Abstract
Background and Purpose
The number of disease-modifying drugs (DMDs) available for treating relapsing-remitting multiple sclerosis is increasing. Numerous drugs have been approved since 2010 in South America, which has increased the complexity of the treatment algorithm. The aim of this study was to determine the changes in multiple sclerosis treatments relative to the underlying causes and the availability of new DMDs in Argentina.
Methods
A descriptive retrospective study was carried out on a group of 59 patients diagnosed with RRMS who use more than one DMD.
Results
The first treatment switch occurred before 2010 in 27% of the patients and after 2010 in the other 73%. Efficacy was the main reason for switching during both periods. A second treatment switch was required in 25% of the patients, with this occurring after 2010 in 86.6% of them. Interferon was the most-used drug before 2010 and fingolimod was the most-used drug thereafter.
Multiple sclerosis (MS) is a chronic demyelinating disease of the central nervous system. It is considered to be a T-cell-mediated autoimmune disorder that generates an inflammatory process in a cascade that compromises the oligodendrocytes and microglia, causing destruction of the myelin sheath and axonal injury. MS is characterized by demyelination, gliosis, axonal injury, and neuronal loss. Neurodegeneration that affects both white matter and gray matter is observed from the onset of the disease.123 This complex physiopathogeny, where inflammatory and degenerative processes are combined in different degrees of predominance, results in a variable and unpredictable evolutionary course. In most patients, MS initially presents episodes of reversible neurological deficit, which with the passing of time can lead to progressive and nonreversible neurological impairment.4 Patients can show increasing motor disability during the course of the disease, with half of cases showing severe mobility compromise at 15 years from disease onset that strongly affects their quality of life.5
Corticosteroids were used in the 1960s to diminish the severity of MS relapses, but they failed to reduce the number of annual relapses or the progression rate of the disease. Different immunosuppressant drugs were studied in the 1970s and 1980s, such as cyclophosphamide, cyclosporin, methotrexate, and azathioprine, and trials were carried out with glatiramer acetate.67 The first study of interferon beta 1b (IFNβ-1b) was reported on in 1993,8 and this was the first drug that was effective in reducing disability and the number of relapses.
IFNβ-1b became available for clinical use in South America in 1996, and this changed the paradigm of MS treatment in our region. The number of disease-modifying drugs (DMDs) available for treating relapsing-remitting multiple sclerosis (RRMS) has doubled worldwide in recent years. Numerous drugs for treating RRMS have been approved since 2010 in South America, and they vary in terms of administration method, dosing, action mechanism, efficacy, safety, and tolerability (Table 1). This increase in the available therapeutic options has made treatment algorithms more complex.
The aim of this study was to determine the changes in MS treatments relative to the underlying causes and the availability of new DMDs in Argentina.
A descriptive retrospective study was carried out on a group of patients who had received treatment in the Neurology Department of Dr. J. M. Ramos Mejía Hospital, Buenos Aires, Argentina, between 1994 and 2016. The inclusion criteria were a diagnosis of RRMS according to the 2010 McDonald criteria,9 use of more than one DMD, and having attended a clinical consultation within the past 2 years. This study was approved by the J. M. Ramos Mejia Hospital Bioethical Committee (approval date: November 1, 2017).
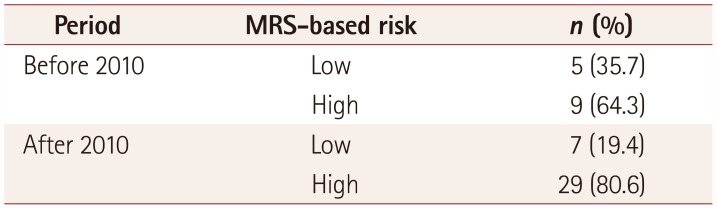
The following patient data were registered: sex, age, DMDs used at the beginning of the disease, changes in treatment, and reasons for these changes (drug tolerance problems, lack of adherence, or therapeutic failures such as loss of efficacy). Therapeutic failure was defined according to the modified Rio score (MRS).10 The MRS is a rating system consisting of a combination of clinical and magnetic resonance imaging (MRI) data that is used to predict those patients who may show a suboptimal response to treatment and be at a greater risk of disease progression or relapse. Patients with an MRS of 1 or more were considered as therapeutic failure. We divided the presents into two groups according to the MRS: those with an MRS of 0 or 1 were considered low risk, and those with an MRS of 2 or 3 were considered high risk.
The analysis was performed while considering when approval was granted for new therapies in Argentina, and hence two time periods were selected: before and after 2010.
Data were analyzed using the SPSS version 21.0 statistical program (IBM Corp., Armonk, NY, USA). The following statistical descriptors were used: frequency, percentage, range, and mean±standard-deviation values. The paired-samples t-test was used to detect statistically significant differences, which were considered to be present when p<0.05.
