This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
The lower eyelid serves important roles in tear distribution and drainage. The purpose of this study was to measure the tear meniscus height (TMH) with anterior segment optical coherence tomography after lower blepharoplasty.
Methods
A total of 52 eyes from 26 patients treated between July 2012 and June 2015 were included in the study. A transcutaneous or transconjunctival approach was performed, depending on whether (1) the supportive lower lid orbicularis oculi muscle was tightened, (2) the middle lamella was elongated, (3) minimal fat was removed or transpositioned, and (4) lateral canthal support was established. Marginal reflex distance 2 and marginal nose distance were analyzed with Image J software. TMH was measured with anterior segment optical coherence tomography. A paired t-test and Wilcoxon signed-rank test were used for statistical comparisons.
Results
Marginal reflex distance 2 decreased and marginal nose distance increased with both surgical techniques. TMH decreased from 337.3 ± 117.9 to 289.3 ± 69.1 µm (p = 0.024) in patients who had transcutaneous lower blepharoplasty, but increased from 186.5 ± 35.5 to 274.8 ± 58.3 µm (p = 0.000) in patients who had transconjunctival lower blepharoplasty. Medial and lateral TMHs decreased significantly from 228.8 ± 80.7 to 152.7 ± 42.1 µm (p = 0.008) in patients with transcutaneous lower blepharoplasty. TMH was significantly restored after lower blepharoplasty with either approach.
Conclusions
Enhancing the lower eyelid position combined with orbicularis muscle tightening and lateral canthal support can normalize the TMH following lower eyelid blepharoplasty.
Go to :

Keywords: Blepharoplasty, Eyelids, Optical coherence tomography, Tears
An increasing number of patients want to alter the periorbital changes associated with aging. Clinical features of lower eyelid aging include protrusion of the lower eyelid fat pads, elongation of the tear trough, and redundancies at the inferior margin of the orbicularis muscle. The orbit appears to enlarge vertically as midface volumes descend and exert downward traction on the septum and arcus marginalis, exposing the tear trough and eventually the inferior orbital rim. Lower eyelid fat becomes prominent due to the loss of malar fat [
1].
The lower eyelid serves important roles in tear distribution and drainage. Blinking pushes tears along the eyelid margin, toward the punctum and lacrimal excretory system, which drains tears via a pump mechanism driven by the dynamics of the orbicularis muscle [
2].
Previous studies have reported tear problems after lower blepharoplasty. The incidence of dry eye after this procedure has been reported to range from 0% to 21.4% [
345]. Surgically modifying the lower eyelid can alter the lower eyelid position and eyelid blink force, and excising the orbicularis muscle may decrease blink rate, which promotes tear evaporation. These factors may produce dryness of the ocular surface [
56].
Optical coherence tomography (OCT) is a safe, cross-sectional imaging method that uses infrared radiation to capture high-resolution images of tissue microstructures [
7]. It is a noninvasive and objective tool to measure tear volume [
8910]. With this technique, the mean normal tear meniscus height (TMH) was previously reported to be 290.86 ± 62.20 µm at our institution [
11].
In the current study, anterior segment-OCT was used to measure changes in lower TMH after lower blepharoplasty in order to evaluate the effects of this procedure on tear fluid level.
Materials and Methods
This retrospective, observational case series comprised patients who underwent lower blepharoplasty at the Oculoplasty Service of Bungdang CHA Hospital, Seongnam, South Korea from July 2012 to June 2015. The case series consisted of 52 eyes (26 patients) without epiphora or eyelid malposition. This study was approved by the institutional review board of Bungdang CHA Hospital (CHAMC IRB 2017-08-053) and was performed in accordance with the tenets of the Declaration of Helsinki. Informed consent was obtained from all study participants.
Preoperative evaluations were performed on all subjects. Slit-lamp examinations were conducted to identify the punctual status and exclude any corneal disorders. Patient histories were reviewed to exclude dry eye syndrome and anterior segment disorders. Lower eyelid laxity was measured with the snap back test and categorized from 0 (absent) to 3 (very severe) [
12]. Fluorescein dye disappearance and lacrimal irrigation tests were performed to evaluate the lacrimal system. Exclusion criteria included eyelid malposition, combined surgery with upper blepharoplasty, and nasolacrimal duct obstruction with epiphora. The choice of treatment was made to ensure that (1) the supportive lower lid orbicularis oculi muscle was tightened, (2) the middle lamella was elongated, (3) minimal fat was removed or transpositioned, and (4) lateral canthal support was established.
