Abstract
Purpose
To examine the effect of menstrual self-management education program on knowledge and behavior of menstrual self-management in high school girls.
Methods
With a randomized controlled trial, 100 high school girl students were randomly assigned into experimental group and control group. Menstruation self-management program was consisted of a total of four sessions of education program (1 hour of education per session). Control group only received the first class of education. Measurement tools were 20-item menstrual knowledge scale and 12-item women's genito-urinary hygiene scale. Pretest and post-test questionnaires were administered.
Results
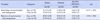
There were significant differences in menstrual knowledge as well as menstrual self-management behavior between the two groups. The experimental group showed significant improvement in both menstrual knowledge score (t=13.37, p<.001) and menstrual self-management behavior score (t=8.38, p<.001) than the control group.
Conclusion
Results of this study suggest that the monthly self-management education program is effective in increasing the knowledge of menstruation of female high school students and enhancing their performance. This program needs to be implemented as a part of high school's standard sex education. Further study is needed to analyze follow-up effects of the program on self-management behavior of students after at least one menstrual cycle.
Figures and Tables
Notes
Summary Statement
▪ What is already known about this topic?
While feminine hygiene for female adolescences is very important for future reproductive health, there is a lack of concern for feminine hygiene and self-care management during menstruation in Korea.
▪ What this paper adds?
This study confirmed that the 4-session menstrual self-management education program was effective in improving the knowledge and enhancing the performance of menstrual self-management.
▪ Implications for practice, education and/or policy
This program needs to be implemented as a part of high school's standard sex education. Further study is needed to analyze follow-up effects of the program on menstrual self-management behavior of students after at least one menstrual cycle.
References
1. Min S, Ki J, Kim J, Kim H, Kim H, Park S, et al. Sex education for teenagers with parents and teachers. Seoul: Korean Sexology Research Association;2016. p. 344.
2. Jogdand K, Yerpude P. A community based study on menstrual hygiene among adolescent girls. Indian J Matern Child Health. 2011; 13(3):1–6.
3. Adinma ED, Adinma JI. Perceptions and practices on menstruation amongst Nigerian secondary school girls. Afr J Reprod Health. 2008; 12(1):74–83.
4. Berhe H, Bayray A, Ukbayohannes R, Getachew G. Menstrual hygiene practice and associated factors among adolescent high school girls. J Bio-Innov. 2016; 5(1):1–15.
5. Santina T, Wehbe N, Ziade F, Nehme M. Assessment of beliefs and practices relating to menstrual hygiene of adolescent girls in Lebanon. Int J Health Sci Res. 2013; 3(12):75–88.
6. Kapoor G, Kumar D. Menstrual hygiene: Knowledge and practice among adolescent school girls in rural settings. Int J Reprod Contracept Obstet Gynecol. 2017; 6(3):959–962. DOI: 10.18203/2320-1770.ijrcog20170564.

7. Ahn S, Cho K. Personal hygiene practices related to genitourinary tract and menstrual hygiene management in female adolescents. Korean J Women Health Nurs. 2014; 20(3):215–224. DOI: 10.4069/kjwhn.2014.20.3.215.

8. Anand E, Singh J, Unisa S. Menstrual hygiene practices and its association with reproductive tract infections and abnormal vaginal discharge among women in India. Sex Reprod Healthc. 2015; 6(4):249–254. DOI: 10.1016/j.srhc.2015.06.001.

9. Kansal S, Singh S, Kumar A. Menstrual hygiene practices in context of schooling: A community study among rural adolescent girls in Varanasi. Indian J Community Med. 2016; 41(1):39–44. DOI: 10.4103/0970-0218.170964.

10. Low N, Chersich MF, Schmidlin K, Egger M, Francis SC, van de, et al. Intravaginal practices, bacterial vaginosis, and HIV infection in women: individual participant data metaanalysis. PLoS Med. 2011; 8(2):e1000416. DOI: 10.1371/journal.pmed.1000416.

