Abstract
Purpose
This study aimed to analyze the learning curves for colorectal surgery fellows in a colonoscopy training program.
Methods
Between May 2003 and February 2017, 60 surgical fellows joined our 1-year colonoscopy training program as trainees and performed 43,784 cases of colonoscopy. All trainees recorded their colonoscopy experiences prospectively into the database. After excluding 6 trainees, who had experience with performing more than 50 colonoscopies before participating in our training program or who discontinued our training program with experience performing less than 300 colonoscopies, this study included 54 trainees who had performed 39,539 colonoscopy cases. We analyzed the cecal intubation rate (CIR) and cecal intubation time (CIT) using the cumulative sum (Cusum) technique and moving average method to assess the technical colonoscopy competence.
Results
Overall, the CIR by the trainees was 80.7%. The median number of cases of colonoscopy performed during the training period for each trainee was 696 (range, 322–1,669). The trainees were able to achieve a 90% CIR with 412 and 493 procedures when analyzed using the moving average and the Cusum, respectively. Using the moving average method, CIRs after 150, 300, and 400 procedures were 67.0%, 84.1%, and 89.2%, respectively. The CIT of trainees continuously decreased until 400 successful cases. Median CITs were 9.4, 8.3, and 7.4 minutes at 150, 300, and 400 successful cases, respectively.
Colonoscopy is widely used not only for the diagnosis, but also for the treatment of colorectal disease. A competent colonoscopist can accurately and safely inspect the entire colon and rectum to facilitate diagnosis of colorectal diseases. A welltrained colonoscopist should be able to find lesions without missing them and treat them without complications [1].
Systematic colonoscopy training programs can maximize the capacity of trainees to learn colonoscopy skills, and these training programs can be of great help in obtaining the objective data needed for colonoscopy competency [2]. Competency of colonoscopy can be verified by various factors, such as the time of intubation, minimization of patient discomfort, appropriate sedative use, adenoma detection rate, and polyp retrieval rate, but the cecal intubation rate (CIR) is still an important variable for evaluating one's colonoscopy ability [34]. Because not all colonoscopies can reach to the cecum due to patient discomfort, poor bowel preparation, diverticular disease and strictures, the Joint Advisory Group on Gastrointestinal Endoscopy in the United Kingdom proposed a target CIR of 90% [5].
Because of the importance of colonoscopy in the diagnosis and treatment of colorectal disease, it is an essential skill that colorectal surgeons must learn. However, only a few studies have been reported about the training program for colonoscopy, especially for the colorectal surgical fellows, in Korea. Thus, this study aimed to assess the colonoscopy learning curves for colorectal surgery fellows obtained during a colonoscopy training program. Given the importance of CIR in assessing competency, this study focused on CIR.
Since 2003, National Cancer Center (NCC) Korea has conducted the colonoscopy training program for surgical fellows, called the Colonoscopy Academy of NCC (CAN). The CAN is a 1-year course, including 7 steps (Table 1). Between May 2004 and December 2016, 60 surgical fellows joined the CAN as trainees and performed a total of 43,784 cases of colonoscopy. Among these, 6 trainees and their data were excluded from the analysis of this study; these trainees had experience with performing more than 50 colonoscopies before participating in our training program, or they discontinued our training program with experience performing less than 300 colonoscopies. After exclusion, this study included 54 trainees with a total of 39,539 cases of colonoscopy. The prospectively collected CAN database was reviewed retrospectively, and this study was confirmed to be exempt from review by the Institutional Review Board of National Cancer Center Korea (NCC2018-0009).
During the course, the trainees were required to complete the e-form records for all the cases performed by them. The e-form records include the following information: name of trainee and trainer, date of the procedure, sex and age of the anonymized patient, aim of colonoscopic test, status of bowel preparation, history of abdominal surgery, history of anticoagulant medication, therapeutic procedures, reached colonic site and spent time (if the reached colonic site is cecum, it means that the trainee succeeded in cecal intubation without relief), colon pattern, colonic site for relief, reason for relief, total time spent, and number of polyps. All the records completed by trainees are stored in the CAN database.
The relationships between the CIR, cecal intubation time (CIT), and number of colonoscopies were evaluated, and the number of colonoscopies required to achieve CIR ≥ 90% was calculated using the moving average and the learning curve cumulative sum methods.
The mean CIR was calculated using 20 procedural blocks for each trainee [6]. The mean CIR for all trainees was calculated and plotted against the number of procedures performed. If the moving average CIR exceeded 90%, a trainee was considered competent with colonoscopy in this study.
For reference, we used the following symbols and formula to calculate the moving average.
where Pt denotes the latest outcome at the date t and MAtn denotes the n days moving average at the date t.
