Abstract
Purpose
Changes in angular deviation before and after general anesthesia and strabismus surgery were examined.
Methods
Twenty patients with intermittent exotropia who were operated on by the same surgeon from January 2014 to October 2017 were included. The basic angle of deviation (preoperative angle of deviation, PreAn) was measured at an outpatient clinic. While lying on a surgical bed under general anesthesia, the bispectral index was referenced, and it was confirmed that there was a sufficient degree of sedation. Photographs were then taken at a height of 40 cm (angle of deviation under general anesthesia, PostAn); while still under general anesthesia, the same procedure was followed immediately after the end of surgery. At 6 months after surgery, the angle of deviation was measured.
Results
There were 10 males and 10 females, and the mean age was 7.31 ± 3.59 years. The preoperative angle of deviation was 30.0 ± 13.87 prism diopters (PD) at far fixation; under general anesthesia, 26.46 ± 5.39 PD. There was a significantly positive correlation between the PreAn and angle of deviation under general anesthesia (PostAn - PreAn = −7.67 × PreAn + 19.57; R2 = 0.872; p < 0.00). The angle of deviation changes between pre- and post-anesthesia (PostAn-PreAn) and at the end point of surgery (OP end) and at 6 months after surgery (6mon) also showed a significantly positive correlation (6mon-OP end = 0.317 × [PostAn - PreAn] + 13.098; R2 = 0.334; p = 0.01).
Conclusions
There was a significant positive correlation between the measured angle of deviation pre- and post-anesthesia. We could estimate the degree of change between the angle of deviation immediately after surgery and the stable angle according to the degree of deviation before and after general anesthesia.
Figures and Tables
 | Figure 1Schematic illustration showing the angle of deviation in the surgical plane of general anesthesia. The changed angle is calculated by this formula (from Ku et al.4). |
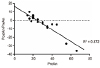 | Figure 2Relationship between the PreAn and PostAn-PreAn, expressed as a linear regression with simple scatter dots and fit line. PostAN-PreAn = −7.67 × PreAn + 19.57 (R2 = 0.872, p<0.00). PreAn = preoperative angle of deviation; PostAn = angle of deviation under general anesthesia. |
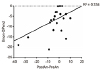 | Figure 3Relationship between the PostAn-PreAn and 6mon-OP end, expressed as a linear regression with simple scatter dots and fit line. 6mon-OP end = 0.317 × (PostAn-PreAn) + 13.098 (R2 = 0.334, p = 0.01). PreAn = preoperative angle of deviation; PostAn = angle of deviation under general anesthesia; 6mon = angle of deviation at 6th month after strabismus operation; OP end = angle of deviation before waking from general anesthesia after strabismus surgery. |
Notes
References
1. Owens PL, Folk ER, Chen F. Previous strabismus surgery and eye position under anesthesia. J Pediatr Ophthalmol Strabismus. 1979; 16:313–316.

2. Lim ST, Kim SJ, Park YG. A clinical study: change of the eye position under general anesthesia. J Korean Ophthalmol Soc. 1995; 36:2243–2251.
3. Lee DS, Kim SY. Eye position of orthophoric patients under general anesthesia. J Korean Ophthalmol Soc. 2001; 42:1303–1308.
4. Ku HC, Lee SY, Lee YC. Change of eye position in patients with orthophoria and horizontal strabismus under general anesthesia. Korean J Ophthalmol. 2005; 19:55–61.

5. Lee SY, Seong GJ, Kim HB. Eye position of strabismus patients under general anesthesia. J Korean Ophthalmol Soc. 1987; 28:117–120.
6. Kim SJ, Oh JS, Kim JM. A study of the change in angle deviation under general anesthesia in horizontal strabismus patients. J Korean Ophthalmol Soc. 1989; 30:115–122.
7. An GJ, Cho YA, Jung HR. The change of the squint angle under general anesthesia using pancronium bromide (Myoblock [R]). J Korean Ophthalmol Soc. 1989; 30:773–778.
8. Apt L, Isenberg S. Eye position of strabismus patients under general anesthesia. Am J Ophthalmol. 1977; 84:574–579.

9. Romano PE, Gabriel L, Bennett WL, Snyder BM. Stage I intraoperative adjustment of eye muscle surgery under general anesthesia: consideration of graduated adjustment. Graefes Arch Clin Exp Ophthalmol. 1988; 226:235–240.

