Abstract
Background
Syndecan-1 (sCD138) has recently been suggested to predict the clinical course of early-stage chronic lymphocytic leukemia (CLL), but few studies have been reported. This study assessed the role of syndecan-1 in the prognosis of patients with CLL and its correlation with other prognostic markers.
Methods
This prospective study was performed in the hematology department of an Indian tertiary care center, over nineteen months (Jun. 2009–Jan. 2011). Forty-nine new patients with CLL presented during this period and were included. Twenty age- and gender-matched healthy patients served as controls, and six patients with multiple myeloma were included as positive controls. Baseline serum syndecan-1 concentrations were measured for all patients at presentation using ELISA (Diaclone, Besancon, France). At baseline, patients were divided into low (N=10), intermediate (N=18) and high (N=21) risk cohorts. Serum syndecan-1 levels in these patient subgroups were compared with clinical and laboratory parameters.
Results
The median syndecan-1 level in patients with CLL (73.32 ng/mL, range, 28.71–268.0 ng/mL) was marginally higher than that in healthy patients (63.10 ng/mL, range, 55.0–75.11 ng/mL). At presentation, syndecan-1 levels in patients with CLL correlated strongly with symptomatic disease (cytopenias, P=0.004) and higher clinical stage (Rai stage III and IV, P=0.001) markers and poorly with β2-microglobulin level (P=0.270), diffuse BM infiltration (P=0.882), and surrogate mutation status markers (CD 38, P=0.174 and ZAP-70, P=0.459). Syndecan-1 levels dichotomized by the median value were higher with progressive disease markers, e.g. shorter lymphocyte doubling time (LDT, P=0.015) and increased treatment (P=0.099).
Syndecan-1 (sCD138), a member of the syndecan family of proteoglycans, is a transmembrane protein expressed on epithelial cells, B lymphocytes, and plasma cells [1]. These transmembrane proteins act as adhesion molecules and serve as coreceptors for various growth factors, thereby contributing to the proliferative capability of the host cell. The protein has three domains; namely, the cytoplasmic, transmembrane, and extracellular domains [1]. The extracellular domain is constantly shed from cell surface during normal cell turnover, resulting in presence of sCD138 in circulation. This release of the ectodomain decreases cell adhesion to the matrix, leading to increased cell motility and invasion [1].
The shed ectodomain exists in the circulation in a biologically active form (soluble syndecan-1 or sCD138), which can bind various growth factors, including EGF, FGF, and HGF [2]. The soluble form of syndecan-1 promotes invasiveness and inhibits proliferation, as opposed to the membrane-bound form, which increases proliferation and inhibits invasiveness [2].
The role of syndecan-1 in myeloma cell growth and the prognosis of patients with multiple myeloma patients is well known [3]. Recent studies have revealed its role in predicting the clinical course of patients with chronic lymphocytic leukemia, and some studies showed correlation of baseline sCD138 levels with disease burden at presentation [4567]. At present, sCD138 appears to be a potential prognostic marker; but with the advent of targeted therapeutic agents in the future, it may also have therapeutic implications. This study was undertaken to determine the correlation of baseline sCD138 in patients with CLL with other biological and clinical parameters.
This was a prospective study conducted at the Department of Hematology of an Indian tertiary care center, over a nineteen months, from June 2009 to January 2011. A total of 49 newly diagnosed patients with CLL were included in the study. These patients were diagnosed based on the characteristic immunophenotyping profile (patients with peripheral blood absolute lymphocytosis >5,000/cmm and a Matute's score of 4 or 5 were diagnosed with CLL) [8]. Patients with previously-treated CLL, atypical CLL (Matute's score of 3 or less), or reactive lymphocytosis were excluded from the study. The patients' clinical details were studied from individual case records. The study obtained necessary ethical clearance from the institute's ethics committee.