In addition, we tested the success rate difference between the 2 groups, trainees who experienced 400 cases under 6 months versus those who experienced 400 cases over 6 months. First, we checked preassumptions of the variable proportion. The variable proportion met the equality of variance (P = 0.713), but it did not meet the assumption of normality (in the Kolmogorov-Smirnov test, the P-value was <0.01). Thus, we had to use the nonparametric method, the Wilcoxon rank-sum test. In this test, we set the statistical hypothesis as follows:
where p1 is the success rate of trainees under 6 months and p2 is the success rate of trainees over 6 months.
Cumulative sum analysis (Cusum) is a technique used for monitoring the result by graphing the change of the dichotomy results, such as the error or failure rate. Unlike other Cusum techniques, the learning curve cumulative sum (LC-Cusum) is designed for the learning and training of techniques. The LC-Cusum assumes that the process is still a learning phase in the case of the null hypothesis (H0), whereas the alternative hypothesis (H1) assumes that the process is in competent phase. At the moment when LC-Cusum exceeds the defined threshold (h), H0 is rejected in favor of H1 because there is ample evidence to indicate that the procedure has been learned. If LC-Cusum does not exceed the threshold, competence is not yet proven, and monitoring should continue [37].
For reference, we used the following symbols and formula to calculate the Cusum score and arrive at the learning curve.
where s is the downward decrement with each success on a Cusum plot, while the upward increment with each failure is 1-s
where p0 is an acceptable failure rate, and p1 is an unacceptable failure rate.
We also denote the boundary h0 and h1 as shown in the equation given below:
where a = ln[(1-β)/α] and b = ln[(1-α)/β]; α is a type 1 error, and β is a type 2 error.
Overall, the CIR by the trainees was 80.7% (31,890 of 39,539). The median number of cases of colonoscopy performed during the training period of each trainee was 696 (range, 322–1,669). The mean age of the patients was 54.4 ± 11.3 years. Subjects included 23,039 men (58.3%) and 16,500 women (41.7%).
The mean CIR using the moving average method was compared to the number of colonoscopies for all trainees (Fig. 1). The mean CIRs were 57.0%, 75.2%, and 84.1% after 100, 200, and 300 procedures, respectively. The mean CIR reached 90% of the standard at 412 colonoscopies. The median number of procedures by which the trainee group reached competency was 493 for CIR of 90% using LC-Cusum. The numbers of required procedures for CIR of 80% and 85% were 350 and 408, respectively (Fig. 2).
In addition, in the 2-sided Wilcoxon two-sample test, the P-value was 0.249 when we analyzed the difference in the success rate between the two groups, trainees who experienced 400 cases under 6 months versus those who experienced 400 cases over 6 months. We also had to accept hypothesis H0. Therefore, we concluded that the success rate of trainees who experienced 400 cases under 6 months versus those who experienced 400 cases over 6 months was not different.
The mean CIT was 8.80 ± 2.09 minutes. The CIT continuously decreased until 400 successful cases, where the median CIT was 8.2 minutes from the initial 10.5 minutes (Fig. 3). The CIT continuously improved at 10.1, 8.9, and 8.8 minutes for every 100 consecutive blocks. There was an inverse correlation between the CIT and success rate. The time to cecal intubation continued to improve as the number of cases increased.
In this study, we showed that a mean CIR of 90% by trainees was reached at 412 colonoscopies, as calculated using moving average analysis. Trainees were found to be competent after 493 colonoscopies using the LC-Cusum method, while 350 and 408 colonoscopies were required for CIRs of 80% and 85%, respectively. The number of cases that reached the learning curve was slightly higher in this study than those of other studies. The time to cecal intubation, analyzed using the moving average method, decreased and was found to improve continuously as the number of cases increased. This is the first study to report about a colonoscopy training program and the resulting achievement of colonoscopy competence by colorectal surgeons in Korea.
A lot of training and experience is required to perform colonoscopy optimally. It is not always possible for an expert to reach the cecum [3]. Competency must be determined on an objective basis. Therefore, the United States Multi-Society Task Force on Colorectal Cancer recommended 2 simple, continuous quality improvement goals when performing colonoscopy: (1) CIRs of >90% in all colonoscopies and >95% in screening colonoscopies, and (2) photographic documentation for cecal intubation and visualized landmarks [2]. However, there is a large difference between the results of other studies on the recommended minimum number of procedures before evaluating competency [8910]. Previous studies have reported a requirement of at least 150–400 procedures to achieve competency for colonoscopic procedures [11112], which is less than the number of procedures determined in our study. These differences could be explained as follows: first, there may not be strict indications for being relieved by the supervisors. Most of the previous studies allowed 20 or 30 minutes for the trainee to perform colonoscopy, and some studies had no time limits; however, this study allowed only 10 minutes to perform colonoscopy. Second, subjects were limited to colorectal surgeons in this study, while other studies focused on gastrointestinal fellows accustomed to manipulating the scope because they simultaneously performed gastroscopy during their training sessions.