Measurement of the lower TMH
All patients were tested between 10 a.m. and 5 p.m. The temperature and humidity of the test room were maintained at 23 ± 2℃ and 40 ± 5%, respectively. All measurements were performed by two experienced technicians. None of the subjects used eye drops 1 hour before testing to avoid eye drop effects. The patients blinked two or three times before images were captured to maintain consistency. Patients were asked to look straight ahead at a fixation light with no background illumination and were allowed to blink spontaneously during the examination. Each eye was examined; however, the contralateral eye remained open during image capture. A stable ambient room light was maintained during the examination. All patients were scheduled for examinations preoperatively, 1 week postoperatively, and at the last follow up.
For repeatability and reproducibility of the TMH measurements, 10 patients who did not undergo blepharoplasty and were not diagnosed with ophthalmologic disease underwent TMH measurement by two experienced technicians. Each patient had TMH measured by two examiners independently on the same day.
Three point measurements of TMH
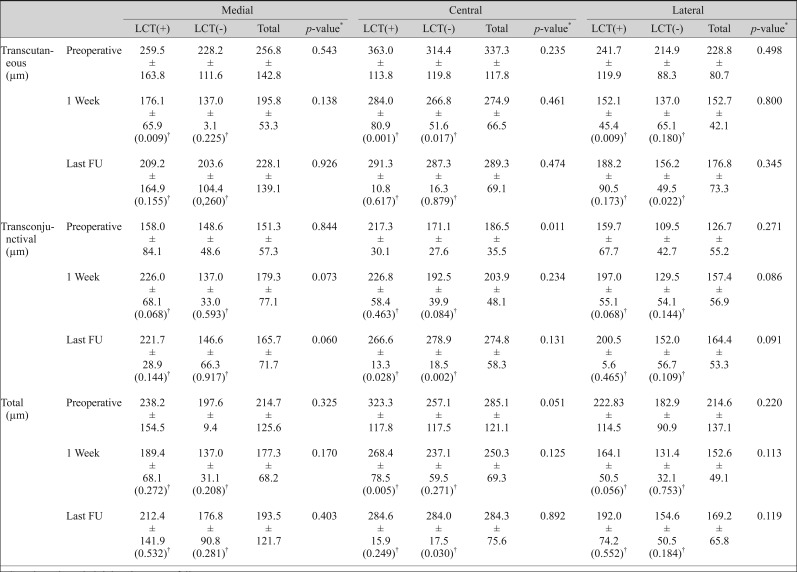
An anterior segment module, vertical raster, single-line, high-resolution scan was performed with a Spectralis OCT system (Heidelberg Engineering, Heidelberg, Germany). The scans were performed twice for each patient. All images were read by a single ophthalmology specialist. The OCT pattern used to scan the tear meniscus was a 6-mm vertical line centered at three points (medial, central, and lateral). The vertical axis of the corneal center was used as a central point that crossed the lower eyelid. The medial limbus was used for the medial point, and the lateral limbus was used for the lateral point. An optical coherence tomography, vertical line scan cross-sectional image of the tear meniscus was taken with spectral-domain OCT. TMH was measured from the cornea–meniscus junction to the lower eyelid-meniscus junction (
Fig. 1A–1D) [
11].
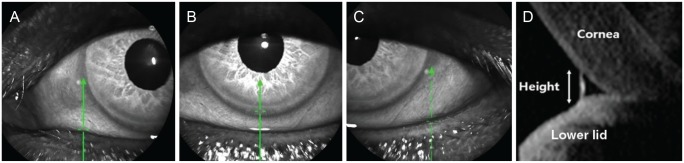 | Fig. 1Lower eyelid tear meniscus height was measured by anterior segment optical coherence tomography with a Spectralis optical coherence tomography. (A) Medial point, (B) central point, (C) lateral point, and (D) cross-sectional view. Green arrows indicate the vertical line centered at three points (medial, central, and lateral).
