Introduction
Streptococcus suis, a gram-positive facultative anaerobe, is an important zoonotic pathogen associated with systemic infections like meningitis, pneumonia, and sepsis, and is frequently associated with hearing loss [
1]. Since the first reported case of human
S. suis infection in Denmark in 1968 [
2], the number of
S. suis infections in humans has increased, particularly in Southeast Asia, and more than 700 cases have been reported worldwide [
3]. All cases of
S. suis infection are reported as sporadic except a few as outbreaks [
3]. In Korea, the first case of human
S. suis infection was reported in 2011 [
4], and four cases have been reported to date with no fatalities [
4567]. We report the first case of life-threatening
S. suis infection in Korea, presenting with severe septic shock and multiple abscesses probably caused by septic emboli. This study was approved by the Institutional Review Board of Bucheon St. Mary's Hospital at the Catholic University of Korea with a waiver of informed consent (Subject number: HC16ZISE0026).
Go to :

Case report
A 60-year-old man visited the emergency department presenting with fever. He had been working on farms and in close contact with swine. Initially, his vital signs were stable except for a fever (up to 39.7°C), and there were no defining abnormal findings in his physical examinations. In addition, no specific findings were present in his laboratory data and urinalysis. There was no active lung lesion in the chest radiograph, and erect abdominal imaging showed mild gas accumulation. Abdominal computed tomography revealed no definite obstructive lesion. As his symptoms improved following hydration and use of analgesics, he was discharged from the hospital.
One day later, he revisited the emergency department for persistent fever, dizziness, and vomiting. He appeared acutely ill and was drowsy. His vital signs were as follows: blood pressure of 70/60 mmHg, heart rate of 52 beats/min, respiratory rate of 20 breaths/min, and body temperature of 36.0°C. Lung sounds were clear, but bowel sounds were decreased. In his laboratory data, leukopenia (white blood cell count, 1.470 × 109/L; neutrophils, 85%; lymphocytes, 14%; monocytes, 1%), thrombocytopenia (platelet count; 40 × 109/L), higher urea nitrogen and creatinine (urea nitrogen, 30.9 mg/dL; creatinine, 3.04 mg/dL), hyperbilirubinemia (total bilirubin; 3.35 mg/dL), and metabolic acidosis (pH, 7.25; pCO2, 30.5 mmHg; bicarbonate, 13.2 mmol/L) were present. The chest radiograph again showed no active lung lesion. Similarly, supine abdominal imaging showed gas accumulation. Erect abdominal imaging was not performed because of the patient's condition. Meropenem and vancomycin were administered as empirical antibiotics after taking a blood sample for bacterial culture. He was then admitted to the intensive care unit for close monitoring.
At six hours of admission, the patient had the following vital signs: blood pressure of 104/48 mmHg, heart rate of 130 beats/min, respiratory rate of 22 breaths/min with continuous infusion of inotropics (dopamine [27 μg/min/kg], norepinephrine [1.7 μg/min/kg]) and low dose corticosteroid (hydrocortisone 100 mg every 8 hours). At 14 hours of admission, generalized tonic-clonic seizure occurred and his peripheral oxygen saturation dropped to <90%, despite oxygen therapy. Endotracheal intubation was performed and the mechanical ventilator was applied. At 16 hours of admission (and 2 hours after mechanical ventilation), his peripheral oxygen saturation was maintained between 95% and 100%. However, his total urine output over those 16 hours was zero despite substantial hydration and use of diuretics. Hence, continuous renal replacement therapy was initiated.
After 12-hour incubation, both aerobic and anaerobic blood cultures (4 bottles total) showed bacterial growth. On hospital day 2, blood cultures revealed the presence of gram-positive cocci. On hospital day 4, the organisms found in the blood cultures were identified as
S. suis using the VITEK 2 system (bioMérieux, Durham, NC, USA). Sequencing PCR of 16S rRNA was performed using the universal primers as previously described [
8]. BLASTN analysis showed that these sequences shared 99% homology with those of
S. suis isolates. Based on antibiotic susceptibility testing results using the VITEK 2 system (susceptible to penicillin, cefotaxime, levofloxacin, vancomycin, and linezolid; resistant to clindamycin, erythromycin, and tetracycline), vancomycin and meropenem were replaced with ampicillin/sulbactam.
The patient's vital signs stabilized after 4 days of treatment. Dopamine and norepinephrine administration were gradually tapered, but drowsiness did not improve. Hydrocortisone was changed to dexamethasone 5 mg/day for prevention of neurologic complications like hearing loss, because we could not completely exclude the possibility of bacterial meningitis.