Colonoscopy is a complex technique that requires proper training and experience to ensure that it is performed accurately and safely. Colorectal surgeons are involved in every step of colorectal disease from diagnosis to treatment, and consequently, colonoscopy is one of the essential skills that colorectal surgeons should learn. The surgeon's proficiency in colonoscopy has several advantages. It is the surgeon who is an expert in intra-abdominal anatomy, and therefore, it is safer to perform diagnostic, postoperative follow-up and therapeutic endoscopy. Additionally, it will be easier to manage severe complications such as bowel perforation.
To date, previous studies have been conducted in various endoscopic training situations in multiple centers, and data heterogeneity may exist. However, our data were collected at a single center. CAN was founded in 2003 to build the colonoscopy expertise of colorectal surgeons. Therefore, our colonoscopy training systems reflect the colonoscopy learning curves of colorectal surgery trainees in a general hospital. Most reports have indicated that CIRs above 90% are a goal of colonoscopy training programs because experienced colonoscopists consistently achieve CIRs above 90% [1314]. Therefore, we focused on a target CIR of 90% as an indicator of competency of colonoscopy in this study. CIT is another important parameter. Prolonged intubation during colonoscopy can cause discomfort to the patient and reduce the colonoscopist's concentration. Therefore, we used 2 objective criteria, the CIR (>90%) and CIT (≤10 minutes), as indicators of competence in colonoscopy training [1]. In the present study, CIT decreased from an initial 10.5 minutes to a final 8.2 minutes at the 400th successful case. There is a possibility that the mean CIT could be underestimated because we did not count cases in which the cecum could not be reached.
Colonoscopy training requires clinical experience with patients, and this must be done within the basic ethical principles that minimize patient inconvenience. It is natural that trainee skills will improve through accumulating cases over a long period. Because the colonoscopy training programs for surgeons have not yet been established and there is limited research on how long it is necessary to undergo training, it is necessary to establish an education program that enables effective colonoscopy training within a short period, and efforts should be made to develop a simulation device that minimizes the patient's discomfort.
Although the CIR or CIT is commonly used as a measure of actual competence at colonoscopy, other quality indicators including the adenoma detection rate, polyp detection rate, and procedure-related complications should be included to assess technical competence. However, because of the limitations of data collection in our study, we could not include quality indicators including the adenoma detection rate in the analysis of trainees' technical competence. This is one of the limitations of our study. Further research studies are needed in this regard.
Previous studies have shown that insertion of a colonoscope in women is more difficult than in men [151617]. This difference of difficulty is also known to be present in abdominal surgery and in patients with a low body mass index, old age, and poor bowel preparation [1819]. However, our study has limitations in using these indicators together for analysis. The colonoscopies analyzed in this study included those for screening and surveillance after colorectal resection. Since the history of abdominal surgery including colorectal resection can have an effect on colonoscopy insertion, additional analysis may be needed to confirm this effect. However, despite the presence of a history of abdominal surgery in approximately 55% of our patients, we were unable to perform additional analysis related to abdominal surgery because details of the operation's name and patients' medical history were not recorded in our database. A further study is required to include these parameters in the evaluation of training programs.
In conclusion, this is the first study in Korea investigating the number of procedures required to achieve competency in colonoscopy performed by the colorectal surgeon. Two statistical methods, moving average and LC-Cusum, showed that a mean CIR reached 90% after 412 and 493 procedures, respectively. We found that more than 400 cases of experience were needed for the technical competence of colonoscopy. Continuous teaching and monitoring is required until trainees become sufficiently competent.
Figures and Tables
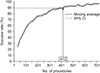 | Fig. 1Colonoscopy learning curve obtained using the moving average. The mean cecal intubation rate reached the standard of 90% in 412 colonoscopies. CI, confidence interval. |
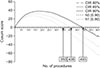 | Fig. 2Colonoscopy learning curve for 90% of the CIR (h0) obtained using the Cusum analysis. The median number of procedures for the group of competent trainees to reach competency is 493 for a CIR of 90%. The numbers of required procedures are 350 and 408 for CIRs of 80% and 85%, respectively. Cusum, cumulative sum; CIR, cecal intubation rate. |
ACKNOWLEDGEMENTS
This work was supported by grants from the National Cancer Center (NCC-1710070). The authors would like to thank all CAN alumni and institutional operators who have participated in the CAN training and have worked hard to accumulate data.
Notes
References
1. Lee SH, Chung IK, Kim SJ, Kim JO, Ko BM, Hwangbo Y, et al. An adequate level of training for technical competence in screening and diagnostic colonoscopy: a prospective multicenter evaluation of the learning curve. Gastrointest Endosc. 2008; 67:683–689.