The inclusion criteria were satisfied by 59 of 260 analyzed patients. The group comprised 70% women, and the mean age at diagnosis was 27 years (range=9–51 years). During both time periods (i.e., before and after 2010), the most frequent treatment at the beginning of the disease was subcutaneous IFNβ-1a (Table 2).
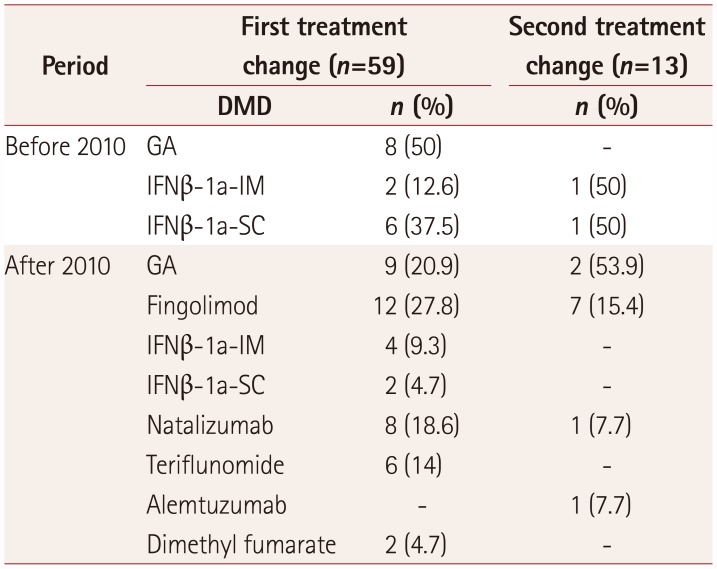
The first treatment switch occurred before 2010 in 27% of the 59 patients, with glatiramer acetate being the most widely selected drug. In the remaining 73% of patients who first switched treatment after 2010, fingolimod was the first choice followed by natalizumab (Table 3).
The main cause for switching treatment in both time periods was loss of efficacy (43% before and 62% after 2010), followed by tolerance problems (31% and 28%, respectively) and lack of adherence (23% and 9%). When drugs were analyzed in terms of the reasons for the first treatment switch, if the cause of the change was therapeutic failure, the drugs that were selected instead were IFNβ (5 patients) before 2010 and fingolimod (10 patients) and natalizumab (8 patients) after 2010. When the reasons motivating the switch of treatment were tolerance problems and lack of adherence, the most widely selected drugs were instead glatiramer acetate (6 patients) before 2010 and teriflunomide (6 patients) after 2010.
Most of the patients with therapeutic failure had an MRS indicating a high risk of new relapses or disease progression before the first change of treatment, and in most of them the score was 3 points (Table 4).
A second change of treatment was needed in 25% of the patients, with 13.4% of these cases making the second switch before 2010, selecting IFNβ-1a and IFNβ-1b as the main choices. The other 86.6% who switched after 2010 selected fingolimod as the main choice. Treatment changes were analyzed according to cause for the time period after 2010. When the reasons for changing were tolerance problems or lack of adherence, fingolimod, teriflunomide, and glatiramer acetate were the most widely selected drugs, while fingolimod was selected when the reason was therapeutic failure (Table 3).
The tendency among the patients who switched due to therapeutic failure was for a more effective treatment to be chosen (called scaling treatment). So-called horizontal changes to therapies considered to be similarly effective were applied to some of the patients, mostly before 2010. Only 1 patient switched to a drug of lower efficacy, from natalizumab to fingolimod (Table 2 and 3). The annualized relapse rate (ARR) in patients who switched due to therapeutic failure decreased significantly in this subgroup, from 0.97±1.14 to 0.18±0.31 (t=3.097, p=0.005). In patients who presented therapeutic failure after the first switch, the AAR was 0.18±0.34, and after the second switch it decreased to 0.14±0.20; however, this decrease was not statistically significant (t=1.279, p=0.233). In patients who presented with a low risk according to their MRS, the AAR was 0.465±0.410 prior to the first switch and 0.00±0.00 thereafter (t=2.200, p=0.115). In contrast, in those patients who presented with a high risk according to their MRS there was a significant reduction in ARR (t=0.283, p=0.010), from 1.065±1.210 to 0.27±0.34. Only patients who were switched to a more effective treatment (i.e., scaling treatment) exhibited a significant reduction in ARR (t=2.97, p=0.007).
The ever-expanding treatments for RRMS are becoming more sophisticated. The complex physiopathogeny of this disease has led to the development of molecules that exhibit substantial differences in their action mechanisms as well as in administration methods, dosage, efficacy, safety, and tolerability. Numerous DMDs have appeared on the market over the past decade. Following a worldwide tendency, new molecules for RRMS treatment were introduced in Argentina from 2010. Although all of these new drugs represent important advances in the treatment of MS, their efficacy, tolerance, and adherence remain unclear, and their adverse effects vary. It also has to be taken into account that individualized treatments are lacking, which makes it difficult to determine the most appropriate drugs for individual patients. These factors together hamper decision-making when initiating or changing treatment.
There can be many reasons for justifying switching from one drug to another. When considering efficacy from the viewpoint of disease physiopathogeny, DMDs have different action mechanisms, and the highly heterogeneous nature of MS and the lack of a biological marker make it difficult to predict which drug will be optimal in a specific patient.11 It also has to be considered that 30% of patients may show suboptimal responses during the first years of treatment,1213 and there are different studies claiming that the annual rate of outbreaks and residual disability are related.14 Although some drugs exhibit greater efficacy, the available data are restricted by few prospective head-to-head trials having been performed. Moreover, there is a wide range of adverse effects with different levels of severity that may appear randomly in only certain patients, making it difficult to predict tolerability. Lastly, adherence can be a significant cause of treatment discontinuation.15
