1. Parsons JK. Benign Prostatic Hyperplasia and Male Lower Urinary Tract Symptoms: Epidemiology and Risk Factors. Curr Bladder Dysfunct Rep. 2010; 5(4):212–218. PMID:
21475707.

2. Roehrborn CG. Pathology of benign prostatic hyperplasia. Int J Impot Res. 2008; 20:S11–S18.

3. Zhang P, Hu WL, Cheng B, Zeng YJ, Wang XH, Liu TZ, Zhang WB. Which play a more important role in the development of large-sized prostates (80 ml), androgen receptors or oestrogen receptors? A comparative study. Int Urol Nephrol. 2016; 48(3):325–333. PMID:
26685888.
4. Wang Z, Hu L, Salari K, Bechis SK, Ge R, Wu S, Rassoulian C, Pham J, Wu CL, Tabatabaei S, Strand DW, Olumi AF. Androgenic to oestrogenic switch in the human adult prostate gland is regulated by epigenetic silencing of steroid 5α-reductase 2. J Pathol. 2017; 243(4):457–467. PMID:
28940538.

5. Kiguradze T, Temps WH, Yarnold PR, Cashy J, Brannigan RE, Nardone B, Micali G, West DP, Belknap SM. Persistent erectile dysfunction in men exposed to the 5α-reductase inhibitors, finasteride, or dutasteride. PeerJ. 2017; 5:e3020. PMID:
28289563.

6. Canguven O, Burnett AL. The effect of 5 alpha-reductase inhibitors on erectile function. J Androl. 2008; 29(5):514–523. PMID:
18421068.
7. Aggarwal S, Verma A, Shukla R, Batra S, Bhardwaj TR, Kumar M. An overview of phytotherapeutic approaches for the treatment of benign prostatic hyperplasia. Mini Rev Med Chem. 2014; 14(3):257–270. PMID:
24456273.

8. Ko JW, Shin NR, Park SH, Kim JS, Cho YK, Kim JC, Shin IS, Shin DH. Pine bark extract (Pycnogenol®) suppresses cigarette smoke induced fibrotic response via transforming growth factor-β1/Smad family member 2/3 signaling. Lab Anim Res. 2017; 33(2):76–83. PMID:
28747971.
9. Bayomy NA, Abdelaziz EZ, Said MA, Badawi MS, El-Bakary RH. Effect of pycnogenol and spirulina on vancomycin-induced renal cortical oxidative stress, apoptosis, and autophagy in adult male albino rat. Can J Physiol Pharmacol. 2016; 94(8):838–848. PMID:
27203524.

10. Feng WH, Wei HL, Liu GT. Effect of PYCNOGENOL on the toxicity of heart, bone marrow and immune organs as induced by antitumor drugs. Phytomedicine. 2002; 9(5):414–418. PMID:
12222661.

11. Yang YS, Ahn TH, Lee JC, Moon CJ, Kim SH, Jun W, Park SC, Kim HC, Kim JC. Protective effects of Pycnogenol on carbon tetrachloride-induced hepatotoxicity in Sprague-Dawley rats. Food Chem Toxicol. 2008; 46(1):380–387. PMID:
17900780.

12. Eryilmaz A, Eliyatkin N, Demirci B, Basal Y, Kurt Omurlu I, Gunel C, Aktas S, Toka A, Basak S. Protective effect of Pycnogenol on cisplatin-induced ototoxicity in rats. Pharm Biol. 2016; 54(11):2777–2781. PMID:
27158843.

13. Huang WW, Yang JS, Lin CF, Ho WJ, Lee MR. Pycnogenol induces differentiation and apoptosis in human promyeloid leukemia HL-60 cells. Leuk Res. 2005; 29(6):685–692. PMID:
15863210.

14. Lee MY, Shin IS, Kyoung H, Seo CS, Son JK, Shin HK. α-spinasterol from Melandrium firmum attenuates benign prostatic hyperplasia in a rat model. Mol Med Rep. 2014; 9(6):2362–2366. PMID:
24682042.

15. Arivazhagan J, Nandeesha H, Dorairajan LN, Sreenivasulu K. Association of elevated interleukin-17 and angiopoietin-2 with prostate size in benign prostatic hyperplasia. Aging Male. 2017; 20(2):115–118. PMID:
28590830.

16. Bisson JF, Hidalgo S, Simons R, Verbruggen M. Preventive effects of lignan extract from flax hulls on experimentally induced benign prostate hyperplasia. J Med Food. 2014; 17(6):650–656. PMID:
24460407.

17. Kim CY, Chung KS, Cheon SY, Lee JH, Park YB, An HJ. Rice Hull Extract Suppresses Benign Prostate Hyperplasia by Decreasing Inflammation and Regulating Cell Proliferation in Rats. J Med Food. 2016; 19(8):746–754. PMID:
27441629.

18. Gratzke C, Bachmann A, Descazeaud A, Drake MJ, Madersbacher S, Mamoulakis C, Oelke M, Tikkinen KAO, Gravas S. EAU Guidelines on the Assessment of Non-neurogenic Male Lower Urinary Tract Symptoms including Benign Prostatic Obstruction. Eur Urol. 2015; 67(6):1099–1109. PMID:
25613154.