2. Rex DK, Bond JH, Winawer S, Levin TR, Burt RW, Johnson DA, et al. Multi-Society Task Force on Colorectal Cancer. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2002; 97:1296–1308.

3. Ward ST, Mohammed MA, Walt R, Valori R, Ismail T, Dunckley P. An analysis of the learning curve to achieve competency at colonoscopy using the JETS database. Gut. 2014; 63:1746–1754.

4. Brahmania M, Park J, Svarta S, Tong J, Kwok R, Enns R. Incomplete colonoscopy: maximizing completion rates of gastroenterologists. Can J Gastroenterol. 2012; 26:589–592.

5. Chung JI, Kim N, Um MS, Kang KP, Lee D, Na JC, et al. Learning curves for colonoscopy: a prospective evaluation of gastroenterology fellows at a single center. Gut Liver. 2010; 4:31–35.

6. Koch AD, Haringsma J, Schoon EJ, de Man RA, Kuipers EJ. Competence measurement during colonoscopy training: the use of self-assessment of performance measures. Am J Gastroenterol. 2012; 107:971–975.

7. Park Y, Yong YG, Yun SH, Jung KU, Huh JW, Cho YB, et al. Learning curves for single incision and conventional laparoscopic right hemicolectomy: a multidimensional analysis. Ann Surg Treat Res. 2015; 88:269–275.

8. Parry BR, Williams SM. Competency and the colonoscopist: a learning curve. Aust N Z J Surg. 1991; 61:419–422.

9. Romagnuolo J, Enns R, Ponich T, Springer J, Armstrong D, Barkun AN. Canadian credentialing guidelines for colonoscopy. Can J Gastroenterol. 2008; 22:17–22.

10. Johna S, Klaristenfeld D. Surgery resident training in endoscopy: the saga continues. Arch Surg. 2011; 146:899–900.
11. Guidelines for credentialing and granting privileges for gastrointestinal endoscopy. American Society for Gastrointestinal Endoscopy. Gastrointest Endosc. 1998; 48:679–682.
12. Cass OW, Freeman ML, Peine CJ, Zera RT, Onstad GR. Objective evaluation of endoscopy skills during training. Ann Intern Med. 1993; 118:40–44.

13. Rex DK. Still photography versus videotaping for documentation of cecal intubation: a prospective study. Gastrointest Endosc. 2000; 51(4 Pt 1):451–459.

14. Marshall JB, Barthel JS. The frequency of total colonoscopy and terminal ileal intubation in the 1990s. Gastrointest Endosc. 1993; 39:518–520.

15. Waye JD, Bashkoff E. Total colonoscopy: is it always possible. Gastrointest Endosc. 1991; 37:152–154.

16. Hull T, Church JM. Colonoscopy--how difficult, how painful? Surg Endosc. 1994; 8:784–787.
17. Church JM. Complete colonoscopy: how often? And if not, why not? Am J Gastroenterol. 1994; 89:556–560.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download