Abstract
Pulmonary extraintestinal manifestation is rare in Crohn's disease and has been reported in only a few cases. Despite the presence of pulmonary abnormalities in a significant proportion of patients with inflammatory bowel disease, there are only few case reports, due to complicated diagnosis and low recognition by clinicians. Currently, treatment guidelines for pulmonary Crohn's disease have not been established. There are some case reports of pulmonary Crohn's disease that achieved remission after infliximab treatment. Clinical and radiological remission of pulmonary extraintestinal involvement in Crohn's disease after adalimumab therapy has not been reported yet. Here, we report one case of lung involvement of Crohn's disease, which shows radiological and clinical remission after adalimumab treatment.
Crohn's disease is a chronic systemic disease that is associated with various extraintestinal manifestations (EIM). EIM of Crohn's disease are known to be associated with 20–40% of cases.1 However, the incidence and prevalence of pulmonary involvement with Crohn's disease are variable in the literature and may be as low as 0.4%.2 As pulmonary involvement of Crohn's disease is rare, there are no established therapeutic guidelines. In some case series reviews, infliximab treatment resulted in clinical and radiographic resolution of pulmonary EIM.3 However, there have been no reports of improvement of pulmonary EIM after adalimumab monotherapy. Here, we present a very rare case of pulmonary involvement with Crohn's disease, which was recovered with adalimumab treatment.
A 35-year-old woman visited National Health Insurance Service Ilsan Hospital with a 7 day history of pleuritic chest pain. She had been diagnosed with Crohn's disease 2 years prior. At that time, she had suffered from lower abdominal pain, diarrhea, and hematochezia. Initial colonoscopy findings showed multiple longitudinal ulcers invading the entire colon, which is compatible with Crohn's disease. The microscopic histopathology of the colon showed cryptitis and crypt abscesses with ill-defined non-caseating granulomas, which are consistent with Crohn's disease. Her Crohn's disease Activity Index (CDAI) score was 365 points at diagnosis. Initially, she had been treated with 5-aminosalicylic acid. During treatment, her CDAI scores were maintained at below 80 points. However, the patient again developed symptoms of diarrhea and lower abdominal pain after 1 year. Her CDAI score was 293 points. Colonoscopy revealed erythematous, longitudinal ulcers, and a cobblestone appearance, consistent with active Crohn's disease. Intravenous administration of Infliximab (5 mg/kg) was added to her treatment regimen. The patient responded to infliximab therapy initially. However, infliximab had to be shifted to adalimumab administered every other week due to loss of response to infliximab after 6 months from initial injection. Adalimumab treatment was also discontinued after 2 months, as the patient refused maintenance therapy due to her desire for pregnancy. She had not been on adalimumab therapy for 10 weeks until initial symptoms of pleuritic chest pain occurred. She had no remarkable family history. Upon physical examination, blood pressure was 101/61 mmHg, body temperature was 36.7℃, and heart rate was 94 beats/min. Neck and chest examination showed no abnormal findings. Tenderness and hepatosplenomegaly were not observed in abdominal examination. Laboratory data revealed a hemoglobin level of 12.6 g/dL, white blood cell count of 1.011×1010/L, platelet count of 353,000/mm3, aspartate aminotransferase level of 14 IU/L, alanine aminotransferase level of 13 IU/L, total bilirubin level of 0.40 mg/dL, albumin level of 3.7 g/dL, blood urea nitrogen level of 11.3 mg/dL, and creatinine level of 0.71 mg/dL. The serum level of CRP was slightly increased by 1.86 mg/dL (normal range, 0–0.8 mg/dL), and erythrocyte sedimentation rate was 61 mm/hr (normal range, 0–20 mm/hr). There were no abnormal findings in the chest X-ray. Chest CT revealed multiple pulmonary necrobiotic nodules on both lung fields (Fig. 1). Colonoscopic examination showed multiple longitudinal ulcers with edematous changes and perianal involvement, which are compatible with active Crohn's disease (Fig. 2). Abdominal CT showed multifocal wall thickening of the rectum and sigmoid colon. The results of three consecutive sputum acid fast bacillus smear and stain examinations turned out to be negative. Anti-neutrophil cytoplasmic antibody testing revealed a negative response. Considering the possibility of combined high metabolic lesions, whole body positron emission tomography CT scan was carried out. Multiple small-sized ill-defined pulmonary nodules in bilateral lung fields with high fluorodeoxyglucose uptake of 3.88 to 8.88 peak standardized uptake value were observed on positron emission tomography CT (Fig. 3).
Surgical biopsy was required since malignancy could not be excluded. Thoracoscopic lung wedge resection was performed for diagnosis. In the surgical field findings, a whitish patch-like mucous-shaped lesion was observed in the left upper lobe surface area, and wedge resection was performed in the target area (Fig. 4A). In gross examination of the surgical specimen, multiple necrotic lesions were noted (Fig. 4B). Necrotizing granulomatous inflammation with parenchymal geographical necrosis was detected in the biopsy specimen (Fig. 5A, B). Organizing pneumonia was observed in a certain section of the tissue compartment (Fig. 5C). The results of tuberculosis polymerase chain reaction and interferon-γ release assays were negative. Based on the patient's underlying disease, imaging, and pathological findings, the possibility of pulmonary EIM from Crohn's disease was considered. Adalimumab therapy had been administered 10 times biweekly. Mycobacterial culture results at 6 and 8 weeks reported no growth.
