This article has been
cited by other articles in ScienceCentral.
Abstract
Hiccup is an intermittent, involuntary and erratic contraction of the diaphragm, immediately followed by a laryngeal closure. Persistent and intractable hiccups are rare but severe, keeping a person from doing daily activities; these can result in depression, fatigue, impaired sleep, dehydration, weight loss, malnutrition, and aspiration. Therefore, proper treatments are necessary. We present a case with intractable hiccup treated with an unusual treatment. A 61-year-old man presented with intractable hiccups, which started 6 years ago after subarachnoid and intraventricular hemorrhage. Conventional pharmacologic treatments including metoclopramide, gabapentin, and baclofen were unsuccessful. Cooperating with cardiothoracic surgeons, phrenic nerve clipping operation was done under intraoperative electrophysiologic monitoring. This method was successful that the symptoms were relieved. Reversible clipping done under intraoperative electrophysiologic monitoring can be a promising therapeutic method for persistent and intractable hiccups in patients with stroke.
Keywords: Hiccup, Phrenic Nerve, Electromyography
INTRODUCTION
Simple hiccup is usually self-limiting. It consists of a sudden powerful activation of the inspiratory muscles of the thorax, diaphragm, neck accessory, and external intercostal muscles, followed by active movement of the tongue toward the roof of the mouth [
1]. Active adduction of the vocal cords follows the initiation of the inspiratory flow. In general, hiccups stop within 48 hours. If these continue for more than 48 hours and end within a month, these are known as persistent hiccups. If these last longer than 2 months, these conditions are considered as intractable hiccups [
2]. Persistent and intractable hiccups, which are uncommon, may prevent people from usual daily activities like sleeping and eating. This decline of quality of life can result in depression, fatigue, impaired sleep, dehydration, weight loss, malnutrition, and aspiration [
3].
To figure out the mechanism of the hiccup, a hiccup reflex arc should be understood. It is thought to be composed of three parts: an afferent limb including vagus, phrenic nerves, and sympathetic chain, a central midbrain modulation, and an efferent limb including phrenic and accessory nerves [
2]. Any disruption of the reflex arc can cause a hiccup, and numerous pathologic conditions can be causes. There are some serious conditions that can cause intractable hiccup including brain malignancies, cerebral vascular lesions, myocardial ischemia, herpes infection, and gastroesophageal reflux disease.
Unfortunately, there is no guideline available to treat these chronic hiccups effectively. Literature suggest that medications and methods such as nasopharyngeal catheter insertion, pharmacologic treatment, phrenic nerve blockade, and phrenic nerve stimulation may treat hiccup [
12]. Here is a case that was successfully improved with phrenic nerve clipping with intraoperative electrophysiologic monitoring in a patient with stroke.
CASE REPORT
A 61-year old man was admitted to the department of rehabilitation medicine at our hospital with quadriplegia. Six years ago, he suffered from subarachnoid hemorrhage and intraventricular hemorrhage with extra-ventricular drainage operation. He also underwent tracheostomy. Since that day, he had become quadriplegic and bedridden state. His past medical history had been unremarkable until the stroke occurred. Immediately after extra-ventricular drainage operation, he began to experience bouts of hiccups which lasted up to 13 hours. These occurred recurrently for 6 years while sleeping or staying awake. Once hiccups occurred, they lasted for more than 10 hours. Self-induced nausea and vomiting also coincided with hiccups for a while. To relieve his symptoms, he received metoclopramide, but there was no apparent improvement. Subsequently, he was treated with gabapentin (300 mg three times a day), which reduces the release of glutamate and substance P and modulates the diaphragmatic action [
4]. Several days later, drowsiness, common adverse effects of gabapentin, emerged, and his hiccups aggravated, appearing more frequently. Therefore, 5 mg of baclofen was given three times a day. Because his hiccups continued, he received the increased dosage of baclofen up to 10mg twice a day. However, he showed drowsiness and deep sedation at a higher dose. Baclofen has side effects such as nephrotoxicity, oversedation, ataxia, and confusion in elderly subjects and especially those with renal failure [
5].
We consulted cardiothoracic surgeons about his hiccup treatment, and they recommended phrenic nerve clipping because phrenic nerve ligation could cease hiccups as it blocked the efferent limb of the hiccups reflex [
6]. On fluoroscopic studies of the chest, there was concurrent left diaphragm involvement during the hiccups. After assessing the movement of the left hemidiaphragm, the left phrenic nerve clipping was chosen. Before the procedure, the initial chest radiograph showed no parenchymal lesion. Also, the arterial blood gas results showed within normal limit. In general anesthesia state, the cardiothoracic surgeons attached surface electrodes at 7th intercostal space for intraoperative electrophysiologic monitoring and made skin incision about 5cm at left supraclavicular fossa. The anterior wall of the spine and the scalene muscle was exposed, and the left phrenic nerve was isolated. After isolating left phrenic nerve, nerve stimulation was started directly. The electromyogram recorded compound muscle action potentials (CMAPs) of the left diaphragm (
Table 1). There were normal onset latencies and amplitudes of CMAPs in the left diaphragm, recorded from the left diaphragm before clipping. After the left phrenic nerve clipping, the amplitudes of CMAPs of the left diaphragm were approximately halved, which suggested conduction block around clipping site (
Fig. 1-A, 1-B). Also, the left diaphragm elevation was identified on chest radiograph suggesting the procedure was successful (
Fig. 2).