|
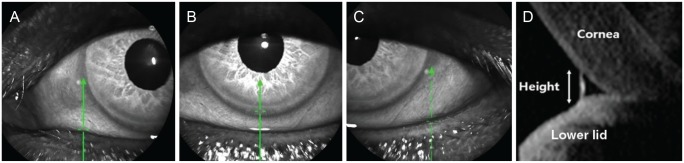
Measurement of lower eyelid position
The marginal reflex distance 2 (MRD
2) and marginal nose distance (MND) were analyzed with Image J software (National Institutes of Health, Bethesda, MD, USA) (
Fig. 2). Informed consent was obtained from all study participants before taking photos. The MRD
2 is the distance between the center of the pupil and lower eyelid margin, and MND is the distance between the lower eyelid margin and horizontal extension line of the nose tip. All patients were scheduled for photographs preoperatively, 1 week postoperatively, and at the last follow-up.
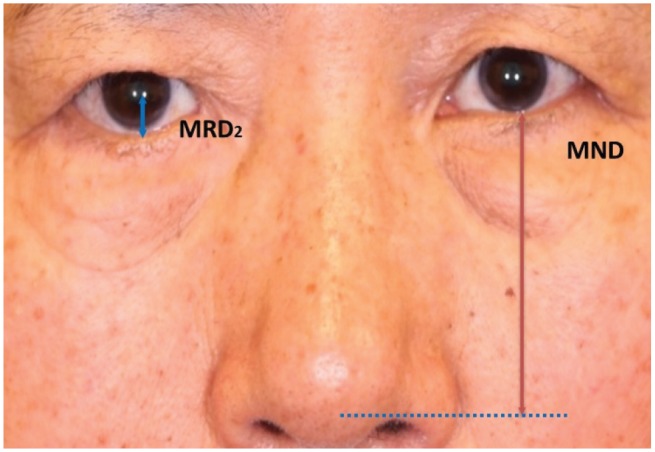 | Fig. 2Measurement of clinical parameters of lower eyelid position. Marginal reflex distance 2 (MRD2) and marginal nose distance (MND) were analyzed with ImageJ software.
|
Assessment of subjective symptoms related to tearing
Patient symptoms were retrospectively assessed on a scale of −2 to 2 based on the last follow-up. A grade of −2 indicated severe dryness with severe gritty symptoms that required artificial tear drops, a grade of −1 indicated mild dryness with only gritty symptoms, a grade of 0 indicated no symptoms, a grade of 1 indicated mild tearing only during windy conditions, and a grade of 2 indicated constant tearing even indoors.
Surgical techniques
All patients underwent lower blepharoplasty by a single surgeon. When planning the lower blepharoplasty, the TMH was measured before surgery, and the surgeon selected a transcutaneous or tranconjunctival approach based on TMH and tearing results.
1) Transcutaneous approach
After local anesthesia with 2% lidocaine and 1 : 100,000 epinephrine, a skin incision was created 1 mm below the lower eyelid margin. The skin and orbicularis muscle flap were dissected inferior to the orbital margin (
Fig. 3A). The orbital septum was then incised, and protruding orbital fat was removed (
Fig. 3B–3F). The surgical procedure was used to correct horizontal lid laxity for 14 eyelids. Orbicularis muscle tightening and lateral canthopexy were performed in patients with grade 1 laxity (n = 2) (
Fig. 3G), lateral canthal suspension was performed in patients with grade 2 laxity (n = 10) (
Fig. 3H), and lateral tarsal strip surgery was performed in patients with grade 3 laxity (n = 2) (
Fig. 3I). A medial spindle excision procedure was performed in patients with severe medial lower lid laxity.
 | Fig. 3Surgical procedures used in lower blepharoplasty. (A–C) The transcutaneous approach. (A) An incision was made 1 mm below the lower eyelid margin, (B) followed by incision of the orbital septum, and (C) removal of orbital fat. (D–F) The transconjunctival approach. (D) An incision was made at the conjunctiva 3 to 4 mm below the tarsal plate, (E) followed by an incision at the orbital septum, and (F) removal of orbital fat. (G–I) Lateral canthal tightening procedures, (G) orbicularis muscle tightening and lateral canthopexy, (H) lateral canthal suspension, and (I) lateral tarsal strip.