The therapeutic options were scarce prior to the appearance of the new drugs, and so only one-third of the subjects evaluated in our study had switched treatment before 2010. This could have been due to the lack of therapeutic options and established criteria for switching, since the main drugs used until that time were IFNβ and glatiramer acetate. The main reasons for changing treatment were therapeutic failure or a suboptimal response to the medication. It was observed that the choice of a certain drug varied according to the reason for changing treatment: when the reason was therapeutic failure, the most frequently selected drugs were IFNβ before 2010 and fingolimod and natalizumab after 2010. This analysis was performed using the MRS, and most of the patients were at a high risk at the time of switching DMDs, which further justified the changes.
We observed a decrease in the ARR in patients who switched treatment due to therapeutic failure, with it being significantly higher in patients with a high MRS. Since the high-MRS patients benefited, careful monitoring for treatment failure and active treatment change should be considered in this population.16 There are scales other than MRS for defining “therapeutic failure” and serving as a guide to assess changes in treatment. Recommendations specific to Argentineans for identifying treatment failure in RRMS patients were published recently.17 That guide does not use the MRS for defining therapeutic failure and provides recommendations for optimizing the management of patients with MS in Argentina. In relation to other authors,18 our study showed greater reduction in the ARR among those patients who received a scaling treatment compared to those who received a horizontal change in treatment. In Carrá et al.18 reported on an Argentinean study of changes in treatment among patients who had experienced immunomodulatory therapy failure. Those authors analyzed switches from low-dose to high-dose IFN, from IFNβ to glatiramer acetate, and from glatiramer acetate to IFN. They found that patients who did not respond to first-line therapies benefited from switching to another immunomodulatory agent. Prosperini et al.19 carried out an observational study of 285 patients who had failed to respond to IFN or glatiramer-acetate therapy, and evaluated if the switch to natalizumab (a scaling treatment) was more effective than switching between first-line drugs (a horizontal change in treatment). They found no differences between the two groups at 12 months, but after 24 months a greater proportion of the patients in the scaling treatment group were free from relapse (p<0.0001), disability progression (p=0.0045), and MRI activity (p=0.0003). However, as mentioned above, it has to be considered that few head-to-head studies have compared the efficacy of one drug against another, and that none of these studies compared the so-called second-generation drugs.
The next most common switches were those motivated by tolerance problems and lack of adherence, which similar to previous findings.15 Nearly one-third of the present patients switched medication due to tolerance problems, and a smaller percentage did so due to loss of adherence. Previous studies have found that the percentage of patients switching differs if each drug is analyzed separately, and also when randomized clinical trials (RCTs) controlled against placebo are compared with observational studies.15 It must be remembered that strict inclusion criteria are applied in RCTs, with these studies usually comparing groups of patients who have been selected and monitored very carefully. The patients encountered in daily clinical practices are more heterogeneous, which makes it difficult to extrapolate data from RCTs to the general population.
Our analyses revealed a change in the treatment paradigm in patients with RRMS since 2010, which is probably due to the increased availability of drugs with greater efficacy and the existence of established criteria.2021 This complex scenario could be related to the appearance of new DMDs that vary greatly in efficacy, safety, and tolerability. New DMDs that are currently in different stages of clinical development will probably be introduced in the near future for treating RRMS, which will further add to the complexity of the therapeutic options for these patients. Another remaining challenge is to develop individualized treatments based on clinical, radiological, and laboratory variables. Individual needs should be considered when treating each patient and for controlling the disease.
Notes
Conflicts of Interest: Ricardo Alonso has received honorary-speaker payments from Biogen and Gemzyme. María Bárbara Eizaguirre has received an honoraryspeaker payment from Novartis. Lucía Zavala declares that he has no conflict of interest. Cecilia Pita declares that he has no conflict of interest. Berenice Silva has received honorary-speaker payments from Novartis, Biogen, and Gemzyme. Orlando Garcea has received honorary-speaker payments from Teva, Novartis Biogen, and Gemzyme, and has received research grants from Teva and Novartis.
References
1. Calabresi PA. Diagnosis and management of multiple sclerosis. Am Fam Physician. 2004; 70:1935–1944. PMID: 15571060.
2. Fraussen J, Vrolix K, Martinez-Martinez P, Losen M, De Baets MH, Stinissen P, et al. B cell characterization and reactivity analysis in multiple sclerosis. Autoimmun Rev. 2009; 8:654–658. PMID: 19239929.

