Abstract
Purpose
Short-term results regarding the efficacy of intravitreal bevacizumab, dexamethasone implants, and triamcinolone-bevacizumab in macular edema (ME) secondary to branch retinal vein occlusion (BRVO) were compared.
Methods
This study included 30 eyes of with BRVO and ME. Patients received the following treatments: 1.25 mg of bevacizumab (group 1, n = 9), 0.7 mg of dexamethasone as an implant (group 2, n = 12), or a combination of 2 mg of triamcinolone acetonide and 1.25 mg of bevacizumab (group 3, n = 9). Measurements of visual acuity and central macular thickness (CMT) with optical coherence tomography were performed at baseline, and at 1 and 3 months injection.
Results
Compared to baseline, the CMT was significantly decreased in all groups by 326.32 ± 149.32, 311.50 ± 58.54, and 282 ± 28.21, respectively, at 1 month and 407 ± 160, 348 ± 108, and 289 ± 66, respectively, at 3 months, but there was no significant difference within each group. Compared to baseline, best-corrected visual acuity (BCVA) was significantly increased in all groups at 1 month and 3 months. Using post hoc analysis, there was no significant difference in the degrees of BCVA gain, but in degrees of CMT reduction, groups 2 and 3 were significantly higher than group 1 at 1 month and only group 3 was significantly higher than group 1 at 3 months (p < 0.017).
Conclusions
The intravitreal injection of bevacizumab, a dexamethasone implant, or a combination of triamcinolone-bevacizumab could be effectively used in the treatment of ME due to BRVO. For ME, steroid treatment showed a greater reduction percentage, and in the case of the triamcinolone-bevacizumab combination, we could cover the short half-life of bevacizumab and the complications of steroid use. In severe cases of ME, an intravitreal dexamethasone implant or a combination of triamcinolone and bevacizumab can be considered as the first-line therapy.
Figures and Tables
Figure 1
Changes of central macular thickness (CMT) after intravitreal injection. Compared with baseline, mean amount of decrease were 155.32 ± 151.12, 190.50 ± 126.51, 289.52 ± 121.83 μm in group 1, group 2, and group 3, respectively at 1 month after injection and group 2 and 3 showed greater CMT change than group 1 in post-hoc analysis (p < 0.017). Mean amount of decrease were 74.10 ± 138.61, 153.14 ± 85.62, 282.21 ± 145.90 μm in group 1, group 2, and group 3, respectively at 3 months after injection and only group 3 showed greater CMT change than group 1 in post-hoc analysis (p < 0.017).

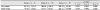
Table 2
Alteration of best-corrected visual acuity (BCVA), central macular thickness (CMT), and intra-ocular pressure (IOP)

References
1. Hayreh SS. Prevalent misconceptions about acute retinal vascular occlusive disorders. Prog Retin Eye Res. 2005; 24:493–519.

2. Hayreh SS, Rojas P, Podhajsky P, et al. Ocular neovascularization with retinal vascular occlusion-III. Incidence of ocular neovascularization with retinal vein occlusion. Ophthalmology. 1983; 90:488–506.
3. Argon laser. The Branch Vein Occlusion Study Group. Am J Ophthalmol. 1984; 98:271–282.
4. Campochiaro PA, Hafiz G, Shah SM, et al. Ranibizumab for macular edema due to retinal vein occlusions: implication of VEGF as a critical stimulator. Mol Ther. 2008; 16:791–799.

5. Pe'er J, Folberg R, Itin A, et al. Vascular endothelial growth factor upregulation in human central retinal vein occlusion. Ophthalmology. 1998; 105:412–416.
6. Campochiaro PA, Brown DM, Awh CC, et al. Sustained benefits from ranibizumab for macular edema following central retinal vein occlusion: twelve-month outcomes of a phase III study. Ophthalmology. 2011; 118:2041–2049.

7. Antonetti DA, Barber AJ, Hollinger LA, et al. Vascular endothelial growth factor induces rapid phosphorylation of tight junction proteins occludin and zonula occluden 1. A potential mechanism for vascular permeability in diabetic retinopathy and tumors. J Biol Chem. 1999; 274:23463–23467.
8. Suzuki Y, Nakazawa M, Suzuki K, et al. Expression profiles of cytokines and chemokines in vitreous fluid in diabetic retinopathy and central retinal vein occlusion. Jpn J Ophthalmol. 2011; 55:256–263.

9. Kim TH, Yoon CH, Lee JE, et al. One-year outcome of intravitreal dexamethasone implant for macular edema secondary to central retinal vein occlusion. J Korean Ophthalmol Soc. 2016; 57:1918–1925.

10. Ehrlich R, Ciulla TA, Moss AM, Harris A. Combined treatment of intravitreal bevacizumab and intravitreal triamcinolone in patients with retinal vein occlusion: 6 months of follow-up. Graefes Arch Clin Exp Ophthalmol. 2010; 248:375–380.

11. Chang-Lin JE, Attar M, Acheampong AA, et al. Pharmacokinetics and pharmacodynamics of a sustained-release dexamethasone intravitreal implant. Invest Ophthalmol Vis Sci. 2011; 52:80–86.