|
2) Transconjunctival approach
Lidocaine (2%) with 1:100,000 epinephrine was injected into the palpebral conjunctiva. After everting the lower eyelid, a conjunctival incision was made 3 to 4 mm below the tarsal plate (
Fig. 3D). An incision to the orbital septum was made, and orbital fat was removed through the opening (
Fig. 3E, 3F). This surgical procedure was used to correct the horizontal lid laxity for six eyelids. Orbicularis muscle tightening and lateral canthopexy were performed in patients with grade 1 laxity (n = 2), lateral canthal suspension for patients with grade 2 laxity (n = 2), and a lateral tarsal strip for patients with grade 3 laxity (n = 2). A medial spindle excision procedure was performed in patients with severe medial lower eyelid laxity.
Statistical analyses
All data are expressed as mean ± standard deviation. Parameters were compared with paired t-tests and Wilcoxon signed-rank tests. IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA) was used for all statistical analyses. A level of p < 0.05 was considered statistically significant. Intraclass correlation analyses were used to verify the reliabilities of the examinations.
Go to :

Results
Demographic characteristics of the patients
This study included 52 eyes of 26 consecutive patients who underwent lower blepharoplasty. Seventeen patients (65.3%) were female. The mean age at the time of surgery was 62.2 ± 13.1 years. The mean follow-up period after lower blepharoplasty was 10.2 ± 4.5 weeks. Lower blepharoplasty was performed through a transcutaneous approach for 34 eyes from 17 patients and through a transconjunctival approach for 18 eyes from nine patients.
Repeatability and reproducibility of the TMH measurements
Intraclass correlation analyses were performed for 10 eyes to verify the examination repeatability and reliability between the two technicians. The correlation coefficients ranged from 0.889 to 0.951.
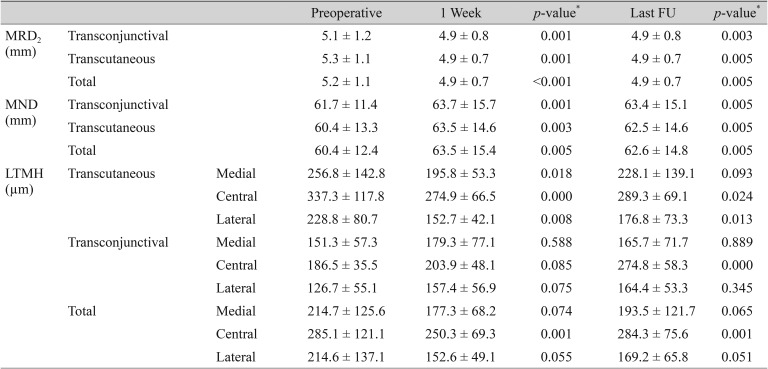
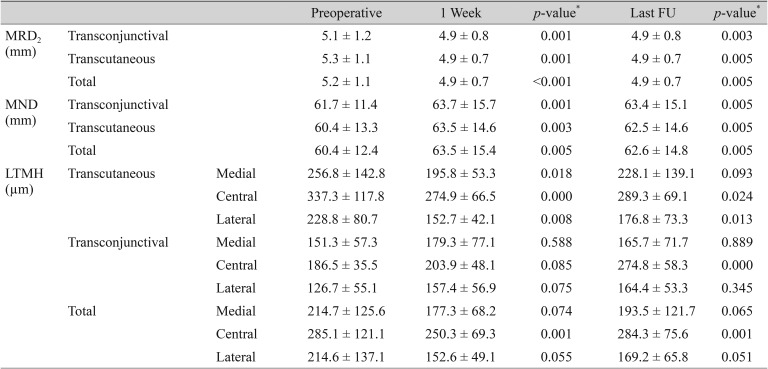
Measurement of eyelid position
Eyelid position changed significantly after surgery. MRD
2 (5.13 ± 1.21 mm for a transconjunctival approach and 5.29 ± 1.12 mm for a transcutaneous approach) decreased significantly at 1 week after surgery (4.89 ± 0.81 mm for a transconjunctival approach and 4.97 ± 0.69 mm for a transcutaneous approach) (
p = 0.001 and
p = 0.001, respectively) and was maintained at the last follow-up (4.90 ± 0.79 mm for a transconjunctival approach and 4.95 ± 0.71 mm for a transcutaneous approach) (
p = 0.003 and
p = 0.005, respectively). The MND (61.71 ± 11.35 mm for a transconjunctival approach and 60.37 ± 13.27 mm for a transcutaneous approach) increased significantly at 1 week after surgery (63.73 ± 15.71 mm for a transconjunctival approach and 63.49 ± 14.63 mm for a transcutaneous approach) (
p = 0.001 and
p = 0.003, respectively) and at the last follow-up (63.41 ± 15.09 mm for a transconjunctival approach and 62.50 ± 14.65 mm for a transcutaneous approach) (
p = 0.005 and
p = 0.005, respectively). In summary, MRD
2 and MND changed significantly with both approaches (
Table 1).