The basic investigations that were performed in all patients included complete blood count (Sysmex XT1800i, Kobe, Japan), peripheral blood smear examination (for morphology and percentage of smudge cells), and immunophenotyping by flowcytometry (FACScanto, BD Biosciences, San Jose, CA, USA). The marker panel included CD 45, CD 19, CD 20, CD 79 b, CD 22, CD 2, CD 3, sIg G, sIg M, kappa and lambda (for clonality), CD 38, and ZAP 70 (expression >20% considered positive for all markers except CD 38, where expression >30% was considered positive). Patients with peripheral blood absolute lymphocytosis >5,000/cmm and a Matute's score of scoring 4 or 5 were considered positive for CLL. A bone marrow examination as a diagnostic test was not mandatory at presentation; hence, trephine biopsies were evaluated in a subset of the patients (27 cases) [9]. Beta 2 microglobulin (β2 MG) levels were available in only 10 patients. The staging of all patients was performed according to a modified Rai's staging system. Patients were classified into low, intermediate, and high-risk groups [10].
Serum levels of sCD138 were determined by an enzyme immunoassay using kit marketed by Diaclone, Besancon, France. This is a solid phase sandwich enzyme-linked immunosorbent assay that uses a monoclonal antibody to sCD138. The test procedure was standardized using standards provided with the kit. All of the standards and samples were run in duplicates, as instructed. The results were measured in units of ng/mL. Serum syndecan-1 levels were measured for all patients at presentation. For comparison, twenty healthy age- and gender-matched controls and six patients with multiple myeloma were included (who served as positive controls).
Serum syndecan-1 levels in these patients were correlated with clinical features, hematological parameters, and available prognostic markers. Comparison of syndecan-1 levels between different patient subgroups (as per modified Rai's stages) was performed using the non-parametric Mann–Whitney U test or the Kruskal–Wallis test, for continuous variables, and the t test for categorical data. Statistical analyses were performed using SPSS (version 15) software and P-values <0.05 were considered statistically significant.
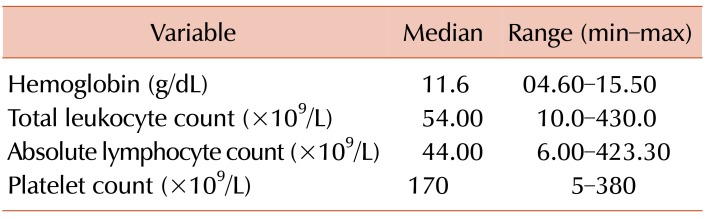
The study population was composed of 49 newly-diagnosed patients with CLL, with 39 (79.59%) males and 10 (24.39%) females. The median age of the study group was 60 years (range, 40–82 yr). Thirty-eight (77.6%) patients were symptomatic (had B symptoms) at presentation, while the remaining 11 (22.4%) patients were detected incidentally during routine evaluations. Thirty-three (67.3%) patients had organomegaly, and 17 (34.6%) patients had cytopenias at presentation. The distribution of patients as per modified Rai's staging was as follows; low risk N=10, intermediate risk N=18, high risk N=21 Baseline hematological parameters are shown in Table 1.
The median Syndecan-1 level across 49 patients with CLL was 73.32 ng/mL (range, 28.71–268 ng/mL), which was marginally higher than that in 20 healthy controls (63.10 ng/mL, range, 55.00–75.11 ng/mL), but this difference was not statistically significant (P=0.475). Six patients with multiple myeloma were included in the study as known positive controls for high syndecan-1 level (median level, 84.42 ng/mL) The syndecan-1 levels increased with increasing stage of the disease, and the correlation was significant (low risk, intermediate risk, and high risk; 42.89 ng/mL, 73.81 ng/mL, and 109.11 ng/mL, respectively, with P=0.025 low vs. intermediate risk and P=0.001 for low vs. high risk group).
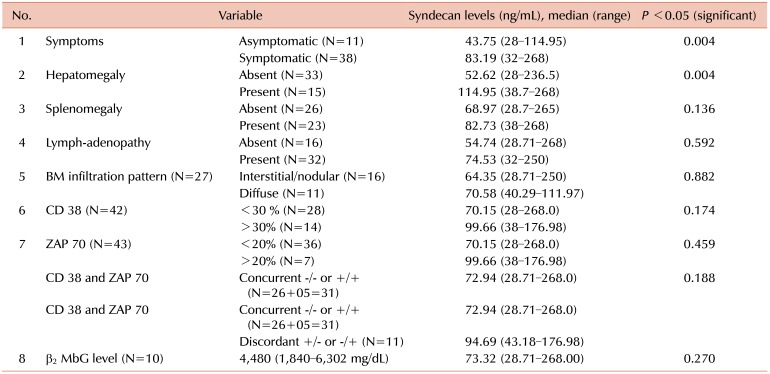
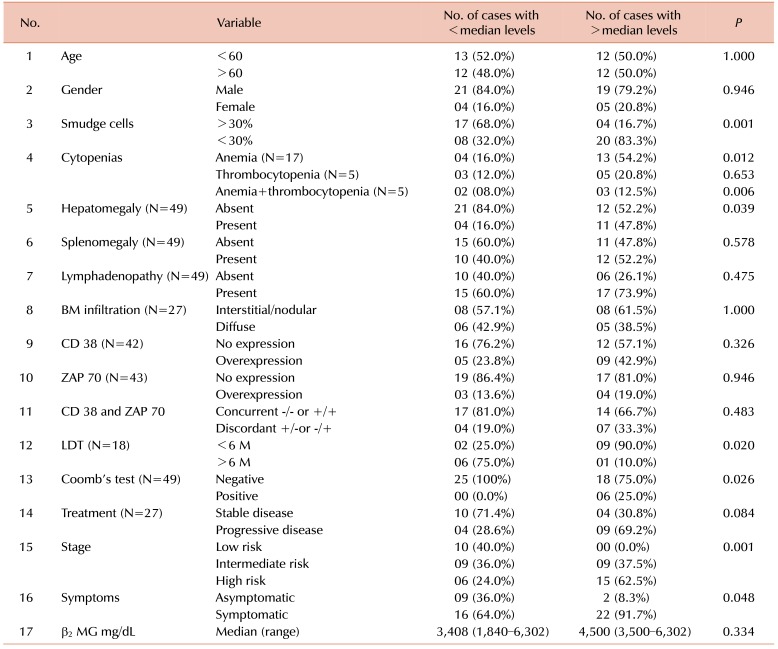
The correlation of serum syndecan-1 levels with other clinical and prognostic markers is shown in Table 2. Syndecan-1 levels, dichotomized by the median value, was correlated with various clinical and biological variables, which are given in detail in Table 3. Patients with higher baseline syndecan-1 levels had faster rates of lymphocyte doubling (as assessed by lymphocyte doubling time, LDT) and increased requirement for treatment during further follow-ups. The criteria for starting treatment included symptomatic cytopenias, bulky organomegaly, and modified Rai's stage 3 or 4 disease.