After 7 days of treatment, ventilator weaning and extubation was done, and continuous renal replacement therapy was stopped. His mental status improved; however, he complained of difficulty in hearing. Otoscopic examination revealed no conclusive abnormal findings in either his tympanic membrane or external auditory canal. Tuning fork examination indicated bilateral sensorineural hearing loss. We performed a spinal tap to evaluate the possibility of meningitis. White blood cell and red blood cell counts from cerebrospinal fluid (CSF) were 7/mm3 and 16/mm3, respectively, and opening pressure was within normal range (80 mmH2O). Glucose levels were not decreased (CSF glucose, 143 mg/dL; serum glucose, 265 mg/dL), but protein levels were higher (125 mg/dL). Dexamethasone treatment was continued (5 mg/day for 3 days, 2.5 mg/day for 3 days, 1 mg/day for 3 days) because his condition was comparable with partially treated S. suis meningitis and subsequent labyrinthitis.
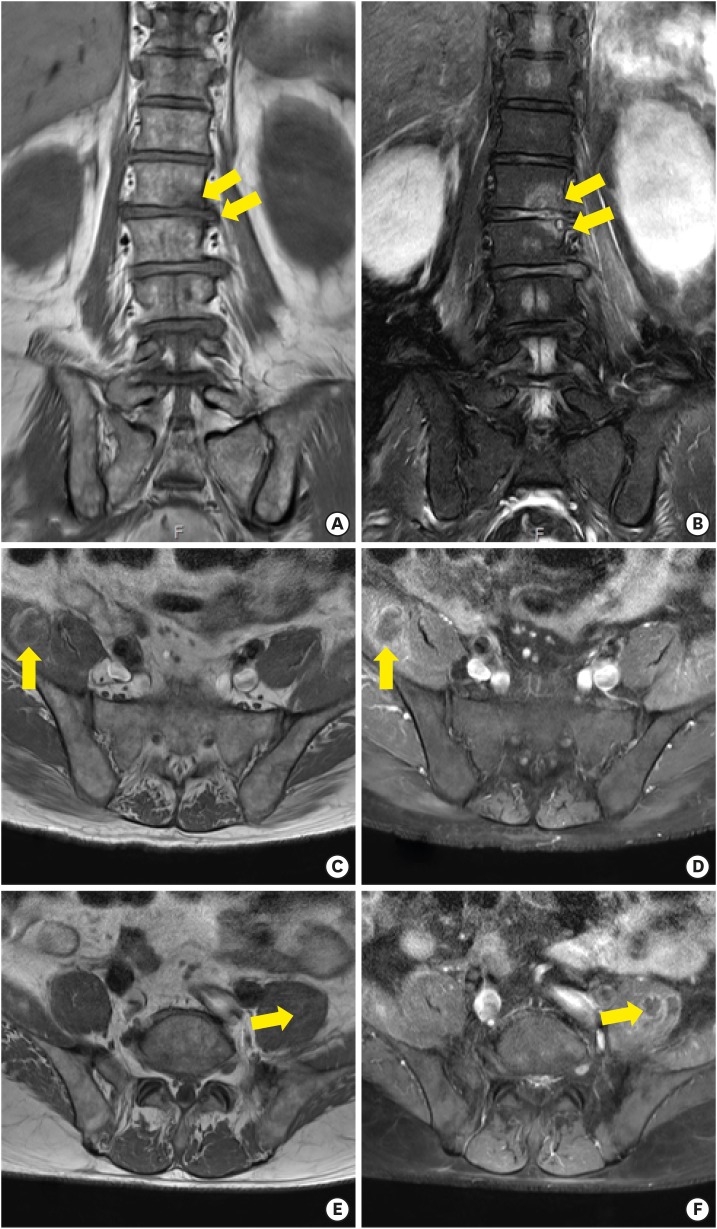
After 10 days of admission, the patient complained of back pain that did not respond to analgesic drugs. Magnetic resonance imaging of the lumbar spine area showed the following: bone marrow signal alteration with end plate irregularity of the left first and second lumbar spine levels; a partially unenhanced lesion in the right iliacus muscle and left iliopsoas muscle, which indicated infective spondylitis of the left first and second lumbar spine levels; and intramuscular abscess formation in the right iliacus muscle and left iliopsoas muscle (
Fig. 1). No neurologic abnormality was noted with his physical examination, and multiple abscesses were located in an area that is not easily accessible percutaneously, so medical treatment (ampicillin/sulbactam) was continued.
