This article has been
cited by other articles in ScienceCentral.
Abstract
Corticobasal syndrome (CBS) is characterized by asymmetric dystonia, and myoclonus accompanied by higher cortical features including apraxia, alien limb phenomena, cortical sensory loss. Here, we report treatment course of 3 CBS patients. Asymmetric dystonia was seen in the first and second cases, a cortical sensory loss was seen in the third case and left lower limb apraxia was common in all cases. In the first and second cases, we performed an alcohol block on the obturator nerve and injected botulinum toxin into the lower leg to reduce dystonia. In the third case, patient was treated with a robotic assisted gait training, whole body therapeutic pool and gait training with laser pointer visual cueing. After appropriate treatment for patients, all 3 cases showed improvement in gait.
Highlights
CBS is a disease with various clinical features such as limb apraxia.
After obturator nerve block and botulinum toxin injection in CBS patients with limb dystonia, the gait pattern improved.
In the CBS patients with limb apraxia, gait improved after whole body therapeutic pool and robotic assisted gait training.
Keywords: Gait Apraxia, Dystonia, Botulinum Toxins, Nerve Block, Neurological Rehabilitation
INTRODUCTION
Corticobasal degeneration (CBD) is a rare neurodegenerative disease characterized by asymmetric cortical atrophy mainly at the frontoparietal region, and by degeneration in the basal ganglia and nigral neurons. Its core clinical features reflect the pathology with a progressive asymmetric rigidity together with other clinical features denoting cortical affection (e.g., alien limb phenomenon, myoclonus, cortical sensory loss, and apraxia) and basal ganglionic circuits dysfunction (e.g., bradykinesia, tremor, and dystonia) [
1]. Moreover, the clinical syndrome and this distinctive pathology do not always coexist in all cases. So, the term CBD is reserved for pathologically confirmed cases, while the clinically diagnosed cases are referred to as corticobasal syndrome (CBS) [
2].
At present, treatment of CBS is limited. The pharmacological intervention such as levodopa was largely ineffective in the management of CBS [
3]. Recently, there have been reports suggesting the effectiveness of botulinum toxin injections in CBS patients with dystonia [
4].
We report case series in which patients with gait instability due to CBS improved after rehabilitation therapy. The first and second cases were patients with left unilateral lower leg dystonia, which improved abnormal tone and gait pattern after alcohol block and botulinum toxin injection. The third case was a patient with left unilateral side sensory abnormality and limb apraxia, gait pattern improved after gait training with a visual cue, whole body therapeutic pool, and robotic assisted gait training.
CASE REPORT
Patient 1
An 80-year-old woman with the history of total knee replacement for both knees due to osteoarthritis, and right total hip replacement after femur neck fracture was started on levodopa 4 years ago due to left leg resting tremor and gait instability. The dosage of levodopa was raised gradually. Despite this change in treatment, no changes in symptoms were observed and she could not initiate gait step properly.
She was then referred to the department of rehabilitation medicine. Physical examinations revealed 20° limitation in the abduction at the angle of the hip joint, inversion of the left foot (
Fig. 1), involuntary movement in the left lower extremity, and increased muscle tone at the left hip adductor, ankle plantar flexor, and foot inverter. Electromyography revealed continuous muscle contractions at the left hip abductor, gastrocnemius, and tibialis posterior muscles after sufficient muscle rest. The overall findings allowed us to diagnose this patient with CBS.
Fig. 1
Inversion of left ankle in case 1 patient.

We performed electromyography-guided alcohol block to the left obturator nerve and ultrasound-guided botulinum toxin injection to the left medial/lateral gastrocnemius and the tibialis posterior muscles with a dosage of 70, 70, and 60 units, respectively.
One week after the injection, a follow-up electromyography showed decreased dystonic muscle contractions. Follow-up physical examinations revealed 40° in the abduction angle of the left hip joint, decreased frequency and duration of the involuntary movement. Stretching exercise was continued in order to reduce muscle tone in left ankle and hip muscles. Afterwards, she underwent lower extremity strengthening exercise through sit-to-stand training and one leg standing. Finally, she could walk for 200 meters by holding an anterior walker.
Patient 2
A 69-year-old woman presented with walking difficulty for a year. After being diagnosed with lumbar spine spondylolisthesis by the department of orthopedic surgery, she had undergone posterolateral fusion on the lumbar spine. Despite the operation, gait disturbance was not improved.
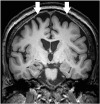
She visited the department of neurology and finally was diagnosed with gait disturbance due to Parkinsonism. Brain magnetic resonance imaging (MRI) showed cortical atrophy of bilateral cerebral hemisphere (
Fig. 2). The dosage of levodopa was raised gradually. However, gait disturbance was not improved. She was referred to the outpatient department of rehabilitation medicine.
Fig. 2
Coronal view of magnetic resonance image demonstrating cortical atrophy of bilateral cerebral hemisphere (white arrows) in case 2 patient.
She could not initiate the gait step properly which was similar to freezing of gait. Physical examinations revealed lead-pipe rigidity at the left lower extremity and increased muscle tone at the left hip adductor and calf muscles. Finally, we diagnosed it with lower limb dystonia as one of the symptoms in CBS.
