Abstract
Background
Helicobacter pylori infection in children causes gastrointestinal symptoms and iron deficiency anemia. This study aimed to investigate trends in H. pylori stool antigen (HpSA) positivity in children and the relationship between HpSA test results and anemia.
Methods
We analyzed the results of 2,762 HpSA tests and the correlation of hemoglobin and ferritin with HpSA in patients aged 0–18 years from 2008 to 2014 at a tertiary care center. Additionally, we prospectively evaluated HpSA test results and correlation with hemoglobin in 352 specimens obtained from five centers.
Results
From 2008-2014, the mean positive rate of the HpSA test was 5.8%, with a high of 9.1% in 2012 and a low of 2.3% in 2013. The positive rate correlated with age: 2.9% in 0–6-year-olds, 5.8% in 7–12-year-olds, and 10.6% in 13–18-year-olds (P<0.0001). There was no difference in HpSA positivity in patients with (7.0%) and without (5.7%) anemia. Ferritin was significantly lower in patients with positive HpSA results than in those with negative results (P=0.0001). In a multicenter study, the positive rate of HpSA was 16.8%.
Conclusion
The rate of HpSA positivity was 5.8% in pediatric patients at a single center from 2008–2014, and this rate increased with age. Helicobacter pylori infection may be associated with iron deficiency, as ferritin level was significantly lower in HpSA-positive patients than HpSA-negative patients.
Figures and Tables
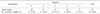
 | Fig. 1Helicobacter pylori stool antigen result by age from 2008 to 2014 in a tertiary care hospital. H. pylori stool antigen was tested by ELISA. |
References
1. NIH Consensus Conference. Helicobacter pylori in peptic ulcer disease. NIH consensus development panel on Helicobacter pylori in peptic ulcer disease. JAMA. 1994; 272:65–69.
2. Song JH, Kim JJ. Helicobacter pylori infection. J Korean Med Assoc. 2006; 49:1017–1025.
3. Kim JH. The diagnosis of Helicobacter pylori infection. Korean J Helicobacter Up Gastrointest Res. 2014; 14:233–236.
4. da Silva-Etto JMK, Mattar R, Villares-Lopes CA, Marques SB, Carrilho FJ. Evaluation of diagnostic accuracy of two rapid stool antigen tests using an immunochromatographic assay to detect Helicobacter pylori. Clin Biochem. 2017; 50:959–962.
5. Fagan RP, Dunaway CE, Bruden DL, Parkinson AJ, Gessner BD. Controlled, household-randomized, open-label trial of the effect of treatment of Helicobacter pylori infection on iron deficiency among children in rural Alaska: results at 40 months. J Infect Dis. 2009; 199:652–660.
6. Baysoy G, Ertem D, Ademoglu E, Kotiloglu E, Keskin S, Pehlivanoglu E. Gastric histopathology, iron status and iron deficiency anemia in children with Helicobacter pylori infection. J Pediatr Gastroenterol Nutr. 2004; 38:146–151.
7. Hershko C, Ianculovich M, Souroujon M. A hematologist's view of unexplained iron deficiency anemia in males: impact of Helicobacter pylori eradication. Blood Cells Mol Dis. 2007; 38:45–53.
8. Malope BI, MacPhail AP, Alberts M, Hiss DC. The ratio of serum transferrin receptor and serum ferritin in the diagnosis of iron status. Br J Haematol. 2001; 115:84–89.

9. Jang KM, Choe BH, Choe JY, Hong SJ, Park HJ, Chu MA, et al. Changing prevalence of Helicobacter pylori infections in Korean children with recurrent abdominal pain. Pediatr Gastroenterol Hepatol Nutr. 2015; 18:10–16.
10. Kim JH, Kim HY, Kim NY, Kim SW, Kim JG, Kim JJ, et al. Seroepidemiological study of Helicobacter pylori infection in asymptomatic people in South Korea. J Gastroenterol Hepatol. 2001; 16:969–975.
11. Cullen DJ, Collins BJ, Christiansen KJ, Epis J, Warren JR, Surveyor I, et al. When is Helicobacter pylori infection acquired? Gut. 1993; 34:1681–1682.
12. Banatvala N, Mayo K, Megraud F, Jennings R, Deeks JJ, Feldman RA. The cohort effect and Helicobacter pylori. J Infect Dis. 1993; 168:219–221.
13. Peleteiro B, Bastos A, Ferro A, Lunet N. Prevalence of Helicobacter pylori infection worldwide: a systematic review of studies with national coverage. Dig Dis Sci. 2014; 59:1698–1709.
14. Dalla Nora M, Hörner R, De Carli DM, Rocha MP, Araujo AF, Fagundes RB. Is the immunochromatographic fecal antigen test effective for primary diagnosis of Helicobacter pylori infection in dyspeptic patients? Arq Gastroenterol. 2016; 53:224–227.
15. Jekarl DW, Kim JK, Lee HK, Sung JH, Kim H, Cho EJ, Kim Y, Park YJ. Clinical evaluation of BioTracer™ H.pylori Rapid card and BioTracer™ H.pylori Ag Rapid Card. Ann Clin Microbiol. 2017; 20:S119.
16. Choe YH, Kim SK, Hong YC. Helicobacter pylori infection with iron deficiency anaemia and subnormal growth at puberty. Arch Dis Child. 2000; 82:136–140.
17. Choe YH, Kim SK, Hong YC. The relationship between Helicobacter pylori infection and iron deficiency: seroprevalence study in 937 pubescent children. Arch Dis Child. 2003; 88:178.
18. Seo JK, Ko JS, Choi KD. Serum ferritin and Helicobacter pylori infection in children: a sero-epidemiologic study in Korea. J Gastroenterol Hepatol. 2002; 17:754–757.
19. Son MH, Yeom JS, Park JS, Park ES, Seo JH, Lim JY, et al. Relationship between Helicobacter pylori infection and irondeficiency anemia in infants and children. Korean J Pediatr. 2009; 52:544–548.
20. Patel SK, Pratap CB, Jain AK, Gulati AK, Nath G. Diagnosis of Helicobacter pylori: what should be the gold standard? World J Gastroenterol. 2014; 20:12847–12859.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download