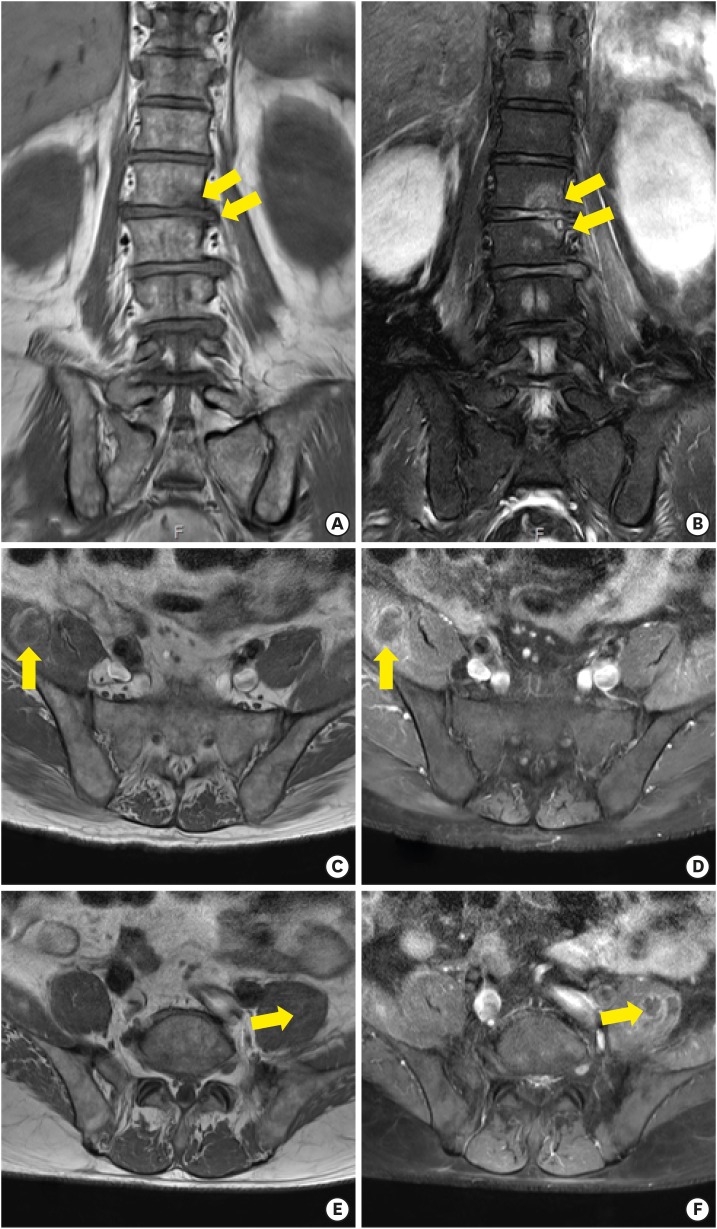 | Figure 1 Lumbar spine MRI of patient. Coronal T2-weighted (A,C,E) and gadolinium-enhanced (B,D,F) images shows bone marrow signal alteration with end plate irregularity of the left first and second lumbar spine levels, which indicated infective spondylitis (A,B). Axial T1-weighted and gadolinium-enhanced images show partially unenhanced lesion in the right iliacus muscle (C,D, arrows) and left iliopsoas muscle (E.F, arrows), which was compatible with intermuscular abscess cavity formation in the right iliacus muscle and left iliopsoas muscle, respectively.
|
The patient was eventually transferred to another hospital for prolonged antibiotic treatment. His back pain improved after completion of a 6-week treatment with antibiotics. As of 2016 (one year since the first visit), he has nearly recovered except for the hearing difficulty, which has him regularly visiting the otolaryngology outpatient department.
