1. Zhang K, Bhatia S, Oh M, Whiting D. Epidural anesthesia for placement of spinal cord stimulators with paddle-type electrodes. Stereotact Funct Neurosurg. 2009; 87:292–296. PMID:
19590261.

2. Vangeneugden J. Implantation of surgical electrodes for spinal cord stimulation: classical midline laminotomy technique versus minimal invasive unilateral technique combined with spinal anaesthesia. Acta Neurochir Suppl. 2007; 97:111–114.

3. Skipsey IG, Colvin JR, Mackenzie N, Kenny GN. Sedation with propofol during surgery under local blockade. Assessment of a target-controlled infusion system. Anaesthesia. 1993; 48:210–213. PMID:
8460797.
4. Mingus ML, Monk TG, Gold MI, Jenkins W, Roland C. Remifentanil versus propofol as adjuncts to regional anesthesia. Remifentanil 3010 Study Group. J Clin Anesth. 1998; 10:46–53. PMID:
9526938.
5. Holsheimer J, Barolat G, Struijk JJ, He J. Significance of the spinal cord position in spinal cord stimulation. Acta Neurochir Suppl. 1995; 64:119–124. PMID:
8748598.

6. Holsheimef J, Barolat G. Spinal geometry and paresthesia coverage in spinal cord stimulation. Neuromodulation. 1998; 1:129–136. PMID:
22150980.

7. Bhananker SM, Posner KL, Cheney FW, Caplan RA, Lee LA, Domino KB. Injury and liability associated with monitored anesthesia care: a closed claims analysis. Anesthesiology. 2006; 104:228–234. PMID:
16436839.
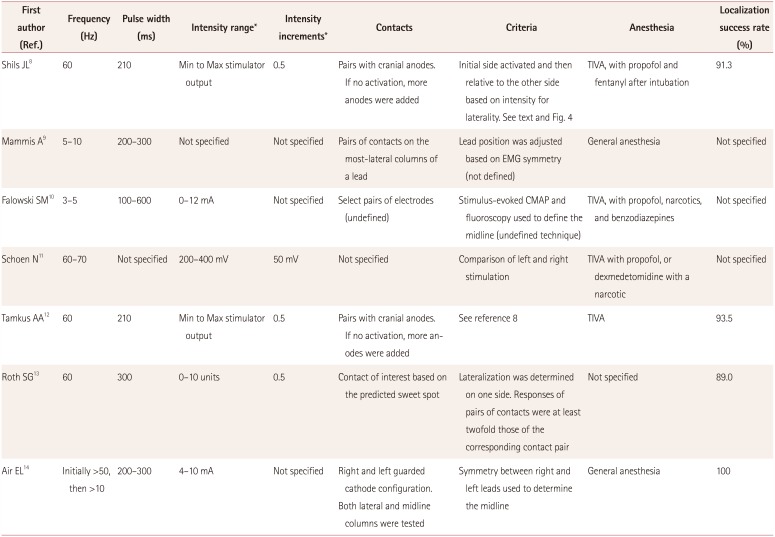
8. Shils JL, Arle JE. Intraoperative neurophysiologic methods for spinal cord stimulator placement under general anesthesia. Neuromodulation. 2012; 15:560–571. PMID:
22672099.

9. Mammis A, Mogilner AY. The use of intraoperative electrophysiology for the placement of spinal cord stimulator paddle leads under general anesthesia. Neurosurgery. 2012; 70:230–236. PMID:
21869720.

10. Falowski SM, Celii A, Sestokas AK, Schwartz DM, Matsumoto C, Sharan A. Awake vs. asleep placement of spinal cord stimulators: a cohort analysis of complications associated with placement. Neuromodulation. 2011; 14:130–134. PMID:
21992199.

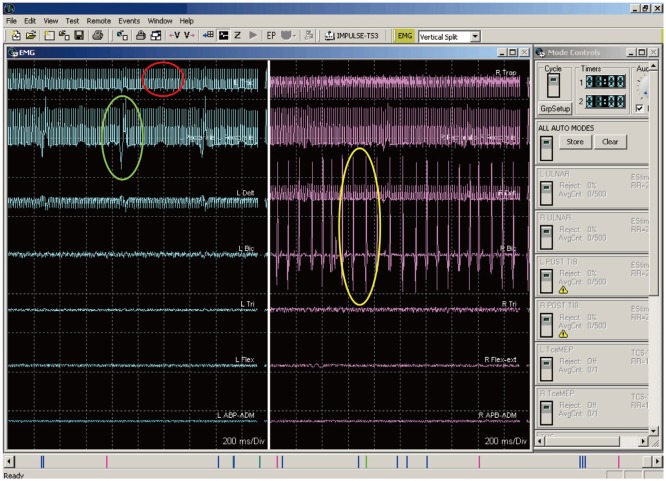
11. Schoen N, Chieng LO, Madhavan K, Jermakowicz WJ, Vanni S. The use of intraoperative electromyogram during spinal cord stimulator placement surgery: a case series. World Neurosurg. 2017; 100:74–84. PMID:
28034811.

