antibiotics used to treat exacerbations, which undergo hepatic metabolism [33]. The occurrence of hepatic steatosis in this series (7.8%) differs from the prevalence of 23% to 67% reported in another study [30]. It is the most common liver lesion in patients with CF [33], and appears unrelated to the defect in the CFTR gene, but may be indirectly related to malnutrition, deficiency of essential fatty acids and oxidative stress, often occurring in these patients [31]. These factors may explain the low prevalence of hepatic steatosis, since most of the patients studied were eutrophic.
The prevalence of cholelithiasis in this study (6.5%) is reflective of the prevalence of 1% to 10% described in a revision study [31]. Of all the cases evaluated, 7.8% presented splenomegaly, 6.5% portal hypertension, 3.9% esophageal varicose veins, and 1.3% cirrhosis. It is questionable whether cirrhosis in CF is necessary for the development of portal hypertension, because according to Witters et al. [34], noncirrhotic portal hypertension (PH) can occur secondary to a vascular component. However, additional studies are needed to better elucidate this subject.
More than half of patients with hepatobiliary involvement were treated with UDCA, with a reduction in liver enzymes and improved echographic aspects in most cases. UDCA shows choleretic activity, reducing bile destruction, preventing bacterial translocation, and the development of endotoxin [30]. Thus, UDCA treatment has a beneficial effect on the activity of liver enzymes, in biliary drainage, hepatic histology, as well as in altering the profile of essential fatty acids [30].
Several research studies have been undertaken in the last decade to identify a non-invasive method for evaluating hepatic fibrosis, such as hepatic transient elastography (TE) [13]. In this study, fibrosis was observed in approximately 1/3 of the patients submitted for examination. The median (6.85 kPa) resembles the one (5.6 kPa) described by Witters et al. [35]. According to the literature, liver disease usually occurs after 10 years of disease evolution, and the fibrosis index is associated with the age of patients [13]. Similar to this study, measurements of hepatic rigidity in TE were significantly higher in the group manifesting clinical hepatic disease, altered liver biochemistry, as well as in the group with splenomegaly detected by ultrasound [35]. Thus, liver rigidity represents a viable non-invasive marker to detect CF, and to exclude PH.
This study found that the diagnosis of CF was earlier in the group with pancreatic insufficiency, when compared with the group diagnosed with pancreatic sufficiency (Table 4), possibly due to the manifestation of symptoms related to malabsorption syndrome of pancreatic insufficiency.
A reduction in the median age of diagnosis was observed after the implementation of the neonatal screening, similar to that described in REBRAFC 2014 [14] (Table 4). Although this study made descriptive analysis, the findings demonstrate the importance of extending the scope of neonatal screening for CF, with active investigation, in order to ensure early diagnosis and treatment to prevent damage.
In conclusion, the pulmonary phenotype was the most common, while the extrapulmonary manifestations were frequent and clinically relevant, and warrant early detection in the course of the disease followed by prompt treatment. Most patients, despite manifesting pancreatic insufficiency, revealed satisfactory nutritional status, demonstrating the effectiveness of treatment. The diagnosis was made earlier in patients with pancreatic insufficiency. The median age of diagnosis was reduced after the implementation of neonatal screening test by the public health service of the Federal District of Brazil, underscoring the significance of universal adoption of this test internationally.
Figures and Tables
Table 1
Nutritional Classification of Children and Adolescents with Cystic Fibrosis, according to Body Mass Index (BMI) and Stature

Table 2
Evaluation of Different Clinical Phenotypes of Children and Adolescents Diagnosed with Cystic Fibrosis

References
1. Kelly T, Buxbaum J. Gastrointestinal manifestations of cystic fibrosis. Dig Dis Sci. 2015; 60:1903–1913.

2. Gelfond D, Borowitz D. Gastrointestinal complications of cystic fibrosis. Clin Gastroenterol Hepatol. 2013; 11:333–342.

3. Carvalho E, Ferreira CT, Silva LR. Gastroenterologia e nutrição em pediatria. Barueri: Manole;2012.
4. Sathe MN, Freeman AJ. Gastrointestinal, pancreatic, and hepatobiliary manifestations of cystic fibrosis. Pediatr Clin North Am. 2016; 63:679–698.

5. Hurley MN, McKeever TM, Prayle AP, Fogarty AW, Smyth AR. Rate of improvement of CF life expectancy exceeds that of general population--observational death registration study. J Cyst Fibros. 2014; 13:410–415.

6. Farrell PM, Rosenstein BJ, White TB, Accurso FJ, Castellani C, Cutting GR, et al. Guidelines for diagnosis of cystic fibrosis in newborns through older adults: Cystic Fibrosis Foundation consensus report. J Pediatr. 2008; 153:S4–S14.

7. World Health Organization. The WHO child growth standards, 2006 [Internet]. Geneva: WHO;2006. cited 2017 Jan 31. Available from: http://www.who.int/childgrowth/en/.
8. Pereira CAC. Espirometria. J Pneumol. 2002; 28:Suppl 3. S1–S82.
9. Lee TW, Brownlee KG, Conway SP, Denton M, Littlewood JM. Evaluation of a new definition for chronic Pseudomonas aeruginosa infection in cystic fibrosis patients. J Cyst Fibros. 2003; 2:29–34.