Table 1
Eyelid position and lower tear meniscus heights after lower blepharoplasty

Subjective symptoms
The subjective symptom score was −0.3 ± 0.8 for patients with a transcutaneous approach, 0.4 ± 0.7 for patients with a transconjunctival approach, and 0.5 ± 1.2 for all patients. Tearing scores were associated with changes in TMH following lower blepharoplasty. Overall, most patients had a score within +1 or −1, indicating that patient eyes were neither dry nor tearing after lower blepharoplasty.
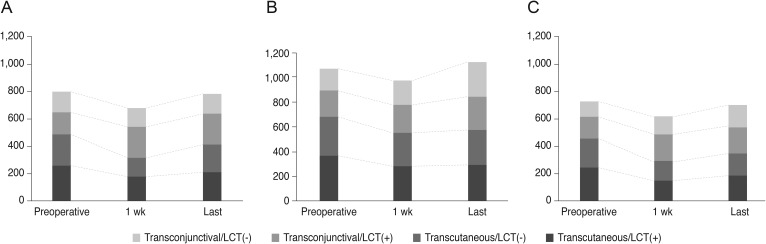
Changes in lower TMH
After transcutaneous lower blepharoplasty, the mean preoperative TMH at the central point (337.3 ± 117.8 µm) was decreased at 1 week after surgery (274.9 ± 66.5 µm,
p = 0.000) and at the last follow-up (289.3 ± 13.9 µm,
p = 0.024) (
Fig. 4A and
Table 1). The mean preoperative TMH at the medial point (256.8 ± 142.8 µm) was significantly decreased at 1 week after surgery (195.8 ± 53.3 µm,
p = 0.018). The mean preoperative TMH at the lateral point (228.8 ± 80.7 µm) was significantly decreased at 1 week after surgery (152.7 ± 42.2 µm,
p = 0.008) and at last follow-up (176.8 ± 73.4 µm,
p = 0.013).
 | Fig. 4The changes of lower eyelid tear meniscus height after lower blepharoplasty. (A) Transcutaneous approach (n = 34, Wilcoxon signed-rank test; *p < 0.05), (B) transconjunctival approach (n = 18, Wilcoxon signed-rank test; *p < 0.05), (C) total patients (Wilcoxon signed-rank test, *p < 0.05).
|
In patients treated with a transconjunctival approach, the mean preoperative TMH (186.5 ± 35.5 µm) was increased, though not significantly, at 1 week after surgery (203.9 ± 48.1 µm,
p = 0.085; Wilcoxon signed-rank test) and was significantly increased at the last follow-up (274.8 ± 15.6 µm,
p = 0.000; Wilcoxon signed-rank test) (
Fig. 4B and
Table 1).
The mean preoperative TMH at the central point (285.11 ± 121.05 µm) was significantly decreased at 1 week after surgery (250.3 ± 69.2 µm,
p = 0.001; Wilcoxon signed-rank test) and recovered at the last follow-up (284.3 ± 16.7
p = 0.001; Wilcoxon signed rank test) (
Fig. 4C and
Table 1). The mean preoperative TMH at the medial point (214.7 ± 125.6 µm) was significantly reduced at 1 week after blepharoplasty (177.3 ± 68.3 µm,
p = 0.044; Wilcoxon signed-rank test). The mean preoperative TMH at the lateral point (214.6 ± 137.0 µm) was significantly reduced at the last follow-up (169.3 ± 65.8 µm,
p = 0.044; Wilcoxon signed rank test).