Go to :

Discussion
We report a case of
S. suis infection presenting as rapidly progressing severe septic shock of unknown origin, and multiple abscess formation probably caused by septic emboli. Initially, the cause of sepsis was not clear, but we speculated that the port of entry was the gastrointestinal tract. Because
S. suis can be transmitted to humans by ingestion of contaminated raw porcine foods or from cutaneous wounds [
1], it is unsurprising that the patient's initial presentation was determined to be enterocolitis. Moreover, meningitis might have developed from a complication due to primary bacteremia. His decreased mental focus and seizure on the first day of admission could be a manifestation of meningitis. His CSF analysis revealed normal CSF pressure and no definite pleocytosis; however, the CSF sample was obtained 9 days after use of antibiotics suggesting meningitis as an initial manifestation. Further, the occurrence of hearing loss, which is a major complication of
S. suis meningitis, also indicated meningitis.
The most common manifestation of an
S. suis human infection is meningitis; however, other manifestations such as septic arthritis, endocarditis, pneumonia, and peritonitis may occur [
1]. Septic shock was present in 24% of patients infected with
S. suis, and more than 80% of these patients died [
1]. Hearing loss is a frequent complication of
S. suis infection, and it occurs in approximately half of the patients infected with
S. suis [
9]. The cause of hearing loss in patients with
S. suis meningitis is labyrinthitis, and it is distinct from that resulting due to other types of bacterial meningitis like
S. pneumoniae or
Haemophilus influenzae meningitis, for which the cause of hearing difficulty is damage to the auditory nerve [
10]. Dexamethasone is known to reduce hearing loss in
S. suis meningitis [
9]. Unfortunately, hearing difficulty occurred in our patient despite dexamethasone use.
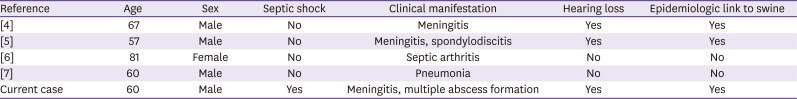
There are only four case reports on human infections due to
S. suis in Korea [
4567]. The patient presented with meningitis in the first case (2011), and with septic arthritis, meningitis and spondylodiscitis, and pneumonia in the other three cases, respectively (
Table 1). Of these patients, hearing loss occurred in two. A unique characteristic of our case was the presence of septic emboli. Septic shock occurs in approximately one quarter of patients with
S. suis infection [
1], but the prevalence of multiple infections by septic emboli is not clearly defined. Case 3 out of all four cases is similar to the present case (
Table 1).
S. suis meningitis was confirmed, and improved after 3 weeks of antibiotics treatment. However, the lumbar spine MRI for evaluation of back pain revealed spondylodiscitis. He was fortunately treated well without the need for surgical management.
Table 1
Summary of five cases of Streptococcus suis infection in Korea.
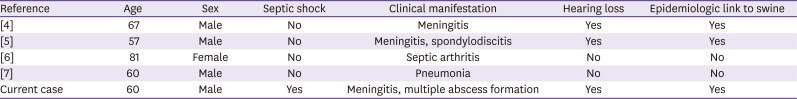
|
Reference |
Age |
Sex |
Septic shock |
Clinical manifestation |
Hearing loss |
Epidemiologic link to swine |
|
[4] |
67 |
Male |
No |
Meningitis |
Yes |
Yes |
|
[5] |
57 |
Male |
No |
Meningitis, spondylodiscitis |
Yes |
Yes |
|
[6] |
81 |
Female |
No |
Septic arthritis |
No |
No |
|
[7] |
60 |
Male |
No |
Pneumonia |
No |
No |
|
Current case |
60 |
Male |
Yes |
Meningitis, multiple abscess formation |
Yes |
Yes |

To date, more than 700 cases of human infection due to
S. suis have been reported worldwide, including a few outbreaks [
1]. An outbreak in the Sichuan province of China during the summer of 2005 was the largest involving 215 patients and 39 deaths (18%) [
11]. Interestingly, an
S. suis infection outbreak in swine had occurred around the same time [
11]. This indicates a relationship between the outbreak of
S. suis infection in humans and that in swine. In Korea, there was no evidence of an outbreak of
S. suis infection in humans until recently; however, outbreaks of
S. suis in swine were already reported [
1213]. To the best of our knowledge, even though research is in progress, there is no
S. suis vaccination available for humans [
1]. Hence, prevention is crucial. Improving swine hygiene methods is the best option for decreasing the chances of
S. suis infection in swine, which can conclusively reduce the possibility of infection in humans. Educating the population is also of critical importance. Those with open wounds should wear gloves when cooking raw pork, and wash their hands after contact to reduce the changes of contracting
S. suis. Moreover, it is recommended that pork should be cooked to reach an internal temperature of 70°C [
1].
Clinicians should consider the possibility of S. suis infection in patients who have a history of contact with swine, including contact with contaminated animals or those who cook with pork. Sometimes it is rapidly progressive, and can lead to sepsis. Finally, it is important to administer dexamethasone for prevention of neurologic complications like hearing loss in S. suis meningitis patients.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download