We performed obturator nerve block and botulinum toxin injection to the left medial/lateral gastrocnemius and the tibialis posterior muscles. Stretching exercise was continued in order to reduce muscle tone in left ankle and hip muscles. After that, we performed lower extremity strengthening through sit-to-stand and squatting exercise, weight shifting in standing posture in order to improve standing balance. In the beginning, gait training was continued with an anterior walker, and gradually gait training was carried out independently with a verbal cue. One week after the injection, finally, she could walk 100 meters independently in level grounds (
Supplementary Video. 1).
Patient 3
A 57-year-old woman with no prior medical history. Four years ago, she noted a strange sensation on the left leg and began to develop gait instability shortly after that. In addition, the subjective motor weakness of left arm and leg began to progress. However, there was no problem in activities of daily living. At the same time dysarthria began to emerge, and when she tried to speak, the word did not come out immediately.
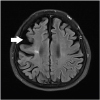
Brain MRI revealed cortical atrophy of right cerebral hemisphere (
Fig. 3). She was diagnosed with CBS and was started on levodopa. However since her symptoms was persisted, she was admitted to the Department of Rehabilitation Medicine. Physical examinations revealed no motor weakness and no dystonia in all extremities. Speech evaluation was performed. In terms of language it was normal, but there was a problem in speech. There were some weak vocalizations, inaccurate articulation, and non-fluent speaking.
Fig. 3
Axial view of magnetic resonance image demonstrating cortical atrophy of right cerebral hemisphere (white arrow) in case 3 patient.
Additionally, she showed limb apraxia of the left leg. Upon gait analysis, left leg swing phase duration and gait velocity decreased. After performing lower extremity strengthening exercise, we performed Frenkel's exercise in standing position. In order to initiate the left leg, cane dependent gait training was continued with visual cue by a laser pointer. Furthermore, she continued gait training with a whole body therapeutic pool and robotic assisted gait training. At discharge, gait initiation and stride length improved and gait velocity also improved (
Supplementary Video. 2).
DISCUSSION
CBD is a pathologic disorder resulting from abnormal aggregation of hyperphosphorylated tau isoforms with 4 conserved repeat sequences (4R tau). CBS is a motor presentation with asymmetric dystonia, and myoclonus accompanied by higher cortical features including apraxia, alien limb phenomena, cortical sensory loss, and cognitive changes. It is now recognized that CBS is only one presenting phenotype of CBD [
4].
The 3 cases described above showed various clinical features. Asymmetric dystonia was seen in the first and second cases. Cortical sensory loss was seen in the third case and left lower limb apraxia was seen in all cases. Gait apraxia is one of the most frequent signs in CBS [
5]. Limb-kinetic apraxia may be an isolated early feature, while ideational apraxia is typically late and associated with more severe cognitive dysfunction [
6]. In all 3 cases, lower limb apraxia was more prominent than ideational apraxia.
There are no published cases in which a significant and sustained clinical improvement has occurred with L-dopa therapy [
3]. Many regard the lack of objective improvement during therapy with 1,000 mg of daily L-dopa (divided doses, on an empty stomach) as a diagnostic feature of CBD [
7]. In patients with the first and second cases, levodopa was used, but gait disturbance did not improve.
CBS is similar in clinical symptom to freezing gait when the on-off phenomenon of Parkinson disease occurs. The difference between the 2 is that freezing gait responds partially to levodopa, but CBS does not. In other words, it is important to distinguish between CBS and Parkinson disease in order to apply an effective treatment regimen to patients. Second, freezing gait is usually observed when on-off symptoms occur after Parkinson disease progresses while unilateral lower limb gait apraxia was the primary symptom of CBS. In this way, these 3 cases can be thought of as CBS, not an on-off symptom of Parkinson disease [
8].
Dystonia is most successfully treated with targeted botulinum toxin injections and chemical denervation [
3]. It is widely accepted that Botulinum toxin injections for dystonia in CBS can be used to reduce pain, improve hygiene, prevent secondary contractures, and on occasion, improve limb function early in the disease course [
9]. In the first and second cases, we performed an alcohol block on the obturator nerve and injected botulinum toxin into the lower leg to reduce dystonia. We found that dystonia was reduced and gait was improved in CBS patients.
Recently, a multidisciplinary therapeutic approach, including low-frequency repetitive transcranial magnetic stimulation (rTMS), has been reported to be beneficial to CBS patients [
1]. Rehabilitation treatments such as whole body therapeutic pool and robotic assisted gait training have recently become popular treatments, but few reports have shown benefits of these regimens.
Previous studies reported that dystonia and pain were reduced through botulinum toxin injection in CBS patients with dystonia [
3], but there was no case focusing on gait improvement after the injections. Additionally, as mentioned above, no prior studies have demonstrated the effectiveness of whole body therapeutic pool and robotic assisted gait training. Here, we report that botulinum toxin injections can drastically improve gait function in CBS patients, and that novel therapeutic regimens may be used in conjunction with the injection to further improve the outcome.
In conclusion, through this case series, we highlight the importance of accurately diagnosing CBS patients and report that treatments such as nerve block or gait training according to the patient's symptoms can drastically improve the gait pattern with overcoming lower limb apraxia.