3. Frohman EM, Racke MK, Raine CS. Multiple sclerosis--the plaque and its pathogenesis. N Engl J Med. 2006; 354:942–955. PMID: 16510748.
4. Weinshenker BG. Epidemiology of multiple sclerosis. Neurol Clin. 1996; 14:291–308. PMID: 8827172.

5. Polman CH, Uitdehaag BM. Drug treatment of multiple sclerosis. BMJ. 2000; 321:490–494. PMID: 10948033.

6. Bornstein MB, Miller A, Slagle S, Weitzman M, Crystal H, Drexler E, et al. A pilot trial of Cop 1 in exacerbating-remitting multiple sclerosis. N Engl J Med. 1987; 317:408–414. PMID: 3302705.

7. Lublin F. History of modern multiple sclerosis therapy. J Neurol. 2005; 252(Suppl 3):iii3–iii9. PMID: 16170498.

8. The IFNB Multiple Sclerosis Study Group. Interferon beta-1b is effective in relapsing-remitting multiple sclerosis. I. Clinical results of a multicenter, randomized, double-blind, placebo-controlled trial. The IFNB Multiple Sclerosis Study Group. Neurology. 1993; 43:655–661. PMID: 8469318.
9. Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011; 69:292–302. PMID: 21387374.

10. Río J, Castilló J, Rovira A, Tintoré M, Sastre-Garriga J, Horga A, et al. Measures in the first year of therapy predict the response to interferon beta in MS. Mult Scler. 2009; 15:848–853. PMID: 19542263.
11. Coyle PK. Switching therapies in multiple sclerosis. CNS Drugs. 2013; 27:239–247. PMID: 23508518.

12. Coyle PK. Switching algorithms: from one immunomodulatory agent to another. J Neurol. 2008; 255(Suppl 1):44–50. PMID: 18317676.

13. Río J, Tintoré M, Sastre-Garriga J, Nos C, Castilló J, Tur C, et al. Change in the clinical activity of multiple sclerosis after treatment switch for suboptimal response. Eur J Neurol. 2012; 19:899–904. PMID: 22289050.

14. Lublin FD, Baier M, Cutter G. Effect of relapses on development of residual deficit in multiple sclerosis. Neurology. 2003; 61:1528–1532. PMID: 14663037.

15. Giovannoni G, Southam E, Waubant E. Systematic review of disease-modifying therapies to assess unmet needs in multiple sclerosis: tolerability and adherence. Mult Scler. 2012; 18:932–946. PMID: 22249762.

16. Rio J, Rovira A, Blanco Y, Sainz A, Perkal H, Robles R, et al. [Response to treatment with interferon beta in patients with multiple sclerosis. Validation of the Rio Score]. Rev Neurol. 2016; 63:145–150. PMID: 27439483.
17. Cristiano E, Alonso R, Alvez Pinheiro A, Bacile EA, Balbuena ME, Ballario C, et al. Argentinean recommendations on the identification of treatment failure in relapsing remitting multiple sclerosis patients. J Neurol Sci. 2018; 385:217–224. PMID: 29406907.