11. Bui TC, Thai TN, Tran LT, Shete SS, Ramondetta LM, Basen-Engquist KM. Association between vaginal douching and genital human papillomavirus infection among women in the United States. J Infect Dis. 2016; 214(9):1370–1375. DOI: 10.1093/infdis/jiw388.

12. Na J, Kim Y, Kim H. The effects of systematic health education on health knowledge and health promotion behavior in elementary school students. J Korean Soc Sch Health. 2011; 24(2):173–180.
13. The Education Ministry. School sex education standard for teachers' guide (elementary, middle, and high school). Sejong: Author;2015. p. 1096.
14. Choo Y, Ko H, Kwon H, Kim B, Kim J, Noh Y, et al. Science of sex. 4th ed. Seoul: World Science;2015. p. 361.
15. Kim J. Comparison and analysis on national health education standards for high school in South Korea. J Korean Soc Sch Health. 2016; 2(1):25–40.
16. El-Mowafy RI, Mohamed Moussa MM, El-Ezaby HH. Effect of health education program on knowledge and practices about menstrual hygiene among adolescents girls at orphanage home. IOSR J Nurs Health Sci. 2014; 3(6):48–55.

17. Haque SE, Rahman M, Itsuko K, Mutahara M, Sakisaka K. The effect of a school-based educational intervention on menstrual health: An intervention study among adolescent girls in Bangladesh. BMJ Open. 2014; 4(7):e004607. DOI: 10.1136/bmjopen-2013-004607.

18. Nemade D, Seema A, Gujar R. Impact of health education on knowledge and practices about menstruation among adolescent school girls of Kalamboli, Navi-Mumbai. Health Popul: Perspect Popul. 2009; 32(4):167–175.
19. Su JJ, Lindell D. Promoting the menstrual health of adolescent girls in China. Nurs Health Sci. 2016; 18:481–487.

20. Jun J. Effects of experience based menstrual education program on menstrual attitude and menstrual discomfort among female elementary students [master's thesis]. Busan: Pusan National University;2007. 75.
21. Oh S. The comparison of sex-related knowledge and attitude of 6th-grade elementary school students between the field based learning and the cooperative learning method [master's thesis]. Daejeon: Chungnam National University;2010. 59.
22. Lee Y. Development and effects of nocturnal emission and menstruation education program using CAI for Korean elementary school children [dissertation]. Seoul: Ewha Womans University;2010. 130.
23. Kim J. Effect of heated red bean pillow application for college women with dysmenorrhea. Korean J Women Health Nurs. 2013; 19(2):67–74. DOI: 10.4069/kjwhn.2013.19.2.67.

24. Potur DC, Komurcu N. The effects of local how-dose heat application on dysmenorrhea. J Pediatr Adolesc Gynecol. 2014; 27(4):216–221. DOI: 10.1016/j.jpag.2013.11.003.
25. Park K, Hwang EH, Shin MS, Sul JU. An effect of yoga therapy on relieving dysmenorrhea: RCTs (randomized controlled trials) review. Korean J Orient Prev Med. 2011; 15(2):39–49.
26. Czerwinski BS. Variation in feminine hygiene practices as afunction of age. J Obstet Gynecol Neonatal Nurs. 2000; 29(6):625–633.
27. Ahn S. Feminine hygiene and vaginal douche practices in middle-aged women. Korean J Women Health Nurs. 2013; 19(4):285–294. DOI: 10.4069/kjwhn.2013.19.4.285.

28. Rothman KJ, Funch DP, Alfredson T, Brady J, Dreyer NA. Randomized field trial of vaginal douching, pelvic inflammatory disease and pregnancy. Epidemiology. 2003; 14(3):340–348.

29. Kim Y, Park U. The effects of health education on health knowledge and health promoting behaviors in elementary school students. J Korean Soc Sch Health. 2013; 26(2):55–61.
30. Kim K. Amos 18.0, analysis structural equation modeling. Seoul: Hannarae Academy;2010. p. 600.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download