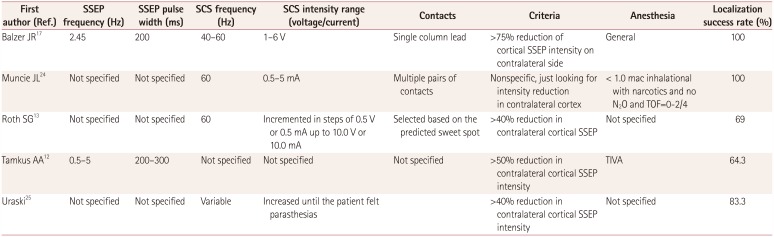
12. Tamkus AA, Scott AF, Khan FR. Neurophysiological monitoring during spinal cord stimulator placement surgery. Neuromodulation. 2015; 18:460–464. PMID:
25677059.

13. Roth SG, Lange S, Haller J, De La Cruz P, Kumar V, Wilock M, et al. A prospective study of the intra- and postoperative efficacy of intraoperative neuromonitoring in spinal cord stimulation. Stereotact Funct Neurosurg. 2015; 93:348–354. PMID:
26444517.

14. Air EL, Toczyl GR, Mandybur GT. Electrophysiologic monitoring for placement of laminectomy leads for spinal cord stimulation under general anesthesia. Neuromodulation. 2012; 15:573–579. PMID:
23205816.

15. Collison C, Prusik J, Paniccioli S, Briotte M, Grey R, Feustel P, et al. Prospective study of the use of intraoperative neuromonitoring in determining post-operative energy requirements and physiologic midline in spinal cord stimulation. Neuromodulation. 2017; 20:575–581. PMID:
28370852.
16. Davidoff RA. Handbook of the Spinal Cord: Anatomy and Physiology (Vols 2 and 3). New York, NY: Dekker Publishing;1984. p. 318.
17. Balzer JR, Tomycz ND, Crammond DJ, Habeych M, Thirumala PD, Urgo L, et al. Localization of cervical and cervicomedullary stimulation leads for pain treatment using median nerve somatosensory evoked potential collision testing. J Neurosurg. 2011; 114:200–205. PMID:
20509731.

18. Hunter JP, Ashby P. Segmental effects of epidural spinal cord stimulation in humans. J Physiol. 1994; 474:407–419. PMID:
8014902.

19. Schirmer CM, Shils JL, Arle JE, Cosgrove GR, Dempsey PK, Tarlov E, et al. Heuristic map of myotomal innervation in humans using direct intraoperative nerve root stimulation. J Neurosurg Spine. 2011; 15:64–70. PMID:
21476796.

20. Arle JE, Mei LZ, Carlson KE, Shils JL. Theoretical effect of DBS on axonal fibers of passage: firing rates, entropy, and information content. Stereotact Funct Neurosurg. 2018; 96:1–12. PMID:
29393267.

21. Yingling CD, Hosobuchi Y. Use of antidromic evoked potentials in placement of dorsal cord disc electrodes. Appl Neurophysiol. 1986; 49:36–41. PMID:
3490219.

22. Deletis V, Bueno De. Interventional neurophysiological mapping during spinal cord procedures. Stereotact Funct Neurosurg. 2001; 77:25–28. PMID:
12378052.

23. Falowski SM, Sharan A, McInerney J, Jacobs D, Venkatesan L, Agnesi F. Nonawake vs Awake Placement of Spinal Cord Stimulators: A Prospective, Multicenter Study Comparing Safety and Efficacy. Neurosurgery. 2018; 3. 14. [Epub] available from: . DOI:
10.1093/neuros/nyy062.

24. Muncie LM, Elens NR, Told-Kemp E, Feler CA, Winestone JS. Intraoperative electrophysiological monitoring for C1-2 spinal cord stimulation. J Neurosurg Spine. 2017; 26:183–189. PMID:
27689422.

25. Urasaki E, Tsuda M, Nakane S, Toyoda K, Umeno T, Yamakawa Y. Spinal cord stimulation for intractable pain evaluated by a collision study using somatosensory evoked potentials: a preliminary report. Neuromodulation. 2014; 17:746–752. PMID:
24945895.










 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download