18. Carrá A, Onaha P, Luetic G, Burgos M, Crespo E, Deri N, et al. Therapeutic outcome 3 years after switching of immunomodulatory therapies in patients with relapsing-remitting multiple sclerosis in Argentina. Eur J Neurol. 2008; 15:386–393. PMID: 18353125.
19. Prosperini L, Giannì C, Leonardi L, De Giglio L, Borriello G, Galgani S, et al. Escalation to natalizumab or switching among immunomodulators in relapsing multiple sclerosis. Mult Scler. 2012; 18:64–71. PMID: 21828195.

20. Ziemssen T, De Stefano N, Sormani MP, Van Wijmeersch B, Wiendl H, Kieseier BC. Optimizing therapy early in multiple sclerosis: an evidence-based view. Mult Scler Relat Disord. 2015; 4:460–469. PMID: 26346796.

21. Freedman MS, Selchen D, Arnold DL, Prat A, Banwell B, Yeung M, et al. Treatment optimization in MS: Canadian MS Working Group updated recommendations. Can J Neurol Sci. 2013; 40:307–323. PMID: 23603165.

Table 1
Disease-modifying drugs available in argentina during the two analyzed time periods
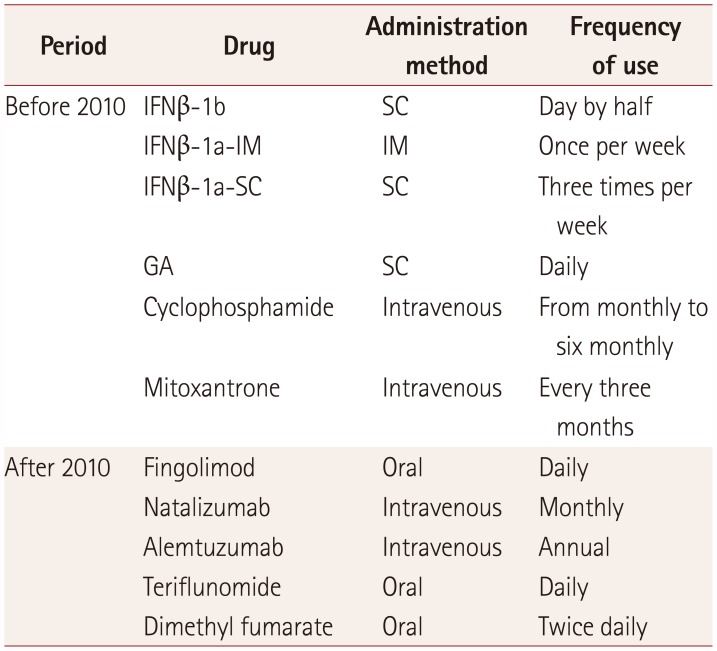
Table 2
Initial DMD according to time period
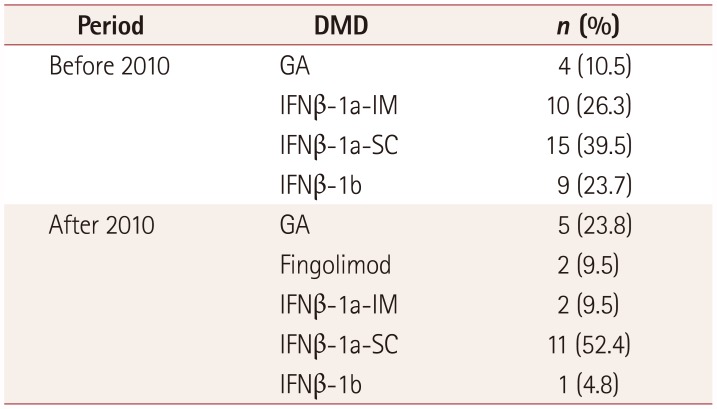
| Period | DMD | n (%) |
|---|---|---|
| Before 2010 | GA | 4 (10.5) |
| IFNβ-1a-IM | 10 (26.3) | |
| IFNβ-1a-SC | 15 (39.5) | |
| IFNβ-1b | 9 (23.7) | |
| After 2010 | GA | 5 (23.8) |
| Fingolimod | 2 (9.5) | |
| IFNβ-1a-IM | 2 (9.5) | |
| IFNβ-1a-SC | 11 (52.4) | |
| IFNβ-1b | 1 (4.8) |
Table 3
DMDs used in the first and second treatment changes according to time period




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download