Table 1
Onset latencies and amplitudes of compound muscle action potentials of the left diaphragm before and after clipping in electromyography
|
Stimulation site |
Onset (ms) |
Peak (ms) |
Amplitude (mV) |
|
Left phrenic motor (7 intercostal-) before clipping |
|
|
|
|
Left phrenic nerve (isolated at supraclavicular area) |
8.5 |
21.1 |
0.4 |
|
Left phrenic motor (7 intercostal-) after clipping |
|
|
|
|
Left phrenic nerve (isolated at supraclavicular area) |
9.6 |
23.4 |
0.2 (0 min post) |
|
Left phrenic nerve (isolated at supraclavicular area) |
10.0 |
20.7 |
0.1 (5 min post) |

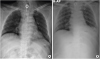
 | Fig. 1
(A) Normal ranges of onset latencies and amplitudes of CMAPs of the left diaphragm before clipping. (B) Decreased amplitudes of CMAPs after clipping.
(CMAP, compound muscle action potential; O, onset latency; P, peak latency; T, termination latency)

|
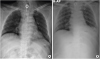
 | Fig. 2(A) Chest radiograph before clipping. (B) The left diaphragm was elevated after clipping. 
|
Because the patient had a tracheostomy and could not follow our orders, we could not perform pulmonary function test to evaluate pre- and post-procedural respiratory function. But laboratory findings after procedure including analysis of the arterial blood gas showed normal limits. Also, clinical feature and vital sign were stable. Before the procedure, hiccup occurred once every two or three days and continued more than 10 hours. After the procedure, however, his symptoms gradually improved over a month. During a month, the frequency of hiccup gradually declined to the half of the pre-procedural state. In addition, the interval between hiccups increased to 3 days, and the intensity of hiccup was also decreased. This improvement was sustained for a year after discharge.
DISCUSSION
There are various pathologic conditions that can cause hiccups. Whatever the cause is, the management of hiccup is still debated and even sometimes unsatisfactory. Both pharmacological or non-pharmacological treatments are available to treat hiccups. In various pathologic cases, medical treatment is usually chosen preferentially. Chlorpromazine is well-known treatment option which is approved to treat hiccups, but many other drugs have been tested and recommended [
1]. Gabapentin, an alpha-2-delta ligand which is similar to gamma-aminobutyric acid, blocks voltage-operated calcium channels to lessen release of several neurotransmitters including substance P and glutamate and finally modulates the diaphragmatic activity. Gabapentin is safe to treat intractable hiccups but can cause sleepiness [
47]. Baclofen, a gamma-aminobutyric acid derivative, is available to treat hiccup caused by central nervous system tumors and chronic renal failure. However, baclofen should be adopted very carefully when prescribed to elderly subjects and patients with renal failure because baclofen can cause nephrotoxicity, deep sedation, ataxia and confusion [
5]. Other miscellaneous agents used to treat hiccup include beta-blocker, calcium channel blocker, antioxidant, 5-hydroxytryptamine agonist, a serotonergic antagonist, and a benzodiazepine. If medical therapy is unsuccessful, many alternative treatments are available.
Non-pharmacological treatment of hiccups may include phrenic nerve blockades, diaphragmatic pacing and pulsed radiofrequency ablation of phrenic nerves. Ultrasound- guided blockades of efferent limbs of phrenic nerves were may be treatment options for persistent post-operative hiccups [
8]. Ultrasound-guided pulsed radiofrequency may be used to treat coronary by-pass surgery related hiccup [
6]. Acupuncture has been adopted to treat serious hiccups following myocardial infarction [
9]. Near-infrared irradiation to the acupoints may improve the local blood circulation of affected areas and may be an effective treatment for intractable hiccups [
10]. Our patient has been suffered from long-lasting hiccups, interfering with rehabilitation treatment and aggravating quality of life. Pharmacologic treatments with metoclopramide, gabapentin, and baclofen had no effect; instead, he had side effects such as drowsiness and deep sedation. To improve his condition and avoid side effects of medication, we considered non-pharmacological measures as an alternative treatment. The patient wanted a definite cure even though it was more invasive, so we recommended reversible phrenic nerve clipping that is removable when severe complication such as respiratory failure occurring under informed consent. Phrenic nerves are easily approached and isolated by cardiothoracic surgeons at the supraclavicular area. Furthermore, if complications such as dyspnea and hypoxia occur after phrenic nerve ligation, removal of phrenic nerve clipping is possible immediately. These alternative treatments have been applied to some limited cases. Further studies are required to evaluate the safety and efficacy of this procedure with more patients.
In conclusion, intractable hiccups can be extremely distressing, often significantly destroying the quality of life. Through this case report, we illustrated our experience in performing phrenic nerve clipping in a patient with stroke. We attempted to present the possible effectiveness of phrenic nerve clipping against the intractable hiccups which are not responsive to other types of treatments including Levin tube insertion, carotid sinus massage, and pharmacologic treatments. Because this surgical procedure can be applied to patients with normal pulmonary function, patients with respiratory diseases or other underlying conditions might need additional evaluation such as pulmonary function test. Last but not least, we demonstrate that further studies are needed to prove the safety and efficacy of the treatment because this procedure was the first attempt in Korea and unexpected complications can arise in the future.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download