12. Greenberger S, Boscolo E, Adini I, et al. Corticosteroid suppression of VEGF-A in infantile hemangioma-derived stem cells. N Engl J Med. 2010; 362:1005–1013.

13. Saraiya NV, Goldstein DA. Dexamethasone for ocular inflammation. Expert Opin Pharmacother. 2011; 12:1127–1131.

14. Kaldirim HE, Yazgan S. A comparison of three different intravitreal treatment modalities of macular edema due to branch retinal vein occlusion. Int Ophthalmol. 2018; 38:1549–1558.

15. Son BK, Kwak HW, Kim ES, Yu SY. Comparison of ranibizumab and bevacizumab for macular edema associated with branch retinal vein occlusion. Korean J Ophthalmol. 2017; 31:209–216.

16. Krohne TU, Eter N, Holz FG, Meyer CH. Intraocular pharmacokinetics of bevacizumab after a single intravitreal injection in humans. Am J Ophthalmol. 2008; 146:508–512.

17. Stewart MW. Predicted biologic activity of intravitreal bevacizumab. Retina. 2007; 27:1196–1200.

18. Beer PM, Bakri SJ, Singh RJ, et al. Intraocular concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injection. Ophthalmology. 2003; 110:681–686.

19. Haller JA, Bandello F, Belfort R Jr, et al. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion twelve-month study results. Ophthalmology. 2011; 118:2453–2460.
20. Yang HN, Kim YJ, Kim JC, Shyn KH. Clinical evaluation for branch retinal vein occlusion. J Korean Ophthalmol Soc. 1992; 33:599–604.
21. Campochiaro PA, Bhisitkul RB, Shapiro H, Rubio RG. Vascular endothelial growth factor promotes progressive retinal nonperfusion in patients with retinal vein occlusion. Ophthalmology. 2013; 120:795–802.

22. Park SP, Ahn JK, Mun GH. Aqueous vascular endothelial growth factor levels are associated with serous macular detachment secondary to branch retinal vein occlusion. Retina. 2010; 30:281–286.

23. Brown DM, Campochiaro PA, Singh RP, et al. Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010; 117:1124–1133.e1.
24. Campochiaro PA, Heier JS, Feiner L, et al. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010; 117:1102–1112.e1.
25. Bakri SJ, Snyder MR, Reid JM, et al. Pharmacokinetics of intravitreal bevacizumab (Avastin). Ophthalmology. 2007; 114:855–859.

26. Epstein DL, Algvere PV, von Wendt G, et al. Benefit from bevacizumab for macular edema in central retinal vein occlusion: twelve-month results of a prospective, randomized study. Ophthalmology. 2012; 119:2587–2591.

27. Kang KT, Kim YC, Kim KS. Factors related to repeatability of intravitreal bevacizumab injections in branch retinal vein occlusion macular edema. J Korean Ophthalmol Soc. 2015; 56:1580–1585.

28. Koss MJ, Naser H, Sener A, et al. Combination therapy in diabetic macular oedema and retinal vein occlusion--past and present. Acta Ophthalmol. 2012; 90:580–589.
29. Ahn HM, Choi KS. Short-term Effectiveness of Intravitreal Triamcinolone Injection for Refractory Macular Edema Secondary to Branch Retinal Vein Occlusion. J Korean Ophthalmol Soc. 2016; 57:1731–1737.

30. Sohn HJ, Han DH, Lee DY, Nam DH. Changes in aqueous cytokines after intravitreal triamcinolone versus bevacizumab for macular oedema in branch retinal vein occlusion. Acta Ophthalmol. 2014; 92:e217–e224.

31. Guthoff R, Meigen T, Hennemann K, Schrader W. Comparison of bevacizumab and triamcinolone for treatment of macular edema secondary to branch retinal vein occlusion in a pair-matched analysis. Ophthalmologica. 2010; 224:319–324.

32. Tao Y, Hou J, Jiang YR, et al. Intravitreal bevacizumab vs triamcinolone acetonide for macular oedema due to central retinal vein occlusion. Eye (Lond). 2010; 24:810–815.

33. Yepremyan M, Wertz FD, Tivnan T, et al. Early treatment of cystoid macular edema secondary to branch retinal vein occlusion with intravitreal triamcinolone acetonide. Ophthalmic Surg Lasers Imaging. 2005; 36:30–36.

34. Haller JA, Bandello F, Belfort R Jr, et al. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010; 117:1134–1146.

35. Moon SY, Cho KH, Woo SJ, et al. Bevacizumab versus dexamethasone implant followed by bevacizumab for the treatment of macula edema associated with branch retinal vein occlusion. Korean J Ophthalmol. 2018; 32:29–37.

36. Laine I, Lindholm JM, Ylinen P, Tuuminen R. Intravitreal bevacizumab injections versus dexamethasone implant for treatment-naïve retinal vein occlusion related macular edema. Clin Ophthalmol. 2017; 11:2107–2112.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download