Dear Editor,
The incidence of opportunistic infections in immunosuppressed patients has increased in recent decades. Although the most common fungus is Aspergillus species, an upward trend has been observed in some other species such as Scedosporium prolificans. We report the case of a 36-year-old woman with multiple sclerosis (MS) who developed a disseminated Scedosporium prolificans infection with central nervous system (CNS) involvement.
The patient was diagnosed with relapsing-remitting MS following an outbreak of cervical myelitis, which was confirmed by brain and spine MRI (Fig. 1) and cerebrospinal fluid analysis. Treatment was started with interferon beta-1a according to the current protocol in Spain. Three years later there was evident progressive impairment of the spastic paraparesis and ataxia independent of relapses, and so a diagnosis of secondary progressive multiple sclerosis (SPMS) was made. Because the only treatment indicated for SPMS is interferon in Spain, pulses of five 1-g boluses of intravenous methylprednisolone every 3 months were added in an attempt to stabilize the disease course, which is commonly applied in many institutions, including in Spain.
Twenty days after the second cycle of steroids, the patient was admitted due to fluctuating consciousness, confusion, headache, diplopia, and spastic quadriplegia. A CT scan showed hypodense lesions involving the right thalamus and occipital lobe. MRI revealed ischemia in the cerebellar hemispheres, right thalamus, and medial temporal and occipital lobes, subarachnoid hemorrhage (SAH) around the midbrain and ventricular system, and a filling defect of the basilar artery (BA) (Fig. 2A–D). The patient deteriorated suddenly with consciousness impairment, and CT revealed an increase in the SAH that caused tetraventricular hydrocephalus. CT angiography revealed severe vasospasm, and the presence of aneurysms could not be ruled out. A ventricular drain was inserted to release acellular cerebrospinal fluid, which had low glucose and high protein levels. The patient died several hours later. The autopsy revealed dilatation compatible with a ruptured aneurysm and a thrombus in the BA. A microscopy examination showed necrotic ruptured arterial walls and infiltration of polymorphonuclear cells involving the posterior communicating artery, anterior inferior cerebellar artery, and BA (Fig. 2E). Multiple fungal structures identified as Scedosporium prolificans were found in the necrotic areas and the arterial thrombus (Fig. 2F), and also in the pulmonary vessels, larynx, and small intestine. The final diagnosis made by the anatomical pathology department was ruptured mycotic aneurysms in the BA, anterior inferior cerebellar artery, and posterior communicating artery, with ischemic stroke involving the brainstem and the base of the brain, and SAH.
Scedosporium prolificans is a ubiquitous fungus with a worldwide distribution that is transmitted via the inhalation of spores or direct inoculation. Human Scedosporium prolificans infection was first described in 1984 in a case of osteomyelitis.1 A Scedosporium prolificans infection may manifest in three ways:2 airway colonization, local infection (immunocompetent patients after near-drowning, trauma, or surgery), and disseminated infection. Disseminated infection is the most frequent type, and it has a very high mortality rate3 and is usually associated with immunosuppression, especially AIDS or blood disorders,4 although isolated cases have been described in immunocompetent patients.3 Disseminated forms affect the CNS to cause meningoencephalitis, abscesses, or vasculitis.2 Scedosporium prolificans is easily isolated in cultures; however, a positive airway culture may only indicate colonization.3 Scedosporium prolificans is highly resistant to antifungals, although some authors have reported positive results when combining voriconazole and terbinafine.3 The disease progresses rapidly to death,3 and survival is related to the restoration of immunity and the possibility of surgery in localized infections.35 Scedosporium prolificans is particularly angioinvasive, and encroaches both medium-sized and large arteries.25 The most common type of CNS involvement is ischemic stroke,2 especially in the posterior circulation territory,5 although corticosubcortical lesions without edema or contrast uptake are reported.2 The fulminant course may prevent the formation of abscesses. Mycotic aneurysms are rare, with few reported cases of BA aneurysm secondary to Scedosporium prolificans,5 although there are reports of SAH without confirmed aneurysms.2 As in our patient, aneurysms usually involve the circle of Willis and its main branches.2 All of these reported cases occurred in immunosuppressed patients with hematological neoplasia or bone marrow transplant, and none of them survived.
The present case is the first of Scedosporium prolificans infection in a patient with MS. Only a case with keratomycosis due to Scedosporium apiospermum has been reported previously.6 Because interferon beta-1a did not cause a hematological alteration and has not been related to opportunistic infections, periodic steroids represent the only possible predisposing factor, as in some previously described cases.4 Glucocorticoids have been repeatedly suggested to increase the risk of infections, especially opportunistic infections, even when administered as pulse therapy.78 Awareness of emergent opportunistic infections in MS patients is necessary, particularly when applying modern treatments that involve immunosuppression. A high suspicion level is particularly important in strokes involving the posterior circulation, even in the absence of fever.
Figures and Tables
Fig. 1
MRI T2-weighted images showing hyperintensities (arrows) in the brainstem and spinal cord. A: Brainstem, sagittal view. B: Brainstem, axial view. C: Spinal cord, sagittal view.
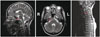
Fig. 2
Composition of CT scan (A), MRI (B–D), and anatomical pathology (E–F) images. A: CT image obtained at admission showing thalamic hypodensity (arrow). B: Hyperintensities in MRI long-repetition-time images with (C) restricted diffusion in medial temporal and occipital lobes (arrows). D: MRI gradient-echo images displaying small subarachnoid hemorrhage foci in the interpeduncular cistern and anterior to the right cerebral peduncle (arrow). E: Microscopy image revealing necrosis and rupture of the arterial wall of the basilar artery, in which a ruptured aneurysm dilatation and a vascular thrombus are evident (hematoxylin-eosin stain, ×20). F: Methenamine silver staining showing multiple fungal structures identified as Scedosporium prolificans in the necrotic areas (×400).

References
1. Malloch D, Salkin IF. A new species of Scedosporium associated with osteomyelitis in humans. Mycotaxon. 1984; 21:247–255.
2. Marco de Lucas E, Sádaba P, Lastra García-Barón P, Ruiz Delgado ML, Cuevas J, Salesa R, et al. Cerebral scedosporiosis: an emerging fungal infection in severe neutropenic patients: CT features and CT pathologic correlation. Eur Radiol. 2006; 16:496–502.

3. Rodriguez-Tudela JL, Berenguer J, Guarro J, Kantarcioglu AS, Horre R, de Hoog GS, et al. Epidemiology and outcome of Scedosporium prolificans infection, a review of 162 cases. Med Mycol. 2009; 47:359–370.

4. Idigoras P, Pérez-Trallero E, Piñeiro L, Larruskain J, López-Lopategui MC, Rodríguez N, et al. Disseminated infection and colonization by Scedosporium prolificans: a review of 18 cases, 1990-1999. Clin Infect Dis. 2001; 32:E158–E165.

5. Ong A, Blyth CC, Bency R, Vicaretti M, Harun A, Meyer W, et al. Fatal mycotic aneurysms due to Scedosporium and Pseudoallescheria infection. J Clin Microbiol. 2011; 49:2067–2071.

6. Díaz-Valle D, Benitez del Castillo JM, Amor E, Toledano N, Carretero MM, Díaz-Valle T. Severe keratomycosis secondary to Scedosporium apiospermum. Cornea. 2002; 21:516–518.

7. National Medical Advisory Board of the National Multiple Sclerosis Society. Recommendations regarding corticosteroids in the management of multiple sclerosis. US Neurology. 2008; 4:22–24.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download