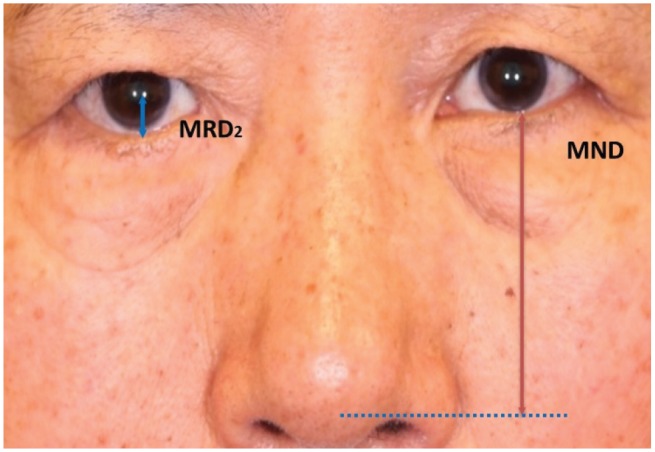
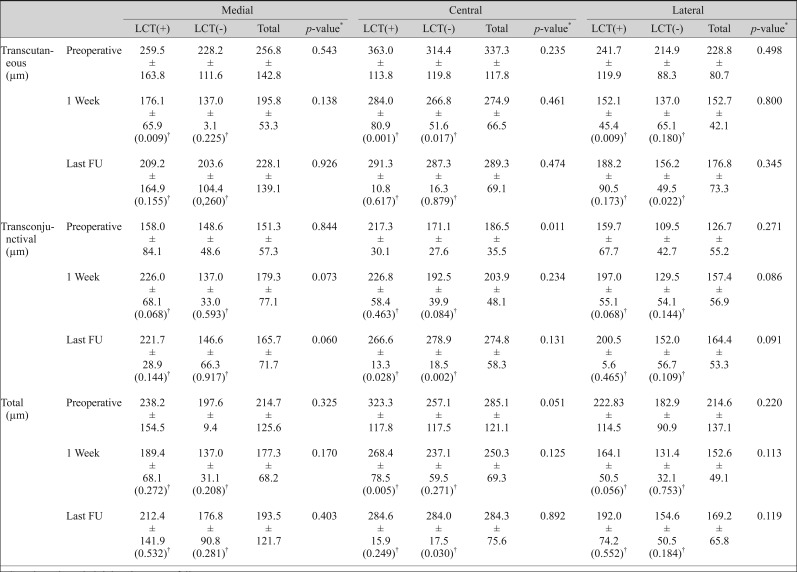
Lower eyelid TMH did not change significantly after a lateral canthal tightening procedure. Preoperative TMH at the central point was significantly higher in patients treated with a lateral canthal tightening procedure through a transconjunctival approach (217.3 ± 30.1 vs. 171.1 ± 27.6 µm,
p = 0.011) (
Table 2 and
Fig. 5A–5C).
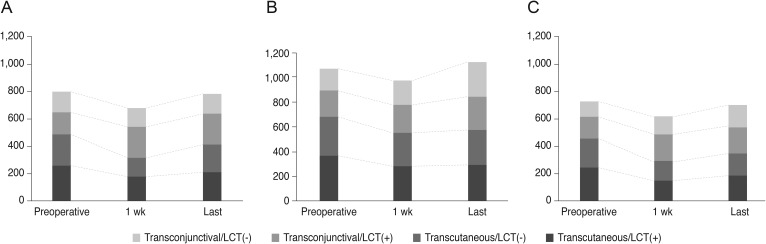 | Fig. 5Lower eyelid tear meniscus height at three points (A, medial; B, central; C, lateral) after lower blepharoplasty with all lateral canthal tightening (LCT) procedures.
|
Table 2
Lower eyelid tear meniscus height after lower blepharoplasty with and without lateral canthal tightening

Go to :

Discussion
Eyelid position after lower eyelid surgery is a source of debate. Taban et al. [
13] reported that the change in lower eyelid position was not statistically significant after a transconjunctival lower blepharoplasty with or without a skin pinch. Sultan et al. [
14] reported that transcutaneous skin-muscle flap lower eyelid surgery increased the distance between the pupil and lower eyelid margin. Segal et al. [
15] reported that transconjunctival blepharoplasty with or without skin resurfacing did not induce lid retraction but elevated the lower lid in the majority of patients. Elevating the lower lid can reduce or eliminate inferior scleral show, providing further cosmetic advantage. In a study of Koreans, Sung et al. [
16] reported that MRD
2 decreased and MND increased after lower eyelid blepharoplasty. In the present study, lower eyelid position likely changed MRD
2 and MND because horizontal eyelid laxity was corrected in 20 of 52 eyes with concurrent lower blepharoplasty.