19. Harati K, Slodnik P, Chromik AM, Behr B, Goertz O, Hirsch T, Kapalschinski N, Klein-Hitpass L, Kolbenschlag J, Uhl W, Lehnhardt M, Daigeler A. Pro-apoptotic effects of pycnogenol on HT1080 human fibrosarcoma cells. Int J Oncol. 2015; 46(4):1629–1636. PMID:
25625225.

20. Romar GA, Kupper TS, Divito SJ. Research Techniques Made Simple: Techniques to Assess Cell Proliferation. J Invest Dermatol. 2016; 136(1):e1–e7. PMID:
26763463.

21. Vital P, Castro P, Ittmann M. Oxidative stress promotes benign prostatic hyperplasia. Prostate. 2016; 76(1):58–67. PMID:
26417670.

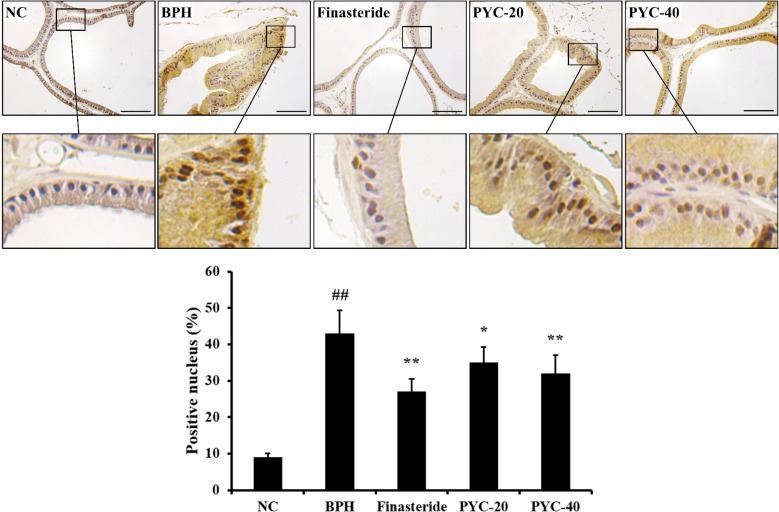
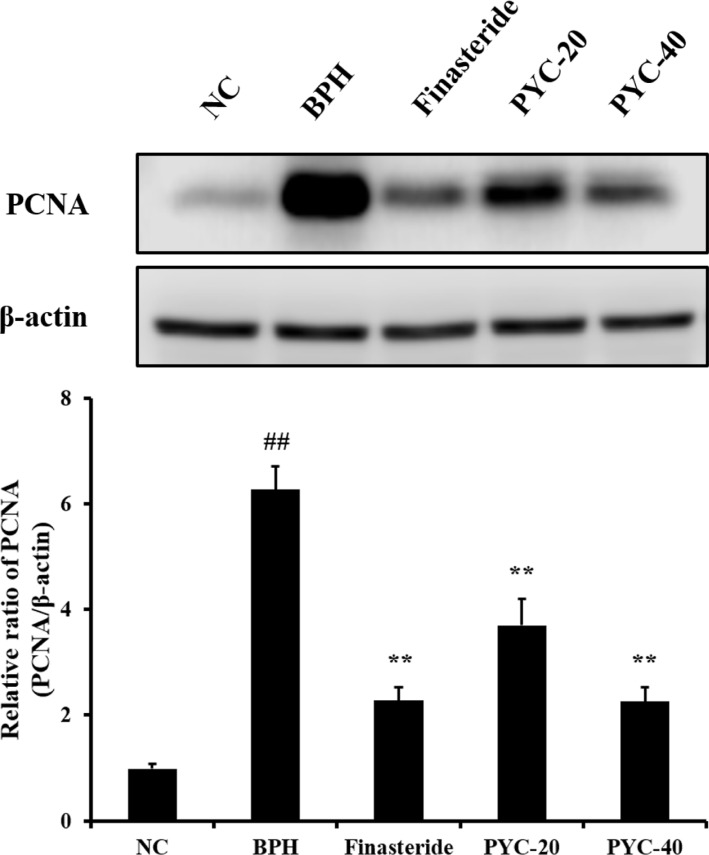
22. Cai HC, Song LB, Zhang GW, Qing XR, Mo DS, Liu W, Zhan XX, Huang YF, Shang XJ. Effects of Xialiqi Capsules on the expressions of PCNA and caspase-3 in rats with benign prostatic hyperplasia. Zhonghua Nan Ke Xue. 2017; 23(8):728–733. PMID:
29726649.
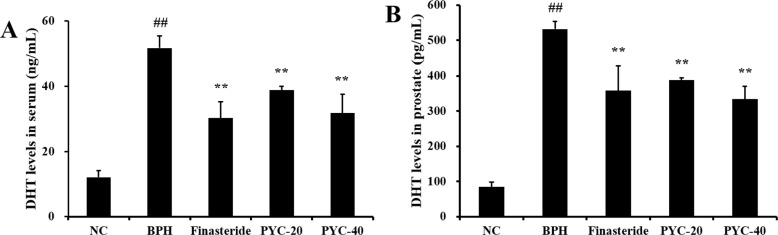
23. Carson C, Rittmaster R. The role of dihydrotestosterone in benign prostatic hyperplasia. Urology. 2003; 61(4 Suppl 1):2–7.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download