10. Moran A, Brunzell C, Cohen RC, Katz M, Marshall BC, Onady G, et al. Clinical care guidelines for cystic fibrosis-related diabetes: a position statement of the American Diabetes Association and a clinical practice guideline of the Cystic Fibrosis Foundation, endorsed by the Pediatric Endocrine Society. Diabetes Care. 2010; 33:2697–2708.

11. Witt H, Apte MV, Keim V, Wilson JS. Chronic pancreatitis: challenges and advances in pathogenesis, genetics, diagnosis, and therapy. Gastroenterology. 2007; 132:1557–1573.

12. Vandenplas Y, Rudolph CD, Di Lorenzo C, Hassall E, Liptak G, Mazur L, et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J Pediatr Gastroenterol Nutr. 2009; 49:498–547.

13. Ciucă IM, Pop L, Tămaş L, Tăban S. Cystic fibrosis liver disease - from diagnosis to risk factors. Rom J Morphol Embryol. 2014; 55:91–95.
14. Registro Brasileiro de Fibrose cística [Internet]. São Paulo: Grupo Brasileiro de Estudos de Fibrose Cística;2014. cited 2017 Dec 10. Available from: http://portalgbefc.org.br/wp-content/uploads/2016/11/Registro2014_v09.pdf.
15. Cystic Fibrosis Foundation Patient Registry. 2012 annual data report to the center directors [Internet]. Bethesda: Cystic Fibrosis Foundation;2012. cited 2017 Jan 20. Available from: https://www.cff.org/.
16. Yadav K, Singh M, Angurana SK, Attri SV, Sharma G, Tageja M, et al. Evaluation of micronutrient profile of North Indian children with cystic fibrosis: a case-control study. Pediatr Res. 2014; 75:762–766.

17. Rizzo LC, Fischer GB, Maróstica PJ, Mocelin HT. Profile of cystic fibrosis in two reference centers in southern Brazil. Rev Assoc Med Bras (1992). 2015; 61:150–155.

18. Del Ciampo IR, Del Ciampo LA, Sawamura R, de Oliveira LR, Fernandes MI. Nutritional status of adolescents with cystic fibrosis treated at a reference center in the southeast region of Brazil. Ital J Pediatr. 2015; 41:51.

19. Goss CH, Muhlebach MS. Review: Staphylococcus aureus and MRSA in cystic fibrosis. J Cyst Fibros. 2011; 10:298–306.

22. Munck A, Alberti C, Colombo C, Kashirskaya N, Ellemunter H, Fotoulaki M, et al. International prospective study of distal intestinal obstruction syndrome in cystic fibrosis: Associated factors and outcome. J Cyst Fibros. 2016; 15:531–539.

23. Robinson NB, DiMango E. Prevalence of gastroesophageal reflux in cystic fibrosis and implications for lung disease. Ann Am Thorac Soc. 2014; 11:964–968.

24. Mousa HM, Woodley FW. Gastroesophageal reflux in cystic fibrosis: current understandings of mechanisms and management. Curr Gastroenterol Rep. 2012; 14:226–235.

25. Gorter RR, Karimi A, Sleeboom C, Kneepkens CM, Heij HA. Clinical and genetic characteristics of meconium ileus in newborns with and without cystic fibrosis. J Pediatr Gastroenterol Nutr. 2010; 50:569–572.

26. El-Chammas KI, Rumman N, Goh VL, Quintero D, Goday PS. Rectal prolapse and cystic fibrosis. J Pediatr Gastroenterol Nutr. 2015; 60:110–112.

27. Ramos AF, de Fuccio MB, Moretzsohn LD, Barbosa AJ, Passos Mdo C, Carvalho RS, et al. Cystic fibrosis, gastroduodenal inflammation, duodenal ulcer, and H. pylori infection: the "cystic fibrosis paradox" revisited. J Cyst Fibros. 2013; 12:377–383.

28. Salvatore D, Buzzetti R, Mastella G. Update of literature from cystic fibrosis registries 2012-2015. Part 6: Epidemiology, nutrition and complications. Pediatr Pulmonol. 2017; 52:390–398.

29. Nascimento FS, Sena NA, Ferreira TDA, Marques CDF, Silva LR, Souza EL. Hepatobiliary disease in children and adolescents with cystic fibrosis. J Pediatr (Rio J). 2017; DOI: 10.1016/j.jped.2017.07.006. [In press].

30. Leeuwen L, Fitzgerald DA, Gaskin KJ. Liver disease in cystic fibrosis. Paediatr Respir Rev. 2014; 15:69–74.

31. Kobelska-Dubiel N, Klincewicz B, Cichy W. Liver disease in cystic fibrosis. Prz Gastroenterol. 2014; 9:136–141.

32. Eminoglu TF, Polat E, Gökçe S, Ezgü FS, Senel S, Apaydin S. Cystic fibrosis presenting with neonatal cholestasis simulating biliary atresia in a patient with a novel mutation. Indian J Pediatr. 2013; 80:502–504.

33. Flass T, Narkewicz MR. Cirrhosis and other liver disease in cystic fibrosis. J Cyst Fibros. 2013; 12:116–124.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download