The usefulness and reproducibility of TMH measurements using OCT have been confirmed in previous studies [
1117]. Previous studies reported normal TMH values that ranged from 194 to 345 µm [
11181920212223]. The mean normal TMH at our institution was 290.86 ± 62.20 µm [
11].
The present study reports quantitative changes in tear volumes after lower blepharoplasty. The TMH decreased immediately after surgery, then recovered by the last follow-up. Dry eye is a common complication after lower blepharoplasty, with an incidence from 0% to 24% [
345]. Surgically modifying the lower eyelid can alter the lower eyelid position and eyelid blink force. Lower blepharoplasty may also injure innervations of the orbicularis muscle, which could affect the blink rate and promote evaporative tear loss [
5]. These changes can result in dry eye after lower blepharoplasty.
The TMH results differed for the two surgical approaches. The TMH increased with a transconjunctival approach and decreased with a transcutaneous approach. In the early postoperative period, we presumed that a transcutaneous approach excised the orbicularis muscle and weakened the lacrimal pump function, while a transconjunctival approach induced conjunctival irritation and conjunctival chemosis, resulting in tear hypersecretion. However, the mean TMH at 3 months after surgery was similar to normal TMH values for both approaches. The surgical procedures in this study were performed through different approaches. Correction of lower eyelid laxity depended on its severity. Improving lower eyelid laxity and recovery of dynamic blinking are thought to cause efficient tear distribution and drainage. Changes in the TMH were observed at three points in patients treated with a transcutaneous approach, but only at the central point for patients treated with a transconjunctival approach. The results suggest that a more extensive change in periorbital anatomy with a transcutaneous approach changed tear level at all points in the lower eyelid.
We also evaluated the TMH at the medial and lateral points of the lower eyelid. The medial and lateral TMH changed significantly only in patients treated with transcutaneous lower blepharoplasty. We investigated TMH restoration according to the presence of a lateral canthal tightening procedure and showed that TMH was restored regardless of this procedure. The results suggest that the most suitable technique was sufficient to improve the TMH. Previous studies by Shao et al. [
6] reported that transcutaneous lower blepharoplasty affected the ocular surface and tear fluid, leading to dryness, teary eyes, and chemosis, and the symptoms resolved within 3 months. Unlike our study, TMH did not differ statistically before and three months after surgery. However, that study had some differences from the present study. The authors only studied the transcutaneous approach and did not consider eyelid laxity when planning the lower blepharoplasty procedure. In addition, the TMH was only measured at the central point. The patients were younger (50.53 ± 4.80 years) than in our study (62.2 ± 13.1 years), and the postoperative follow-up was 3 months in that study compared to 10.2 ± 4.5 weeks in the present study.
The retrospective review of lower blepharoplasty was a limitation of the present study. We, therefore, could not directly determine the effects of each surgical technique on tear volume changes. Because of the retrospective design, the preoperative TMH differed between groups. Future prospective studies with larger sample sizes and longer follow-up periods may help to determine the relationship between blepharoplasty approach and TMH. Also, postoperative TMH was only evaluated in two dimensions in our present study. Future prospective studies with 3-dimensional dynamic analysis may help to identify the relationship between blepharoplasty and tear film stability. Despite this limitation, we think that a customized lower blepharoplasty approach is effective in improving the ocular surface. Although we tried to exclude patients with dry eye disease, we did not examine all patients for this disorder. In addition, although we measured tear volume changes after lower blepharoplasty, tear film stability may have been associated with other factors. For example, evaluating blink response is also important in characterizing orbicularis muscle function after lower blepharoplasty.
In conclusion, transcutaneous or transconjunctival lower blepharoplasty, depending on patient characteristics, is effective in normalizing TMH and improving cosmetic outcomes. Therefore, eyelid laxity and the tear film should be evaluated before lower blepharoplasty, and tear film properties should be considered when planning surgery.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download