Abstract
This report presents a case of cervical pneumatocysts as an incidental finding on cone-beam computed tomography. Pneumatocysts are gas-containing lesions of unknown etiology. They usually present in the ilium or sacrum, adjacent to the sacroiliac joint. In the literature, 21 case reports have described cervical pneumatocysts. Cervical pneumatocysts should be differentiated from other lesions, such as osteomyelitis, osteonecrosis, and neoplasms, as well as post-traumatic and post-surgical cases. Computed tomography, cone-beam computed tomography, and magnetic resonance imaging are appropriate tools to diagnose cervical pneumatocysts.
Intraosseous cervical pneumatocysts are rare, asymptomatic benign lesions incidentally found on radiographs. These lesions commonly involve the iliac or sacral bone and are rarely visible on the cervical spine.1 Vertebral pneumatocysts are most commonly seen in the location of spondylosis in adults.2 Awareness of these characteristic features can help radiologists distinguish pneumatocysts from osseous lesions.1 The etiology of pneumatocysts is unknown, but they have been claimed to be caused by the accumulation of nitrogen gas.3 Intraosseous gas collection is a phenomenon of the bone that occurs in various conditions, including osteomyelitis, trauma, neoplasm, and osteonecrosis.45 The most common cause of intraosseous gas collection in the vertebral bodies is the presence of intraosseous pneumatocysts.6 The appearance of pneumatocysts in the cervical spine is uncommon, and 21 cases have been reported in the literature.7 Recent studies have proven that cervical lesions are more common2 than reported; therefore, meticulous radiographic evaluation will allow such lesions to be identified. Cone-beam computed tomography (CBCT) is predominantly used to diagnose dental abnormalities, as well as aiding in the evaluation of structures such as the temporomandibular joint, paranasal sinus, upper cervical vertebrae, the base of the skull, and the pharyngeal airspace. It is more likely that dentists will encounter pneumatocyst-like lesions in the cervical spine while interpreting diagnostic radiographs.8 Medium and large fields of view are the image volumes that enable diagnosticians to identify incidental findings of the cervical spine on CBCT.8
This report presents a case with 8 lytic lesions in the cervical vertebrae (C2–C5) diagnosed incidentally when a patient presented for dental implant treatment planning.
A 60-year-old female patient was referred for a CBCT scan to the Oral and Maxillofacial Imaging Center of the University of Texas School of Dentistry at Houston for an evaluation of the anterior maxilla for dental implant treatment planning. The patient's medical history was positive for a benign brain tumor and visual impairment. The standard Imaging Center protocol was requested for CBCT scanning and interpretation, which consisted of a medium field of view (9 cm×15 cm, 200-μm voxels) at 90 kVp and 10 mA. The scan was acquired on a Kodak 9500 CBCT unit (Carestream Health, Rochester, NY, USA) and the scan was retrieved on an InVivo-5.0 DICOM viewer (Anatomage Inc., San Jose, CA, USA). The CBCT volume revealed multiple radiolucencies with sclerotic margins on C2–C5 that measured approximately 2–10 mm (Figs. 1, 2, 3, 4, 5, 6). The radiolucencies were primarily located on the lamina, adjacent to the facet joints and close to the endplates. No destruction of the adjacent bone or extension into the intervertebral space was evident. The pixel intensity values ranged from −750 to −1000, indicating gas density. Eight lytic lesions were revealed on the CBCT scan. Cystic-appearing radiolucencies on the cervical vertebrae can be associated with a wide spectrum of conditions, and lytic metastasis, subchondral cysts, osteoarthritis, and other analogous conditions were considered in the differential diagnosis. The benign-appearing radiographic appearance and range of pixel intensity values were pathognomonic of intravertebral gas formation and suggestive of cervical pneumatocysts.
Pneumatization of bone commonly occurs in the craniofacial bones irrespective of age, gender, and race. Intraosseous lesions are diagnosed in conditions such as osteomyelitis, trauma, irradiated neoplasms, intraosseous ganglia, osteonecrosis, methyl methacrylate prosthesis, and postoperative conditions.9
Cervical pneumatocysts are very rare; so far, 21 cases have been reported in the literature.8 On computed tomography, pneumatocysts appear as lytic low-density lesions of variable dimension. These lytic lesions show attenuation values of −950 to −580 Hounsfield units (HU), which is pathognomonic of pneumatocysts.10 Intraosseous pneumatocysts are benign lesions and require no specific treatment, although growing lesions may need to be monitored if they pose a risk of fracture.10
Ramirez et al.11 first described an intraosseous pneumatocyst with an unknown etiology in 1984; this benign lesion consisted predominantly of nitrogen gas. Although they are more common in the sacroiliac joint, intraosseous pneumatocysts have occasionally been reported to be present in the vertebrae, humeral head, clavicle, cervical rib, scapula, acetabulum, and pubis.5 Many authors have reported that pneumatocysts did not progress in size. However, Nakayama et al.13 stated that pneumatocysts in the cervical spine and lumbar spine suddenly progressed to fluid-filled cysts 6–16 months after the initial presentation. In the case reported by Yamamoto et al.,5 the pneumatocysts resolved spontaneously and appeared as fluid-filled cysts on follow-up imaging.
Kitagawa et al.4 reported a case of growing cervical pneumatocysts, while the study conducted by Matsukubo et al.14 reviewed 500 neck computed tomography exams and found multiple lytic lesions on the cervical spine, with most occurrences in the C4–C7 segment. The present report describes the incidental finding of multiple intraosseous cervical pneumatocysts involving the C2–C5 segment in a 60-year-old female patient referred for CBCT imaging for dental implant treatment planning. Intraosseous pneumatocysts are gas-filled cystic cavities, and the exact cause of the development of these cavities is unknown. Karasick et al.14 suggested that the source of gas might be from the intervertebral disc through the vertebral endplate, although the gas inside pneumatocysts is mostly composed of nitrogen. Some authors have proposed that negative pressure within the lesion causes the release of nitrogen from the surrounding soft tissues or articular joints.713 In the degenerated spine, gas often accumulates in the intervertebral discs, which is known as the vacuum phenomenon. This phenomenon results from the extension of gas through the defect from the intervertebral disc into the vertebral body, and it causes intravertebral pneumatocysts.7 The spontaneous progression of vertebral intraosseous pneumatocysts could result in fluid-filled cysts.7
In the case reported by Kitagawa et al.,4 direct communication was observed between the intervertebral disc and pneumatocysts on C6. In our case, no such direct communication was observed. The lesions described in this report showed variable dimensions, with largest being approximately 10 mm.4 In our case, the pneumatocysts were primarily seen in the lamina of the cervical vertebra and were adjacent to the facet joints, with minimal degenerative changes on osseous portions of the cervical spine. Since CBCT utilizes pixel intensity values, which closely resemble HU values, all the lesions in our case showed gas attenuation, with pixel intensity values ranging from −1000 to −750. Osteolytic lesions, such as those seen in metastatic lesions, osteomyelitis, and osteonecrosis, should be differentiated from pneumatocysts by their radiographic appearance and gas attenuation characteristics through computed tomography and CBCT.
In conclusion, CBCT has revolutionized dentistry over the last decade, with multiple applications that range from diagnosis to treatment planning. More incidental findings are emerging as CBCT technology advances. It is therefore imperative to report such instances to educate our peers in the dental world and, at the same time, to understand the liability associated with CBCT scan findings during the routine practice of dentistry. Our case report presented innocuous benign lesions seen on an CBCT exam. Although these lesions did not warrant further medical treatment, follow-up imaging may still be needed to assess their expansion potential. Vertebral pneumatocysts are uncommon, but predominantly occur in the cervical spine in patients with degenerative disc disease. They may appear as possible metastatic lesions on plain radiographs, but CBCT, in combination with further consultations with specialists, can confirm the nature of these lesions.
Disclosure: This case report was submitted and presented at the annual American Academy of Oral and Maxillofacial Academy meeting, and the abstract has been published in the journal Oral Surgery, Oral Medicine, Oral Pathology, and Oral Radiology.
Figures and Tables
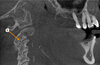
Fig. 1
Sagittal cone-beam computed tomographic image shows cystic lesions (#1 and #2) with sclerotic margins on C-2 and C-4.
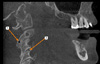
Fig. 2
Sagittal cone-beam computed tomographic image shows a large cystic lesion (#3) with sclerotic margins on the right lateral mass of C-3.