Syndecan-1 is a cytokine that is known to play a role in the differentiation and survival of the B lymphocyte lineage cells [1]. Recent studies have established that CD138 is detectable on CLL lymphocytes but not on other CD5-positive lymphoma cells. Its correlation with stage of disease and other prognostic markers is not established. This study was undertaken to assess the levels of syndecan-1 in the sera of patients with CLL and its correlation with clinical stage and other prognostic parameters.
In this study, we observed that the median syndecan-1 level in patients with CLL (73.32 ng/mL) was only marginally higher than that in normal healthy controls (63.10 ng/mL), and this difference was not statistically significant (P=0.475). This was at variance with other studies, where patients with CLL had significantly higher levels of syndecan-1 in comparison to healthy controls. The median value of syndecan-1 in patients with CLL patients vs normal healthy controls, as reported by Wolowiec et al. [5] and Jilani et al. [6], is 149 ng/mL vs. 36.7 ng/mL and 52.38 ng/mL vs. 19.86 ng/mL, respectively, with P-values of 0.0002 and <0.01, respectively. One explanation for higher syndecan-1 levels in controls, as found in our study, could be due to the presence of metalloprotease enzymes, which degrade syndecan-1 and can affect its values [11]. Therefore, whether syndecan-1 levels are constitutionally higher in Indians is not known because it has never been estimated in the Indian population before.
This study shows robust correlation of serum Syndecan-1 levels with symptomatic disease at presentation, presence of hepatomegaly, thrombocytopenia, and clinical Rai's stage. A similar correlation with stage was observed by Jilani et al. [6], wherein higher syndecan-1 levels correlated with higher clinical stage. However, Molica et al. [4] and Wołowiec et al. [5] did not report any such correlation [6]. Dhodapkar et al. [12] and Caligaris-Cappio et al. [13] observed a significant correlation with absolute lymphocyte count and proposed that syndecan-1 possibly is derived from the microenvironment, rather than the cell surface [1213].
Molica et al. [4] and Jilani et al. [6] did not report any correlation of median syndecan-1 levels at baseline with any prognostic marker (e.g. IgVH mutation status, β2-microglobulin), but this correlation became significant with dichotomized median levels of syndecan-1 [46]. They also showed that syndecan-1 levels were a good predictive marker of overall survival. The dichotomized median value of Syndecan-1 level in the current study showed good correlation with a few prognostic markers, but no added information was obtained. We did not find any correlation of syndecan-1 levels with β2-microglobulin levels and BM biopsy infiltration patterns.
One of the objectives of this study was to see the correlation of syndecan-1 levels with disease progression. In the absence of long-term follow-up, we investigated surrogates for long term survival, like LDT and the requirement for treatment due to cytopenia/stage 3 or 4 disease [14151617]. These two variables showed significant correlation with higher median syndecan-1 levels. Wołowiec et al. [5] also showed similar correlation in his study between median syndecan-1 levels and faster LDT and progressive disease.
Our study has the following limitations. This study was conducted as a cross-sectional study with limited number of cases, and a long-term follow-up was not performed to investigate the impact of the variables on long term outcomes. The prognostic markers that have been shown to have maximum influence on low risk disease outcomes and the associated patients were few. In some cases, full immunophenotype panel information or β2-microglobulin was not available due to cost constraints. The gold standard IgVH mutation studies by RT PCR were not available for validation. A bone marrow biopsy was performed in a limited number of cases. Study of metalloproteases and various cytokines, which can affect baseline syndecan-1 levels, could add more information.
The current study highlights the role of serum syndecan-1 level in CLL patients which is found to be higher than in the normal controls. It can be measured by a rapid and simple ELISA based kit. The elevated syndecan-1 levels at baseline correlate well with the clinical stage, tumor burden and markers of disease progression and hence can provide useful information about future course of disease.
References
1. Kopper L, Sebestyén A. Syndecans and the lymphoid system. Leuk Lymphoma. 2000; 38:271–281. PMID: 10830734.