At the 5 month follow-up visit, the patient did not have any clinical symptoms. The chest CT findings showed that the previously observed ill-defined pulmonary nodules had decreased significantly (Fig. 6). Radiologic and clinical remissions were confirmed.
Pulmonary EIM of Crohn's disease are considered as rare manifestations despite increasing evidence suggesting frequent pulmonary involvement.4 As the association between inflammatory bowel disease (IBD) and pulmonary involvement has not been well established, clinicians may underdiagnose pulmonary involvement in IBD patients.5 Similarities in disease pathogenesis and the sharing of important environmental risk factors and genetic susceptibility suggest that there is complex interplay between IBD and airway diseases.6 Gut-associated lymphoid tissue shares some commonality in adhesion molecules necessary for homing of leukocytes to the mucosa with bronchiolar-associated lymphoid tissue.5 However, the exact mechanism behind the link between lung and bowel abnormalities has not been clearly revealed.
According to reported case series and review articles, pulmonary EIM present a broad spectrum of pathological and radiological features.37 Imaging findings include multifocal patchy consolidation or ground-glass opacity with a subpleural or bronchovascular as well as mid to lower lung predominant distribution.8 However, according to the case series review, radiographic findings of pulmonary involvement with Crohn's disease showed various patterns without any definite specific findings.3 There are no definite specific pathologic findings in distinguishing pulmonary EIM of Crohn's disease from other etiologies. Necrobiotic lung nodules that pathologically resemble those in rheumatoid arthritis (lung) and pyoderma gangrenosum (skin) have been described but are rare.8 Necrotizing granulomatous inflammation with parenchymal geographical necrosis and organizing pneumonia detected in this case are known to be compatible with pulmonary EIM of Crohn's disease. In the lung pathology of this case, typical findings of necrotizing vasculitis often detected in Wegener granulomatosis were not observed. However, these findings are not unique to lung involvement of Crohn's disease. These histologic findings may also be present in vasculitis such as Wegener granulomatosis or pulmonary tuberculosis.910 Pathological reports without typical findings are not rare in the case of pulmonary Crohn's disease.23 Therefore, it is difficult to confirm pulmonary EIM of Crohn's disease with only pathological findings.
The pulmonary EIM of Crohn's disease are difficult to diagnose since not only radiologic findings with pathologic reports but also clinical context should be considered. In addition, pulmonary EIM of Crohn's disease do not always present in textbook fashion.2 In order to diagnose pulmonary EIM, a comprehensive approach may be required, considering following factors and clinical presentations of the patient. 1) Radiological findings; 2) pathological reports; 3) results of endoscopy; 4) tailored laboratory data based on clinical situations such as anti-neutrophil cytoplasmic antibody, interferon-γ release assays, tuberculosis polymerase chain reaction, serum ACE (angiotensin-converting enzyme) level, etc.; and 5) treatment response.
As the spectrum of pathological and radiological patterns is broad, infection, especially tuberculosis, and drug-related changes should be considered in the differential diagnosis.11 In general, anti-tumor necrosis factor therapy is highly effective for EIM, except for primary sclerosing cholangitis.12 However, pulmonary EIM are extremely rare, and there are not enough accumulated cases to establish standardized treatment guidelines. Eight cases of pulmonary EIM with Crohn's disease treated by infliximab were discovered through a literature review by Hayek et al.3 All cases responded to infliximab therapy, resulting in clinical and radiographic resolution of the pulmonary IBD EIM.313 In the case of pulmonary EIM, a graded mixture of inhaled and oral corticosteroids can be also used, based on the nature of pulmonary involvement.14 However, no corticosteroid was used in this case since concurrent infection could not be excluded. In this case, adalimumab monotherapy was used to treat pulmonary EIM of Crohn's disease. According to a recent report, adalimumab is effective for achieving initial and durable resolution of all EIM of Crohn's diasease.15 Adalimumab monotherapy does not seem to be inferior compared to a combination of adalimumab with other immunomodulators for induction and maintenance of remission and response with regards to Crohn's disease.16 It is an unprecedented case of pulmonary Crohn's disease in which clinical and radiological remission has been achieved through adalimumab monotherapy.
In conclusion, we present a case of Crohn's disease with pulmonary EIM that resulted in radiological and clinical remission after adalimumab treatment. Considering anti-tumor necrosis factor treatment such as adalimumab and infliximab, infectious etiologies should be excluded through meticulous and tailored evaluations. When radiological abnormalities such as incidental lung nodules are detected in patients with Crohn's disease, pulmonary EIM should be included in differential diagnosis lists in addition to infections and malignancies.
Figures and Tables
Fig. 1
Chest CT findings revealed multiple ill-defined pulmonary nodules (arrows) in bilateral lung fields. CT, computed tomography.