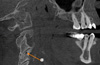
Fig. 3
Sagittal cone-beam computed tomographic image shows a small cystic lesion (#4) with sclerotic margin on the left lateral mass of C-3.
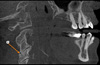
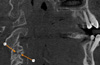
Fig. 4
Sagittal cone-beam computed tomographic image shows a small cystic lesion (#5) with sclerotic margins on C-4.
References
1. Sen D, Satija L, Saxena S, Rastogi V, Singh M. Intraosseous pneumatocyst of the cervical vertebra. Med J Armed Forces India. 2015; 71:380–383.

2. Matsukubo Y, Kashiwagi N, Uemura M, Tatsumi S, Takahashi H, Hyodo T, et al. Intravertebral pneumatocysts of the cervical spine. Neuroradiology. 2013; 55:1341–1344.

3. Coşar M, Eser O, Aslan A, Korkmaz S, Boyaci G, Değirmenci B, et al. Vertebral body pneumatocyst in the cervical spine and review of the literature. Turk Neurosurg. 2008; 18:197–199.
4. Kitagawa T, Fujiwara A, Tamai K, Kobayashi N, Saiki K, Omata S, et al. Enlarging vertebral body pneumatocysts in the cervical spine. AJNR Am J Neuroradiol. 2003; 24:1707–1710.
5. Yamamoto T, Yoshiya S, Kurosaka M, Nagira K, Takabatake M, Hamamoto H, et al. Natural course of an intraosseous pneumatocyst of the cervical spine. AJR Am J Roentgenol. 2002; 179:667–669.
6. Arslan G, Ceken K, Cubuk M, Ozkaynak C, Luleci E. Vertebral pneumatocysts. Acta Radiol. 2001; 42:20–23.

7. Sunder S, Prasad R. Vertebral body pneumatocyst in the cervical spine - a case report. Apollo Med. 2008; 5:121–124.
8. Husain MA, Tetradis S, Mallya SM. Intraosseous pneumatocysts of the cervical spine: a report of four cases and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015; 119:e49–e54.

9. Laufer L, Schulman H, Hertzanu Y. Vertebral pneumatocyst. A case report. Spine (Phila Pa 1976). 1996; 21:389–391.
10. Renshaw H, Patel A, Boctor DS, Hakmi MA. ‘Abnormal’ cervical imaging?: Cervical pneumatocysts - a case report of a cervical spine pneumatocyst. J Orthop. 2015; 12:Suppl 1. S83–S85.

11. Ramirez H Jr, Blatt ES, Cable HF, McComb BL, Zornoza J, Hibri NS. Intraosseous pneumatocyst of the ilium. Findings on radiographs and CT scans. Radiology. 1984; 150:503–505.
12. Oehler E, Valour F, Pascart T. Intraosseous pneumatocysts: a case based review. Clin Rheumatol. 2013; 32:129–134.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download