10. Ruy JW, Lee SY, Lee YC. Change of eye position after strabismus surgery under general anesthesia. J Korean Ophthalmol Soc. 2006; 47:1798–1803.
11. Mindel JS, Raab EL, Eisenkraft JB, Teutsch G. Succinyldicholine-induced return of the eyes to the basic deviation: a motion picture study. Ophthalmology. 1980; 87:1288–1295.
12. Yoon KC, Mun GH, Kim SD, et al. Prevalence of eye diseases in South Korea: data from the Korea National Health and Nutrition Examination Survey 2008–2009. Korean J Ophthalmol. 2011; 25:421–433.

13. McCall LC, Isenberg SJ, Apt L. The effect of torsional muscle dysfunction and surgery on eye position under general anesthesia. J Pediatr Ophthalmol Strabismus. 1993; 30:154–156.

14. Rhiu S, Yoon JS, Zhao SY, Lee SY. Variations in the degree of epiblepharon with changes in position and induction of general anesthesia. Graefes Arch Clin Exp Ophthalmol. 2013; 251:929–933.

15. Collins CC, Carlson MR, Scott AB, Jampolsky A. Extraocular muscle forces in normal human subjects. Invest Ophthalmol Vis Sci. 1981; 20:652–664.
16. Breinin GM. The position of rest during anesthesia and sleep; electromyographic observations. AMA Arch Ophthalmol. 1957; 57:323–326.

17. Burford GE. Involuntary eyeball motions during anesthesia and sleep relationship to cortical rhythmic potentials. Anesth Anal. 1941; 20:191–199.
18. Daien V, Turpin C, Lignereux F, et al. Determinants of ocular deviation in esotropic subjects under general anesthesia. J Pediatr Ophthalmol Strabismus. 2013; 50:155–160.

19. Oliveira CR, Bernardo WM, Nunes VM. Benefit of general anesthesia monitored by bispectral index compared with monitoring guided only by clinical parameters. Systematic review and meta-analysis. Braz J Anesthesiol. 2017; 67:72–84.

20. Porter AJ, Lee L, Bradshaw C. Bispectral index monitoring in vitrectomy surgery under local anaesthetic block with sedation: a single surgeon, single anaesthetist review. Eye (Lond). 2017; 31:1115–1116.

21. Park SW, Lee H, Ahn H. Bispectral index versus standard monitoring in sedation for endoscopic procedures: a systematic review and meta-analysis. Dig Dis Sci. 2016; 61:814–824.

22. Glass PS, Bloom M, Kearse L, et al. Bispectral analysis measures sedation and memory effects of propofol, midazolam, isoflurane, and alfentanil in healthy volunteers. Anesthesiology. 1997; 86:836–847.

23. Yang KS, Habib AS, Lu M, et al. A prospective evaluation of the incidence of adverse events in nurse-administered moderate sedation guided by sedation scores or Bispectral Index. Anesth Analg. 2014; 119:43–48.

24. Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev. 2014; CD003843.

25. Shepherd J, Jones J, Frampton G, et al. Clinical effectiveness and cost-effectiveness of depth of anaesthesia monitoring (E-Entropy, Bispectral Index and Narcotrend): a systematic review and economic evaluation. Health Technol Assess. 2013; 17:1–264.

26. Ahn SE, Ha SG, Kim SH. Esotropia surgery considering the angle under general anesthesia. Semin Ophthalmol. 2017; 32:787–792.

27. Bae HW, Chung SA, Yoon JS, Lee JB. Changes in the interpupillary distance following general anesthesia in children with intermittent exotropia: a predictor of surgical outcomes. J Pediatr Ophthalmol Strabismus. 2012; 49:49–53.

28. Barry JC, Backes A. Limbus versus pupil center for ocular alignment measurement with corneal reflexes. Invest Ophthalmol Vis Sci. 1997; 38:2597–2607.
29. Brodie SE. Photographic calibration of the Hirschberg test. Invest Ophthalmol Vis Sci. 1987; 28:736–742.
30. DeRespinis PA, Naidu E, Brodie SE. Calibration of Hirschberg test photographs under clinical conditions. Ophthalmology. 1989; 96:944–949.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download