2. Witzig TE, Kimlinger T, Stenson M, Therneau T. Syndecan-1 expression on malignant cells from the blood and marrow of patients with plasma cell proliferative disorders and B-cell chronic lymphocytic leukemia. Leuk Lymphoma. 1998; 31:167–175. PMID: 9720726.

3. Seidel C, Sundan A, Hjorth M, et al. Serum syndecan-1: a new independent prognostic marker in multiple myeloma. Blood. 2000; 95:388–392. PMID: 10627439.

4. Molica S, Vitelli G, Mirabelli R, et al. Serum levels of syndecan-1 in B-cell chronic lymphocytic leukemia: correlation with the extent of angiogenesis and disease-progression risk in early disease. Leuk Lymphoma. 2006; 47:1034–1040. PMID: 16840194.

5. Wołowiec D, Dybko J, Wróbel T, et al. Circulating sCD138 and some angiogenesis-involved cytokines help to anticipate the disease progression of early-stage B-cell chronic lymphocytic leukemia. Mediators Inflamm. 2006; 2006:42394. PMID: 16951490.

6. Jilani I, Wei C, Bekele BN, et al. Soluble syndecan-1 (sCD138) as a prognostic factor independent of mutation status in patients with chronic lymphocytic leukemia. Int J Lab Hematol. 2009; 31:97–105. PMID: 18190591.

7. Damle RN, Wasil T, Fais F, et al. Ig V gene mutation status and CD38 expression as novel prognostic indicators in chronic lymphocytic leukemia. Blood. 1999; 94:1840–1847. PMID: 10477712.

8. Matutes E, Owusu-Ankomah K, Morilla R, et al. The immunological profile of B-cell disorders and proposal of a scoring system for the diagnosis of CLL. Leukemia. 1994; 8:1640–1645. PMID: 7523797.
9. Han T, Barcos M, Emrich L, et al. Bone marrow infiltration patterns and their prognostic significance in chronic lymphocytic leukemia: correlations with clinical, immunologic, phenotypic, and cytogenetic data. J Clin Oncol. 1984; 2:562–570. PMID: 6726302.

10. Rai KR, Sawitsky A, Cronkite EP, Chanana AD, Levy RN, Pasternack BS. Clinical staging of chronic lymphocytic leukemia. Blood. 1975; 46:219–234. PMID: 1139039.

11. Sanderson RD, Lalor P, Bernfield M. B lymphocytes express and lose syndecan at specific stages of differentiation. Cell Regul. 1989; 1:27–35. PMID: 2519615.

12. Dhodapkar MV, Sanderson RD. Syndecan-1 (CD 138) in myeloma and lymphoid malignancies: a multifunctional regulator of cell behavior within the tumor microenvironment. Leuk Lymphoma. 1999; 34:35–43. PMID: 10350330.

13. Caligaris-Cappio F. Role of the microenvironment in chronic lymphocytic leukaemia. Br J Haematol. 2003; 123:380–388. PMID: 14616995.

14. Molica S, Alberti A. Prognostic value of the lymphocyte doubling time in chronic lymphocytic leukemia. Cancer. 1987; 60:2712–2716. PMID: 3677006.

15. Molica S, Mauro FR, Callea V, et al. The utility of a prognostic index for predicting time to first treatment in early chronic lymphocytic leukemia: the GIMEMA experience. Haematologica. 2010; 95:464–469. PMID: 19903673.

16. Hamblin TJ, Davis Z, Gardiner A, Oscier DG, Stevenson FK. Unmutated Ig V(H) genes are associated with a more aggressive form of chronic lymphocytic leukemia. Blood. 1999; 94:1848–1854. PMID: 10477713.

17. Crespo M, Bosch F, Villamor N, et al. ZAP-70 expression as a surrogate for immunoglobulin-variable-region mutations in chronic lymphocytic leukemia. N Engl J Med. 2003; 348:1764–1775. PMID: 12724482.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download