Fig. 2
Colonoscopy findings showing multiple various sized longitudinal ulcers and perianal ulcers with edematous changes.
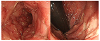
Fig. 3
PET-CT showed multiple various sized ill-defined pulmonary nodules (arrows) with highly increased 18F-FDG uptake (pSUV 3.67–8.88). PET, positron emission tomography; CT, computed tomography; 18F-FDG, fluorine-18 fluorodeoxyglucose; pSUV, peak standardized uptake value.

Fig. 4
(A) The surgical field observed by video-assisted thoracoscopy showing whitish mucous patch-like lesion (arrow). (B) Two ill-demarcated necrotic lesions (arrows) are shown on gross photograph after thoracic wedge resection.

References
1. Lakatos PL, Lakatos L, Kiss LS, Peyrin-Biroulet L, Schoepfer A, Vavricka S. Treatment of extraintestinal manifestations in inflammatory bowel disease. Digestion. 2012; 86:Suppl 1. 28–35.

2. Chew MT, Chak E, Matsukuma K. A rare cause of pulmonary nodules. Case Rep Gastroenterol. 2016; 10:633–639.

3. Hayek AJ, Pfanner TP, White HD. Inflammatory bowel disease of the lung: the role of infliximab? Respir Med Case Rep. 2015; 15:85–88.

4. Black H, Mendoza M, Murin S. Thoracic manifestations of inflammatory bowel disease. Chest. 2007; 131:524–532.

5. Songür N, Songür Y, Tüzün M, et al. Pulmonary function tests and high-resolution CT in the detection of pulmonary involvement in inflammatory bowel disease. J Clin Gastroenterol. 2003; 37:292–298.
6. Vutcovici M, Brassard P, Bitton A. Inflammatory bowel disease and airway diseases. World J Gastroenterol. 2016; 22:7735–7741.

7. Lu DG, Ji XQ, Liu X, Li HJ, Zhang CQ. Pulmonary manifestations of Crohn's disease. World J Gastroenterol. 2014; 20:133–141.

8. Olpin JD, Sjoberg BP, Stilwill SE, Jensen LE, Rezvani M, Shaaban AM. Beyond the bowel: extraintestinal manifestations of inflammatory bowel disease. Radiographics. 2017; 37:1135–1160.

9. Yoon HS, Lee EJ, Lee JY, Chon GR, Lee SH, Kim SJ. Organizing pneumonia associated with M ycobacterium tuberculosis infection. Respirol Case Rep. 2015; 3:128–131.
10. Vaszar LT, Orzechowski NM, Specks U, et al. Coexistent pulmonary granulomatosis with polyangiitis (Wegener granulomatosis) and Crohn disease. Am J Surg Pathol. 2014; 38:354–359.

11. Majewski S, Piotrowski W. Pulmonary manifestations of inflammatory bowel disease. Arch Med Sci. 2015; 11:1179–1188.

12. Ardizzone S, Puttini PS, Cassinotti A, Porro GB. Extraintestinal manifestations of inflammatory bowel disease. Dig Liver Dis. 2008; 40:Suppl 2. S253–S259.

13. Pedersen N, Duricova D, Munkholm P. Pulmonary Crohn's disease: a rare extra-intestinal manifestation treated with infliximab. J Crohns Colitis. 2009; 3:207–211.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download